On this page

RSV vs Whooping Cough: Key Differences at a Glance
No, RSV and whooping cough are not the same illness. RSV is a virus. Whooping cough, also called pertussis, is a bacterial infection of the airways.
Key takeaway: RSV is caused by a virus, while whooping cough (pertussis) is caused by bacteria; this affects spread, treatment, and prevention.
| Feature | RSV | Whooping Cough |
|---|---|---|
| Cause | Virus (Respiratory Syncytial Virus) | Bacterium (Bordetella pertussis) |
| How It Spreads | Respiratory droplets and contaminated surfaces; seasonal surges | Respiratory droplets; extremely contagious without treatment |
| Typical Age Impact | Infants and young children; severe in some babies and older adults | All ages, but most dangerous for young or unvaccinated infants |
| Cough Sound | Wet, raspy cough with possible wheeze; no classic whoop | Dry, violent coughing fits; gasping “whoop” after a fit (infants can pause breathing) |
| Other Clues | Runny/stuffy nose, mild fever, trouble feeding in babies | Vomiting after coughing, exhaustion, little or no fever in fit stage |
| Duration | Peaks around days 3–5; improves in 1–2 weeks | Weeks to months; called the “100‑day cough” |
| Complications | Bronchiolitis, pneumonia, dehydration | Apnea in infants, pneumonia, seizures; can be fatal in babies |
| Prevention | Hygiene; RSV vaccine for older adults; maternal RSV vaccine; infant antibody (nirsevimab) | DTaP/Tdap vaccines; maternal Tdap; antibiotics for exposed close contacts |
| Treatment | Supportive care; no antibiotics for viruses | Early antibiotics reduce spread and can lessen severity; stay home until a doctor says you’re no longer contagious (usually after 5 days of antibiotics) |
Key point: Viral vs bacterial means antibiotics help pertussis but not RSV.
Takeaway: RSV and pertussis are different diseases with different care and prevention.
What Is RSV (Respiratory Syncytial Virus)?
RSV, or respiratory syncytial virus, is a very common virus that infects the lungs and airways. In older kids and adults, it usually looks like a bad cold with runny nose, cough, and a low fever. In babies, RSV can lead to bronchiolitis or pneumonia. Premature infants and babies with heart or lung problems are at higher risk for severe RSV. You can see fast or hard breathing and wheezing, especially in babies. RSV spreads easily by droplets and on shared surfaces, especially in fall and winter. Nearly all children have had RSV by age two.
Takeaway: RSV is a common winter virus that can cause bronchiolitis and wheezing in infants.
What Is Whooping Cough (Pertussis)?
Whooping cough, or pertussis, is a highly contagious bacterial infection of the airways. It usually starts like a mild cold, then turns into weeks of severe coughing fits. Young children can make a high whoop when they gasp in. Vomiting after a fit is common. Some infants can turn blue or even pause breathing during spells. The cough can last for months, which is why it’s called the 100‑day cough. It is most dangerous for very young babies who aren’t fully vaccinated.
Takeaway: Pertussis is a bacterial cough illness marked by long coughing fits and sometimes a classic whoop.
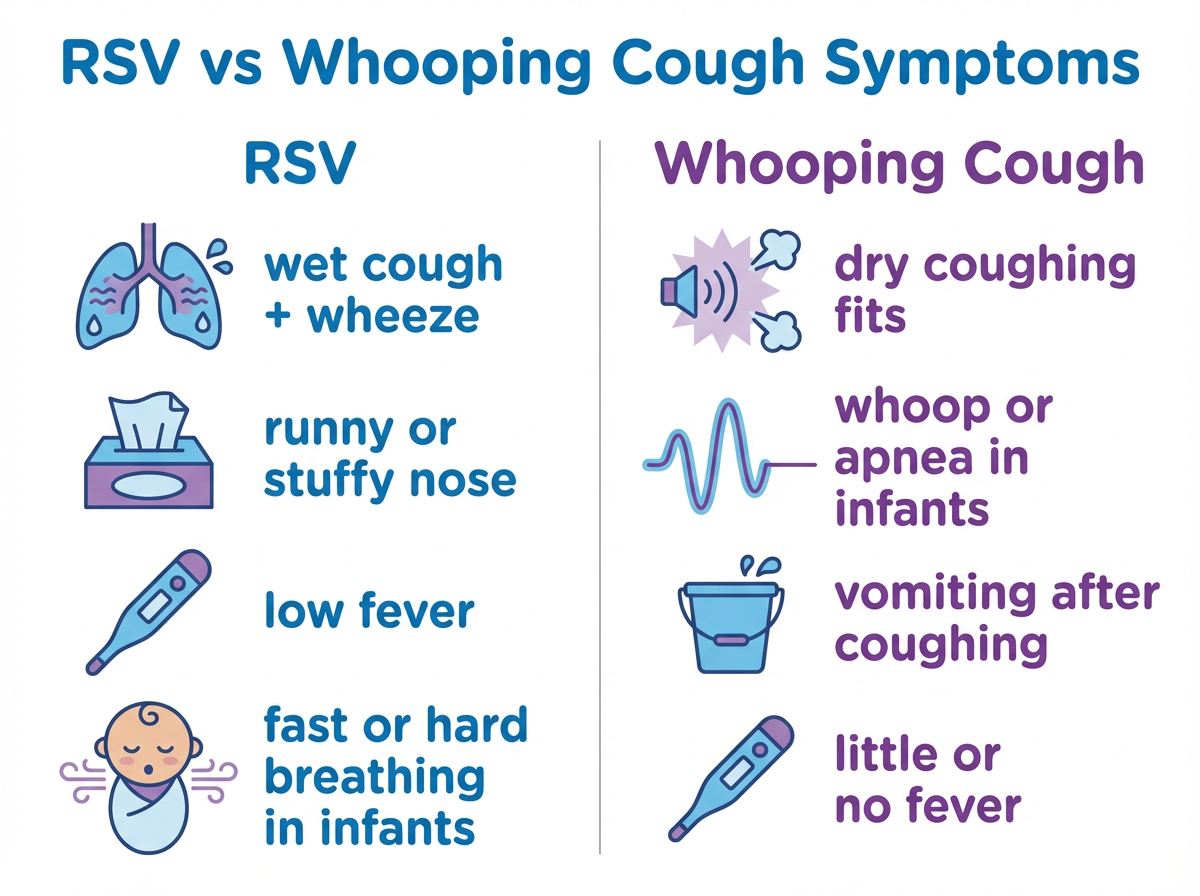
Symptoms and Signs: How to Tell Them Apart
Listen to the cough. RSV usually brings a wet, raspy cough with wheezing and lots of mucus. You’ll notice a stuffy nose and mild fever early on. Breathing can look fast or hard in babies.
Whooping cough causes dry, repeated coughing fits. The child coughs and coughs, then can gasp with a whoop or throw up after the fit. Fever is usually low or not present once the fits begin, but the cough is exhausting.
For babies, RSV usually shows up as trouble feeding, fast breathing, and chest retractions as they work to breathe. In pertussis, very young infants sometimes don’t whoop at all—some pause breathing or turn blue during spells.
In older kids and adults, RSV usually feels like a regular cold. Pertussis in teens and adults can look like a nagging cough that lasts for weeks without the classic whoop. For RSV vs whooping cough in adults, RSV usually feels short‑lived, while whooping cough tends to cause a dry cough that drags on for weeks — if your cough lasts more than 2–3 weeks, ask your doctor about pertussis testing.
Other Cough Illnesses That Can Sound Similar
- Croup: a barking, seal‑like cough with noisy breathing (stridor). It’s usually short‑lived and improves with steroid treatment and humid air.
- RSV/bronchiolitis: a wet, phlegmy cough with wheeze and lots of mucus, not a classic whoop.
- Asthma/bronchitis: a wheezy or phlegmy cough that typically improves with inhalers or over a couple of weeks, unlike the 100‑day cough of pertussis.
Takeaway: Wet wheeze points to RSV; exhausting cough fits with whoop or vomiting point to pertussis.
Causes and How RSV and Whooping Cough Spread
RSV is a virus. Whooping cough is caused by a bacterium (Bordetella pertussis). That core difference guides care: antibiotics do not treat viruses like RSV but do help bacterial pertussis, especially early.
Both spread by droplets when someone coughs or sneezes. RSV also spreads from contaminated hands and surfaces. People with RSV are usually contagious for about 3–8 days. Pertussis is extremely contagious and can spread for weeks unless treated; after 5 full days of antibiotics, people are usually no longer contagious.
Takeaway: Different germs, similar droplet spread—pertussis stays contagious longer unless treated.
Treatment and Home Care for RSV vs Whooping Cough
RSV: There’s no specific antiviral cure. Most care is supportive: manage fever, clear the nose with saline and suction, keep fluids going, and watch breathing. Severe cases can need oxygen or IV fluids in the hospital. Doctors sometimes try nebulized saline or a bronchodilator if a child is wheezing, especially if they have asthma or reactive airways. Not every child with RSV benefits from these, so doctors decide case by case.
Whooping cough: Early antibiotics (often azithromycin) help reduce spread and can lessen severity if started soon, but they don’t instantly stop the cough once it’s in the severe phase. Public health guidance and doctors usually recommend that children with whooping cough stay home until they’ve completed at least 5 full days of antibiotics so they’re no longer contagious.
Common home care steps include:
- offering small, frequent fluids and plenty of rest
- using a cool‑mist humidifier and cleaning it daily
- clearing a baby’s nose with saline and gentle suction before feeds and sleep
- holding a child upright during and after a coughing spell to help them clear mucus
Nebulizers: For doctor‑directed treatments, a portable mesh nebulizer can make breathing care easier at home or on the go. The TruNeb™ portable mesh nebulizer is quiet, handheld, and travel‑friendly, so you can give prescribed saline (for example, 3% hypertonic saline) or medicine only when your child’s doctor recommends it, and clean and dry the device after each use as directed. ⚠️ Don’t use steam inhalers or facial steamers for breathing medicines — they’re not the same as nebulizers and aren’t safe for delivering medication to the lungs. Also don’t add essential oils or over‑the‑counter cough mixtures to any nebulizer.
Safety note: Talk to your doctor before trying a new medication.
Takeaway: RSV is managed with supportive care; pertussis needs early antibiotics and isolation to limit spread.

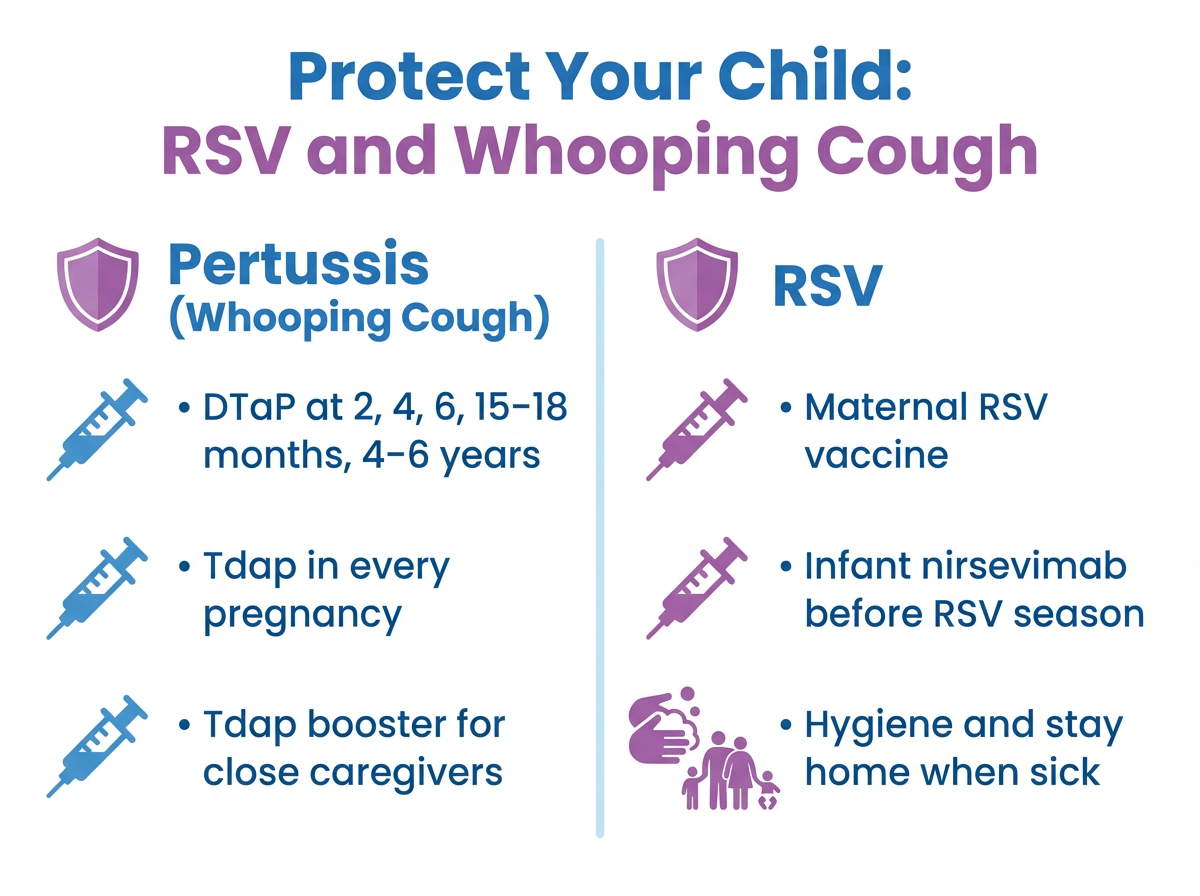
Prevention, Vaccines, and Safety Steps
Pertussis prevention: In the U.S., babies usually get DTaP shots at 2, 4, 6, 15–18 months, and 4–6 years. Preteens get a Tdap booster, and adults need boosters over time. Pregnant people should get Tdap each pregnancy to protect newborns. Check your child’s vaccine record with your doctor to confirm they’re up to date.
RSV prevention: New tools now help. There are RSV vaccines for older adults and a maternal RSV vaccine late in pregnancy to protect newborns. For infants, a long‑acting antibody (nirsevimab) before RSV season can help prevent severe disease.
These are not the same vaccines. The whooping cough vaccine (DTaP/Tdap) does not protect against RSV, and RSV vaccines/antibodies do not protect against pertussis. RSV protections are separate. Ask your pediatrician which protections your child is eligible for. Hygiene still matters: wash hands, clean toys, keep sick people away from babies, and stay home when ill.
Key point: Pertussis vaccines and RSV protections are different and work side by side.
Takeaway: DTaP/Tdap covers pertussis; maternal RSV vaccine or infant antibodies help protect against RSV.
Can You Have RSV and Whooping Cough at the Same Time?
Yes, it’s possible, though uncommon, to have RSV and whooping cough at the same time. They are different germs, so one does not protect against the other. Doctors can use nasal swab PCR tests to check for RSV, pertussis, or other germs at the same time if a baby is very ill. Co‑infection can be harder on infants and can require close monitoring in the hospital.
Takeaway: Co‑infection is rare but possible and can be severe in infants.
When to Seek Medical Help
⚠️ Recognizing emergency signs can be life‑saving.
Go to the ER or call emergency services if you see:
- Blue or gray lips or face.
- Breathing trouble: very fast breaths, pauses in breathing, grunting, or ribs pulling in with each breath.
- Unable to feed or drink, or signs of dehydration (very few wet diapers, very dry mouth, unusual sleepiness).
- Severe coughing spells in an infant, with vomiting, color change, or breathing pauses.
- High fever with worsening cough or any seizure.
For babies younger than 3 months, any significant cough or breathing trouble is a reason to contact a doctor or seek urgent care right away.
Trust your gut. This isn’t a complete list of warning signs — if anything about your child’s breathing or behavior worries you, get medical help.
Takeaway: If breathing is hard, color changes, or feeding stops, seek emergency care now.
Frequently Asked Questions About RSV vs Whooping Cough
Takeaway: These quick answers clear up the most common questions about RSV vs whooping cough, vaccines, and co‑infection.
Tap or click a question below to see the answer:
No. RSV is a virus, and whooping cough (pertussis) is a bacterium. They need different care and prevention.
No. DTaP/Tdap protects against pertussis. RSV protection is separate (maternal RSV vaccine and infant antibodies like nirsevimab).
In adults, RSV usually feels like a short cold with congestion and cough. Whooping cough often shows up as a nagging dry cough that lasts for weeks and can cause choking or vomiting. If you’ve had a cough for more than 2–3 weeks, talk with your doctor.
No. RSV usually causes a wet, wheezy cough. The classic whoop happens with pertussis after a long coughing fit.
It’s rare but possible. A very sick infant is usually tested for both so the care plan fits what’s really going on.
Both can be serious. Pertussis can be deadly in young infants if unvaccinated, and RSV leads to thousands of infant hospital stays each year.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms, questions, or before changing any treatment.