On this page
Normal Oxygen Levels During Sleep
For most healthy adults at sea level, normal oxygen levels during sleep (SpO₂) stay around 95–100%, similar to when you're awake. A small dip of a few points can happen in deep sleep or REM, but your level should stay well above 90%.
If you live at high altitude or have a lung condition like COPD or asthma, your usual range can run a bit lower. Ask your doctor what target range is right for you.
Key take: Most healthy sleepers stay near 95–100% at night with only small dips.
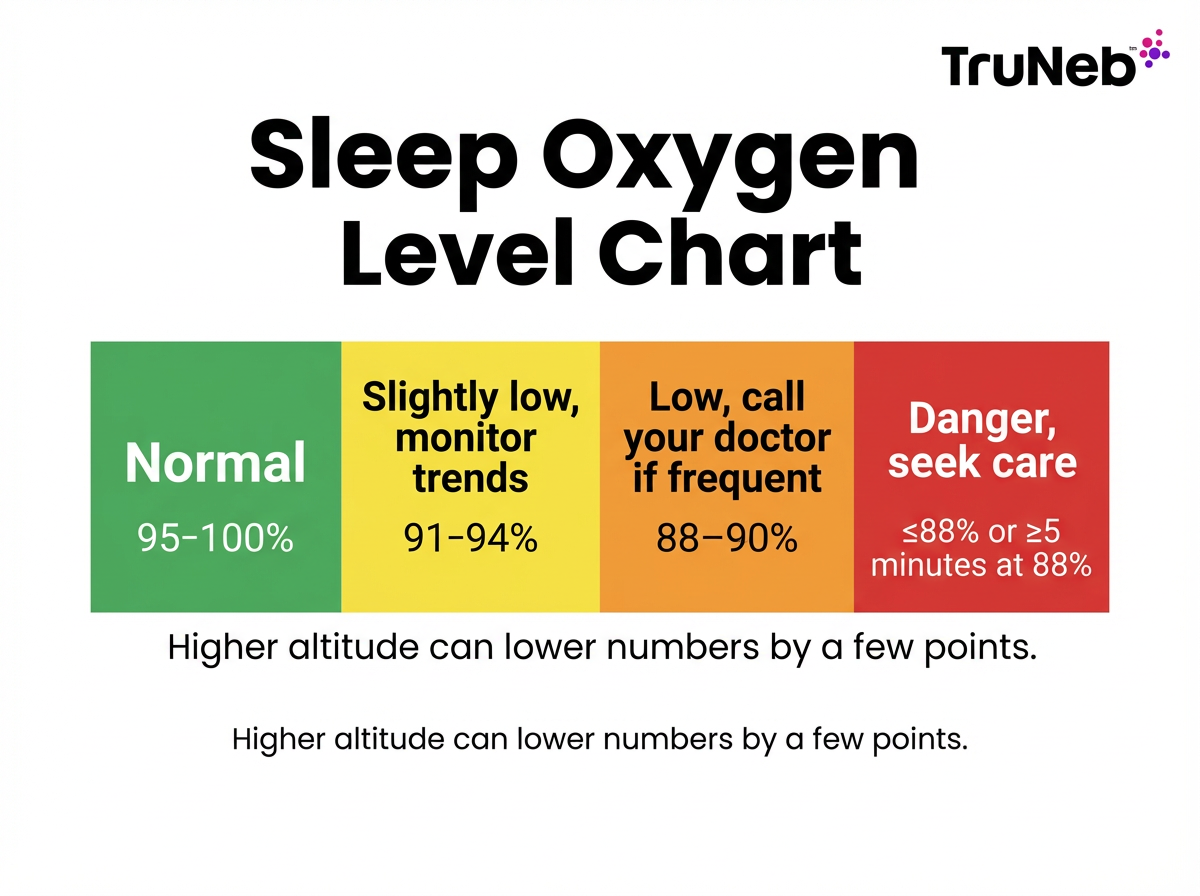
Oxygen Saturation Ranges at Night: Normal vs Low
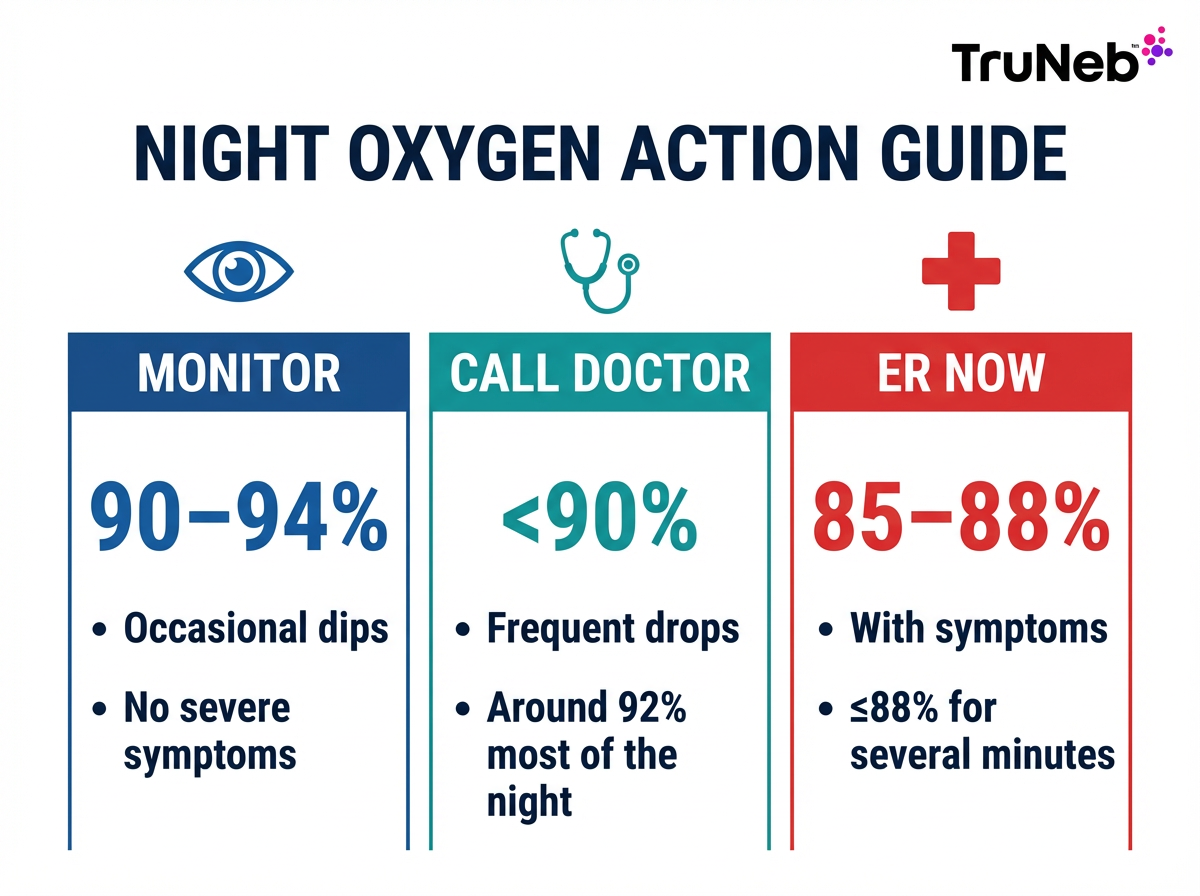
Here is a quick chart to interpret your number and choose next steps.
Sleep apnea oxygen level chart: Use your overnight SpO₂ to decide when to watch, call your doctor, or seek urgent care.
| Overnight SpO₂ | What it means | What to do |
|---|---|---|
| 95–100% | Normal | Keep your routine; monitor as needed |
| 91–94% | Slightly low | Watch trends over several nights |
| 88–90% | Low | Talk to your doctor if this is frequent or lasts more than brief moments |
| ≤88% or 5+ minutes at 88% | Dangerous (nocturnal hypoxemia) | Seek prompt medical care |
* If you have a chronic lung condition like COPD, your doctor might set a different "normal" range for you.
Think of this as a simple sleep apnea oxygen level chart that maps your overnight SpO₂ range to an action. Here's a simple color-coded sleep oxygen level chart you can reference at a glance.
Example: An 87% reading is below normal. One brief dip can be sensor artifact, but repeated dips to 87% or lower are a red flag for a breathing issue like obstructive sleep apnea or another cause of nocturnal hypoxemia.
Key take: Sustained 88% or lower at night is dangerously low and needs prompt care.
Why Oxygen Levels Can Drop at Night: Causes
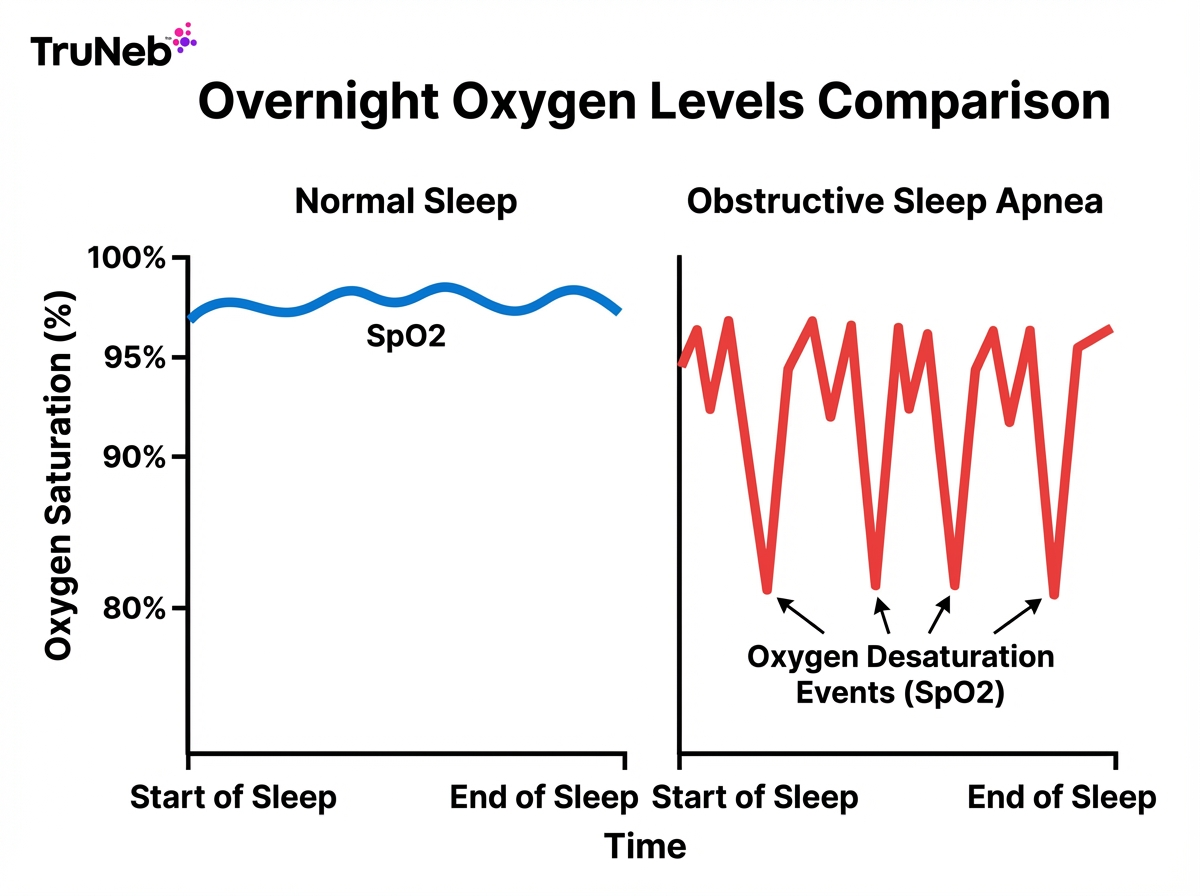
Small drops can be a normal part of sleep. Bigger or longer drops usually point to a fixable cause. These drops are oxygen desaturation events (drops in SpO₂).
- Obstructive sleep apnea: The airway collapses for 10–30 seconds, causing sharp oxygen dips and brief arousals.
- Central sleep apnea or hypoventilation (including obesity hypoventilation syndrome): Weak breathing signals lead to shallow breaths and lower oxygen.
- COPD or asthma: Damaged or inflamed airways move less air, so oxygen falls more at night.
- Heart failure: Weak pumping reduces oxygen delivery to the body.
- Obesity and back sleeping: Extra weight on the chest and tongue can narrow the airway.
- High altitude: Thinner air means lower saturation for many people.
- Respiratory infections or congestion: Swelling and mucus block airflow, such as a bad cold, flu, or pneumonia.
- Alcohol or sedatives: Relax breathing muscles and can worsen apnea.
Key take: Obstructive sleep apnea is the most common reason for big overnight oxygen drops.
Signs and Symptoms of Low Oxygen During Sleep
Watch for these clues:
- Loud snoring with pauses, gasping, or choking awakenings
- Morning headache or dry mouth
- Excess daytime sleepiness or brain fog
- Waking often or restless sleep
- Shortness of breath at night
- Waking with high blood pressure or a fast or irregular heartbeat
- Blue-tinged lips or fingertips in severe cases
If these show up along with low readings, talk to your doctor.
Key take: Gasping, morning headaches, and heavy sleepiness are classic clues of low night oxygen.
When to Worry: Seeking Medical Help for Low Oxygen
Here's how to tell when to worry:
- Often below about 92–93% at night across multiple nights: Schedule a visit with your doctor.
- Repeated dips below 90% (not just one quick blip): Get evaluated soon for sleep apnea or lung disease.
- 88% or lower, especially for several minutes: This is dangerous. Seek prompt care.
- Any low reading plus severe symptoms like trouble breathing, chest pain, confusion, or blue lips: Go to the ER now.
If you already use oxygen or have COPD, follow the thresholds your doctor gave you. When in doubt, get checked.
Key take: Below 90% often means call your doctor; around 85–88% with symptoms is an ER visit.
⚠️ If your oxygen stays at 88% or lower for several minutes, or you have severe symptoms like chest pain, trouble breathing, or confusion, seek emergency medical care right away.
How to Improve Your Oxygen Levels While Sleeping
These steps can help increase your oxygen levels while sleeping and support better oxygen at night, but they don't replace seeing a doctor about ongoing low readings. Focus on what's causing the low oxygen and make breathing easier:
- Treat sleep apnea: Use CPAP as prescribed to keep the airway open and prevent drops.
- Side sleeping and head elevation: These positions help keep the airway clear.
- Skip alcohol and sedatives before bed: They relax airway muscles and can worsen drops.
- Manage weight: Even modest weight loss can improve oxygen at night.
- Clear airways before bed: If you have COPD or asthma and your doctor has prescribed nebulizer treatments, using them before bed can help open airways and reduce mucus for some people.
- Humidify and decongest: A humidifier and nose care (saline rinse or strips) can ease airflow.
- Stay active: Regular exercise and breathing practice strengthen your lungs over time.
- Supplemental oxygen if prescribed: Some people need night oxygen from a concentrator via nasal cannula after testing.
- Follow up: Share your readings and symptoms with your doctor to fine-tune care.
Safety note: Talk to your doctor before trying a new medication or starting oxygen therapy. Only start or change treatments under your doctor's guidance.
Key take: Treat the cause, adjust your sleep position, and use prescribed tools to keep oxygen safer at night.
Monitoring Nighttime Oxygen: Oximeters and How to Read Your Results
Here's how to get reliable readings and make sense of them:
- Device choice: Fingertip pulse oximeters are good for spot checks; some record overnight. Rings and watches are convenient but can be less precise than a medical-grade fingertip pulse oximeter, especially during sleep.
- Good technique: Warm hands, a snug sensor, and less movement improve accuracy.
- Read trends, not blips: A single quick dip is sometimes just artifact. Look at time spent below 90%.
- Know the limits: Motion, cold fingers, nail polish, darker skin tone, or poor circulation can skew readings.
- Confirm with testing: If lows are frequent or you have symptoms, ask for overnight oximetry or a sleep study.
When you're thinking about pulse oximeter accuracy during sleep, focus on trends and duration, not a single low blip. If you see an isolated low reading but feel fine, recheck with a warm, still hand before assuming it's a true drop.
Home pulse oximeters are screening tools, not a formal diagnosis. Always bring concerning patterns to your doctor rather than adjusting treatment on your own.
⚠️ If your oxygen reading is very low (around the mid-80s or lower) and you feel short of breath, dizzy, or confused, don't wait on more readings—get emergency care.
Key take: Trust patterns and duration, not one low blip on your pulse oximeter.
Frequently Asked Questions
These quick answers cover the most common questions about normal and low oxygen levels during sleep. Tap or click a question below to see the answer:
For most healthy adults, 95–100% is typical. Brief dips to 90–94% can be okay if they pass quickly. Levels that stay below 90% need a doctor\u0019s review, and 88% or lower for several minutes is dangerous.
In healthy sleepers, oxygen stays close to daytime levels, usually in the mid to high 90s. Small dips can happen in deep sleep. Bigger or frequent drops point to a problem like sleep apnea, COPD, or another cause.
Yes. 87% falls in the low range on the sleep oxygen chart. One brief dip can be artifact, but repeated readings this low should be checked by a doctor.
Go now if you\u0019re 85–88% with severe symptoms (trouble breathing, chest pain, confusion) or you stay at 88% or lower for several minutes. For repeated dips below 90% without severe symptoms, call your doctor soon.
If you have sleep apnea, using CPAP as your doctor prescribed can prevent drops. Sleep on your side or raise your head, avoid alcohol near bedtime, and use prescribed therapies like supplemental oxygen or inhaled medications only under your doctor\u0019s guidance.
They\u0019re useful for trends, but motion, cold hands, nail polish, darker skin tone, and poor circulation can affect readings. For pulse oximeter accuracy during sleep, trust patterns over single dips and confirm concerns with a formal test.
No. Sleep apnea is common, but COPD, heart failure, high altitude, and infections can also lower oxygen. A medical visit can sort this out.
A nebulizer can deliver medicine that opens airways, which can support better oxygen for some people with asthma or COPD when prescribed by a doctor. A portable nebulizer like TruNeb can be part of a plan your doctor sets; only start or change treatments under your doctor\u0019s guidance.
Key take: These FAQs give quick, plain-language answers so you can see whether your night oxygen numbers and symptoms fall in a safe range or need a doctor\u0019s review.
Medical disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk to your doctor about your health, your oxygen readings, and any changes to your medications or treatment plan.