On this page
The Four Stages of COPD at a Glance: Mild, Moderate, Severe, Very Severe
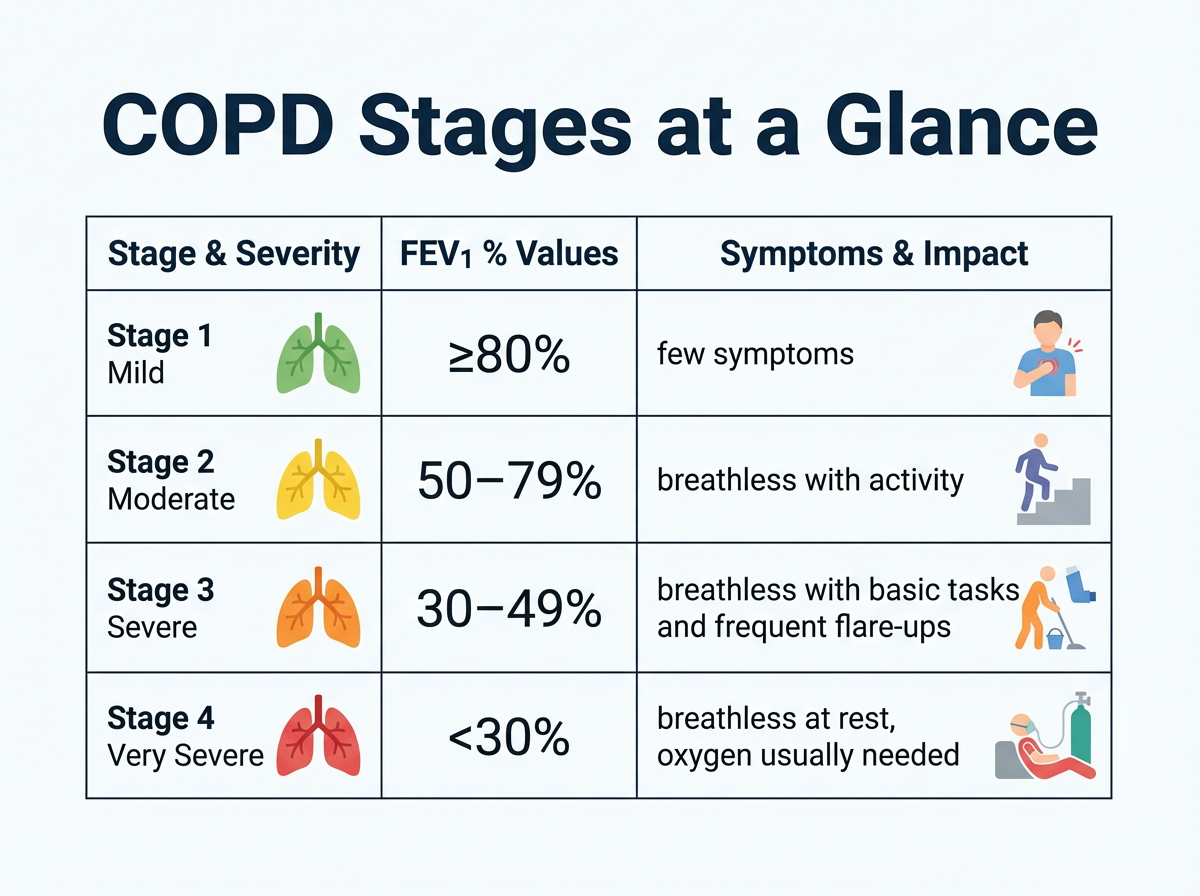
Here’s the simple answer. Doctors sort COPD into four stages based on how much air you can blow out in one second on a breathing test (FEV1).
- Stage 1 Mild: FEV1 is 80% or more of normal. Symptoms can be easy to miss.
- Stage 2 Moderate: FEV1 is 50% to 79% of normal. Shortness of breath shows up with daily activity.
- Stage 3 Severe: FEV1 is 30% to 49% of normal. Breathlessness limits basic tasks and flare-ups are common.
- Stage 4 Very Severe: FEV1 is under 30% of normal, or under 50% with signs of respiratory failure. Breathlessness at rest is common and oxygen is usually needed.
These cutoffs use your FEV1 after you’ve used a bronchodilator on a spirometry test. Stages show lung function, but symptoms and flare-ups also matter.
Quick reference chart: COPD stages are set by post-bronchodilator FEV1. Higher stages mean lower lung function.
| Stage | Name | FEV1 % predicted | Everyday cue |
|---|---|---|---|
| 1 | Mild | ≥80% | Few or no symptoms |
| 2 | Moderate | 50–79% | Breathless with activity |
| 3 | Severe | 30–49% | Breathless with basic tasks; frequent flare-ups |
| 4 | Very Severe | <30% or <50% with respiratory failure | Breathless at rest; oxygen usually needed |
* Respiratory failure means low blood oxygen or high carbon dioxide that continues despite treatment.
Key Takeaway: The four COPD stages run from Mild (FEV1 ≥80%) to Very Severe (FEV1 <30%).
COPD Staging with Spirometry and GOLD Criteria
Doctors use a breathing test called spirometry. You take a deep breath in and blow out hard into a device. It measures FEV1 (air blown out in one second) and FVC (total air blown out). COPD is confirmed when the FEV1/FVC ratio stays below 0.70 after using a bronchodilator.
FEV1 percent predicted compares your result to what’s expected for a healthy person of your age, sex, and height.
GOLD (Global Initiative for Chronic Obstructive Lung Disease) uses your post-bronchodilator FEV1 percent predicted to grade severity:
- Stage 1 Mild: ≥80%
- Stage 2 Moderate: 50–79%
- Stage 3 Severe: 30–49%
- Stage 4 Very Severe: <30%
These numbers help match treatment to need and track changes over time. Today’s care also considers your symptom scores and exacerbation history, not just spirometry.
Key Takeaway: COPD stage comes from a spirometry lung test, especially your FEV1 percent predicted after using a bronchodilator.
GOLD 2024 Groups A, B, and E Explained
Numbers don’t tell the whole story. GOLD 2024 also sorts people by symptoms and flare-up risk to guide care:
- Group A: Low symptoms and low risk of exacerbations (0–1 mild flare in the past year).
- Group B: High symptoms but low risk of exacerbations.
- Group E: Higher risk of exacerbations (2 or more in a year, or any flare needing a hospital visit).
Doctors use simple tools like the COPD Assessment Test (CAT) and the mMRC breathlessness scale (a simple 0–4 breathlessness score) to score symptoms. A hospitalization for an exacerbation places you in Group E even if you had only one flare.
Earlier GOLD guidelines used Groups A–D; in 2024, C and D were combined into Group E for people at higher risk of exacerbations.
Key Takeaway: Groups A, B, and E capture symptom burden and flare-up risk so treatment fits real life, not just lung numbers.
Stage 1: Mild COPD
What it means: FEV1 is 80% or more of normal (also called GOLD 1).
How it can feel: You can do most activities. A chronic or “smoker’s” cough might be the only clue. Shortness of breath sometimes shows up only with hard exercise.
Care basics: Your doctor can prescribe a rescue inhaler for you to use when symptoms flare. Quit smoking and avoid secondhand smoke and pollution. Get flu and pneumonia vaccines. Your doctor can order baseline spirometry and help you create a simple activity plan to stay active. Even in Stage 1, COPD has already started to damage your lungs, even if you feel mostly normal.
When to call your doctor: A chronic cough, more mucus, or new breathing issues deserve a checkup.
Key Takeaway: Mild COPD can feel normal, but it’s the best time to quit smoking and stay vaccinated.
Stage 2: Moderate COPD
What it means: FEV1 is 50% to 79% of normal (also called GOLD 2). Lots of people first notice a problem here.
How it can feel: You might need to pause on stairs or hills. Cough, mucus, wheeze, and fatigue are more common. Sleep can be harder.
Care basics: Doctors typically start daily long-acting bronchodilators at this stage. Pulmonary rehab teaches breathing skills and safe exercise. Pursed-lip breathing can ease breathlessness. Some people add nebulized medicines if inhalers alone aren’t enough. A portable mesh nebulizer, such as the TruNeb™ portable mesh nebulizer, can deliver a fine mist of prescribed bronchodilators or saline at home or on the go. Ask your doctor if it fits your plan.
Safety note: Talk to your doctor before trying a new medication or changing your COPD treatment.
When to call your doctor: If you’re stopping more during daily tasks, cough gets worse, or mucus changes color (thick green or yellow) or wheezing increases, your plan might need an update.
Key Takeaway: In Stage 2, daily inhalers, rehab, and better breathing habits can ease symptoms and reduce COPD flare-ups.
Stage 3: Severe COPD
What it means: FEV1 is 30% to 49% of normal (also called GOLD 3). Airflow is tight and symptoms are hard to ignore.
How it can feel: Breathlessness shows up with simple tasks like dressing or showering. Flare-ups are more frequent and can require ER or hospital care. Fatigue is common. Some people notice morning headaches or ankle swelling from extra strain on the heart.
Care basics: Most people use a combination of long-acting bronchodilators and an inhaled corticosteroid. Your doctor can prescribe oxygen if your levels run low (sometimes only with sleep or activity at first). Not everyone in Stage 3 needs oxygen. It depends on your blood oxygen levels. A written COPD action plan explains when to start rescue medicines during a flare, based on your doctor’s instructions. A lot of people also use a nebulizer for daily treatments because a slow mist is easier to inhale; a portable device like TruNeb can help deliver prescribed bronchodilators or saline and make it easier to loosen mucus.
When to call your doctor: Any sudden increase in shortness of breath, fever, or darker mucus needs quick attention. ⚠️ If you’re so short of breath that you can’t speak in full sentences, have chest pain, or notice blue lips or fingertips, seek emergency medical care (call 911 or your local emergency number).
Key Takeaway: Stage 3 COPD usually requires multiple inhalers, a written flare-up action plan, and sometimes oxygen to stay stable.
Stage 4: Very Severe (End‑Stage) COPD and Palliative Care
What it means: FEV1 is under 30% of normal, or under 50% with signs of respiratory failure (also called GOLD 4). This is sometimes called end-stage COPD.
How it can feel: Breathlessness at rest. Only a few steps can require a break. Weight and muscle loss are common. Anxiety or low mood can appear because breathing is so hard.
Care basics: A lot of people need oxygen most of the day. Treatments usually include bronchodilators, inhaled steroids, and other medicines to ease symptoms. Noninvasive ventilation like BiPAP at night can help rest breathing muscles.
Advanced options: Some people are evaluated for lung volume reduction or transplant. These surgeries are options for a small number of people who meet strict criteria (age, overall health, and smoking status matter).
Palliative support: Adding palliative care (and hospice when appropriate) focuses on comfort, anxiety control, and daily support at home. It’s not giving up—it’s getting more help to live with fewer symptoms and more peace. Palliative care can be added while you continue some disease-directed treatment; hospice is usually for advanced Stage 4 when life expectancy is limited and the focus is comfort.
When to call your doctor: Infection signs (fever, thicker or darker mucus), new confusion, or extreme sleepiness need urgent care. ⚠️ These can be signs of a life-threatening COPD flare or low oxygen. Call 911 or your local emergency number right away.
Key Takeaway: Stage 4 shifts focus to comfort, strong support, and preventing crises while treating symptoms.

COPD Stages and Life Expectancy
COPD gets more serious as stage rises, but life expectancy still varies a lot. Age, smoking status, heart disease, weight, activity level, and flare-ups all matter. Smoking is the main cause of COPD, but inherited conditions such as alpha‑1 antitrypsin deficiency can cause COPD even in nonsmokers.
- Stages 1–2: A lot of people live close to normal lifespans, especially if they quit smoking and stay on treatment.
- Stage 3: Survival drops, but good care and fewer exacerbations help.
- Stage 4: Studies usually report average survival around 2–5 years after reaching very severe disease, though some live longer with excellent care.
Doctors sometimes use the BODE index (body mass, airflow obstruction, dyspnea, exercise) to estimate risk more accurately than stage alone. A higher BODE score means higher risk. Doctors use it to identify people who need closer follow-up. Different studies report different ranges because they look at different patient groups and time periods. Whatever your stage, quitting smoking, staying active, getting vaccines, and treating flares fast can improve outcomes.
Note: Prognosis numbers are averages, not a personal prediction. Your doctor can put your test results and history in context.
Key Takeaway: Higher stage raises risk, but quitting smoking and steady care can shift the odds in your favor.
Living with COPD at Every Stage
Small, steady steps add up:
- Stay Active: Gentle walking or home exercises keep muscles strong. Use oxygen if prescribed.
- Breathing Skills: Pursed-lip and diaphragmatic breathing help you recover faster after activity.
- Take Meds as Directed: Daily inhalers work best when used every day with good technique.
- Avoid Triggers: Skip smoke, dusty air, extreme cold, and avoid sick contacts. Wash your hands regularly.
- Vaccines and Checkups: Flu, pneumonia, and COVID-19 shots reduce severe illness. Keep routine visits.
- Support: Pulmonary rehab, support groups, and counseling can ease stress and teach practical tricks.
- Plan for Flares: Ask your doctor about a written COPD action plan so you know what to do when symptoms spike.
- Helpful Tools: If your doctor recommends it, a portable nebulizer can make treatments easier at home and on the go.
Safety note: Talk to your doctor before starting new medicines, changing doses, or trying hypertonic saline.
⚠️ If your symptoms suddenly get much worse than usual and your rescue medicines don’t help, don’t wait; call your doctor or emergency services.
⚠️ Don’t use someone else’s inhaler or medicines. Only use treatments prescribed for you.
Key Takeaway: Good daily habits, vaccines, and rehab help you breathe easier and avoid setbacks at any stage.
FAQs About COPD Stages
Tap or click a question below to see the answer:
By spirometry. You blow into a device that measures your FEV1 and FVC. Your stage comes from your FEV1 percent predicted after using a bronchodilator. Lower FEV1 means a higher (more severe) stage.
COPD lung damage is usually permanent, so stages rarely move down. The good news: symptoms and flare-ups can improve with treatment, and progression can slow a lot when you quit smoking and follow your plan.
No. Progression varies widely. Quitting smoking, staying active, getting vaccines, and using prescribed treatments can slow or even halt progression for some people, and not everyone reaches Stage 4.
Yes. Stage 4 is also called end-stage COPD. It signals very limited airflow and high symptom burden. Care focuses on comfort, safety, and strong support, including palliative care or hospice when appropriate.
Stage 2 (FEV1 50–79%) causes breathlessness with everyday activity. Stage 3 (FEV1 30–49%) limits basic tasks, brings more frequent exacerbations, and can require oxygen or more intensive therapy.
No. Oxygen is prescribed when blood oxygen is low, more commonly in Stage 3 or 4. Your doctor will check levels at rest, during sleep, and with activity to decide.
Palliative care can start at any stage to help with symptoms, anxiety, and planning. Hospice is usually considered in advanced Stage 4 when life expectancy is limited and the focus shifts to comfort at home.
They describe symptoms and flare-up risk. A is low symptoms/low risk, B is high symptoms/low risk, and E is higher risk of exacerbations (especially with 2+ flares or any hospitalization). Your stage plus your group helps tailor your treatment plan.
Key Takeaway: Spirometry sets your COPD stage; groups A, B, and E guide treatment by symptoms and flare-up risk.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms, test results, and treatment options.