On this page

What Is Nocturnal Asthma and Why Symptoms Get Worse at Night?
Nocturnal asthma means your asthma flares at night. You can cough, wheeze, or feel chest tightness while trying to sleep.
Here’s why nights are harder:
- Your body clock (circadian rhythm) lowers cortisol overnight. Lung function tends to dip around 4 a.m.
- Lying flat lets postnasal drip and acid reflux irritate your airways.
- Cool, dry night air can tighten the bronchial tubes.
- You spend hours close to bedroom allergens like dust mites and pet dander.
If your evening controller medicine wears off before dawn, you might wake up coughing. Frequent night waking is a sign your asthma isn’t well controlled.
One-liner: Nocturnal asthma coughs often happen because your body clock, lying flat, cool night air, and bedroom allergens all make your airways tighter while you sleep.
How to Calm an Asthma Cough at Night (Step-by-Step)
If you’re coughing right now, use these steps to settle your breathing.
⚠️ If you’re too breathless to speak in full sentences, your lips or face look blue, or you feel faint or confused, call emergency services immediately instead of trying home steps.
- Sit up straight. Loosen tight clothing. Staying upright opens your airways.
- If your doctor has given you a quick-relief inhaler, follow your asthma action plan to use it at the first sign of symptoms. Using a spacer (if you have one) and taking slow, deep breaths helps the medicine reach your lungs.
- Breathe slowly with pursed lips. Inhale through your nose, then exhale longer through pursed lips, like blowing out a candle.
- Sip warm water or tea. If appropriate, a small spoon of honey can soothe your throat. These comfort steps do not replace asthma medicine.
- Remove triggers. Move away from smoke, strong odors, or cold air. Turn off a dusty fan.
- Stay propped up for 20–30 minutes. If you have a peak flow meter, check your number as you recover.
- Not better in 5–10 minutes? Follow the emergency steps in your asthma action plan. Some doctors describe this as a “4-4-4” pattern with a reliever inhaler. If you’re still struggling to breathe or can’t speak full sentences, call emergency services right away.
Key point: Your rescue inhaler is usually the fastest way to open tight airways during an asthma cough at night.
One-liner: Sitting upright, using your rescue inhaler as your action plan directs, slow breathing, and your 4-4-4–style emergency steps can help calm a nighttime asthma cough.

Setting Up for Better Nights: Preventive Strategies to Avoid Nighttime Asthma Cough
Once your breathing has settled, shift to prevention for better nighttime asthma control. Strong daytime control and a low-trigger bedroom make night coughs far less likely. Focus on the basics: take controller medicines as prescribed, choose sleep positions that help, and keep your room clean, warm, and calm.
One-liner: Strong daytime asthma control and a smart bedroom setup make night coughs much less likely.
Follow Your Asthma Action Plan and Optimize Medications in the Evening
Your asthma action plan is your guide. Take your daily controller inhaler on schedule. Don’t skip the evening dose if it is prescribed.
Still waking up coughing? Ask your doctor about timing or dose changes. Some people do better with an evening controller or a leukotriene tablet at night. If evening activity sparks symptoms, your doctor might suggest using your reliever before activity.
A quick control check, called the Rule of Twos: if you use your reliever more than two times a week, or wake up more than two nights a month, your asthma isn’t well controlled and your plan needs a tune-up.
One-liner: Controller medicines taken on schedule are the base for quiet nights.
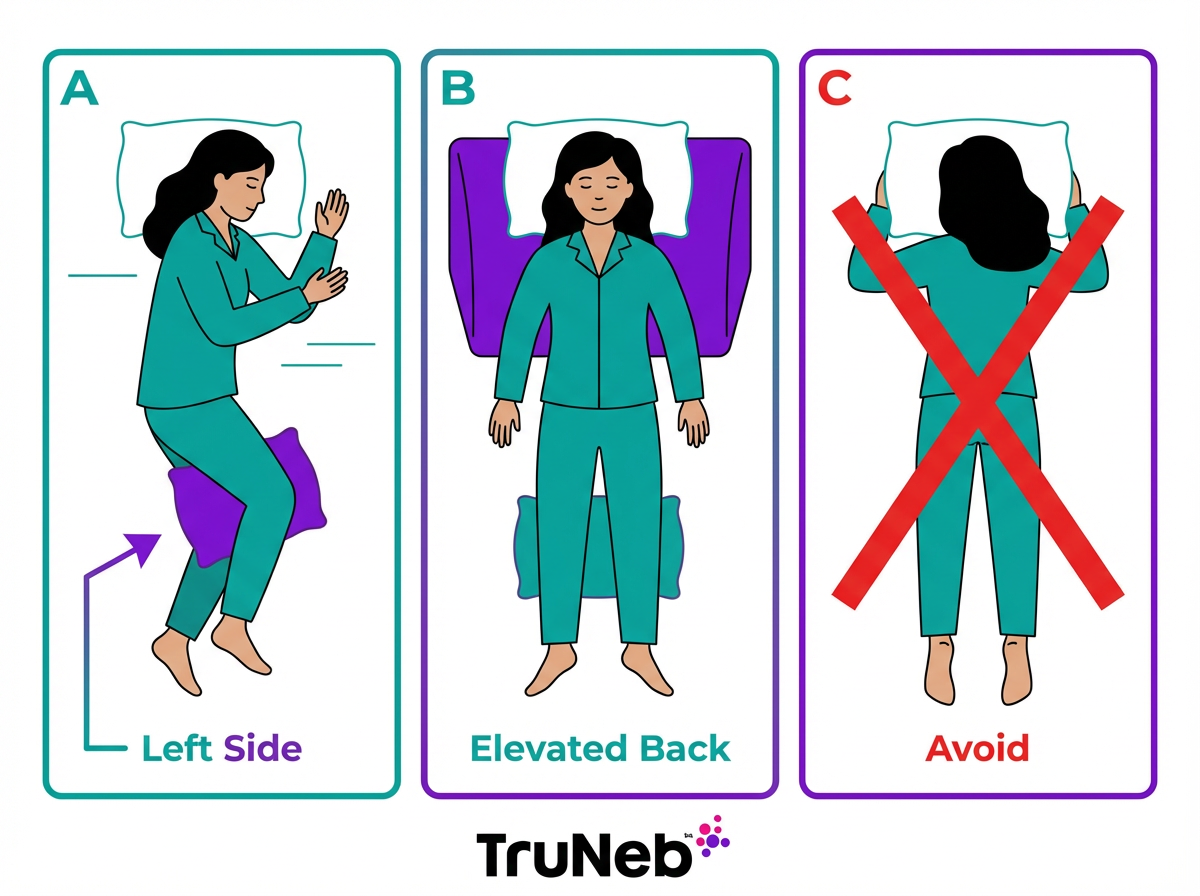
Sleep Positions That Help You Breathe Easier
Left side sleeping with a pillow between your knees can reduce reflux, a common night trigger for cough. Gravity keeps stomach acid lower than the esophagus, which can ease airway irritation.
On your back, raise your head and shoulders on a wedge or extra pillows. Elevation helps keep airways open and limits postnasal drip into the throat.
Avoid stomach sleeping, which can compress your chest. Some people also find the right side less comfortable than the left. Try these positions for a week to see what gives you the calmest nights.
One-liner: Left side or an elevated back position can cut down reflux and drip, easing night cough.
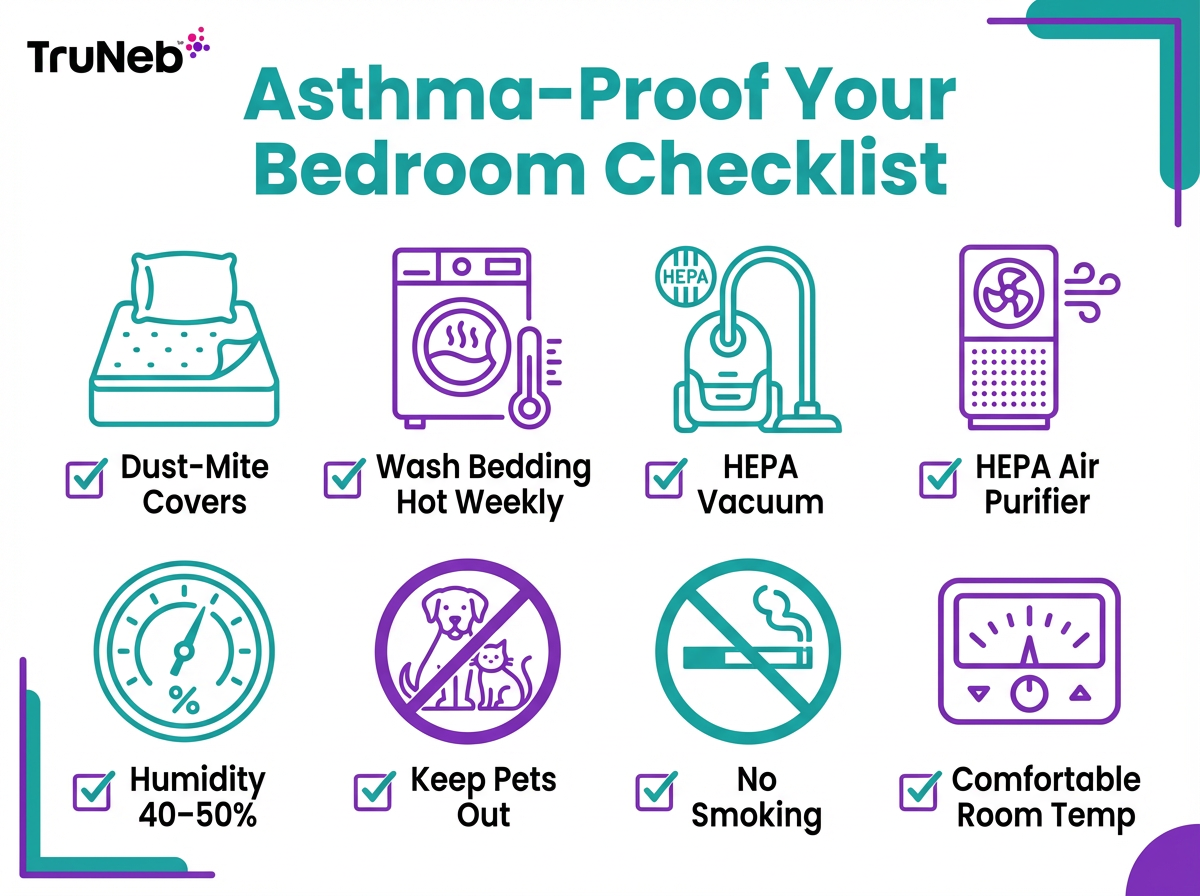
Asthma-Proof Your Bedroom Environment
Reduce allergens where you sleep. Use dust-mite-proof covers on your mattress and pillows, and wash bedding weekly in hot water. Clean surfaces with a damp cloth and vacuum with a HEPA filter.
Keep humidity in a middle range, about 40–50%. If air is very dry, a humidifier can help. If your room is damp, lower humidity to discourage mold and mites. A HEPA air purifier can remove dander and pollen in the room.
Keep pets out of the bedroom, and avoid very cold air or a fan blowing on your face at night. No smoking in or near the bedroom. A slightly warm room can feel easier for breathing.
One-liner: Cleaner air, dust-mite covers, and balanced humidity lower night triggers.
Smart Bedtime Habits and Routine Changes
Key takeaway: Light evenings and a calm routine help your lungs settle before sleep.
| Habit | Do | Avoid/Notes | Why it helps |
|---|---|---|---|
| Meals | Finish eating 2–3 hours before bed | Large or spicy late meals | Reduces reflux‑related cough |
| Alcohol & scents | Limit alcohol; keep fragrances out of the bedroom | Strong scents or sprays before sleep | Lowers airway irritation |
| Exercise | Wind down with gentle breathing or stretching | Hard exercise right before bed | Avoids late airway tightening |
| Screens & lights | Dim lights; turn off screens at least 1 hour before bed | Late scrolling or bright light | Supports better sleep quality |
| Medications | Take any evening medicines on schedule | Don’t skip doses | Keeps asthma control overnight |
These habits support, but don’t replace, your prescribed asthma medicines.
One-liner: Light evenings and a calm routine help your lungs settle before sleep.
Medication Delivery Options at Night: Inhaler, Spacer, or Nebulizer
Most people do best with a metered-dose inhaler and a spacer. A spacer helps medicine reach your lungs, especially when you feel anxious or sleepy.
Some patients, like young children or adults who struggle with inhaler technique, use a nebulizer at night as part of their doctor’s plan. A nebulizer turns liquid medicine into a fine mist you breathe in over several minutes. A portable mesh nebulizer such as the TruNeb™ Portable Mesh Nebulizer is small and quiet, which can make nighttime treatments easier at home or on the go.
Your doctor might also recommend saline inhalation in certain mucus-heavy conditions. Hypertonic saline (3% or 7%) can help loosen thick mucus for some people, but it should only be used under medical guidance and never replaces your prescribed controller or reliever medicines. In some people, hypertonic saline can briefly worsen cough or chest tightness, which is another reason to use it only with guidance.
⚠️ You might see products labeled “steam inhaler” or facial steamer, but these are not designed for breathing asthma medicines and should never replace your inhaler or nebulizer.
Talk to your doctor before trying a new medication.
One-liner: For most people, the best device is the one they can use correctly so the medicine reaches their lungs.
When to See a Doctor and Warning Signs You Should Not Ignore
If night coughs are common, schedule a visit with your doctor. A quick check of control helps: needing your reliever more than two times a week or waking more than two nights a month means your asthma isn’t well controlled and your plan needs an update. Bring notes about nighttime symptoms to your next review so you and your doctor can adjust your asthma action plan.
Go to emergency care right away if you can’t speak full sentences, your lips or face look blue, you feel faint or confused, or your breathing is getting harder even after medicine. For children, watch for flaring nostrils, belly pulling in with breaths, or trouble talking or crying.
Key point: Night symptoms more than twice a month are a sign your asthma isn’t well controlled and your plan needs a tune-up with your doctor.
One-liner: If rescue medicine doesn’t ease your breathing quickly or severe signs appear, get emergency care now.
FAQs – Quick Answers to Common Questions
Tap or click a question below to see the answer:
For most people, the fastest way to relieve an asthma cough is the quick-relief inhaler your doctor prescribed, used as directed in your asthma action plan. Sit upright, breathe slowly, and let the medicine work over the next few minutes. If your cough and breathing don’t improve quickly, or if symptoms are severe, treat it as an emergency and seek urgent medical care.
The 4-4-4 rule is a nickname some doctors use for an emergency pattern of using a quick-relief inhaler during an asthma attack (a short series of puffs, waiting a few minutes, then repeating). Only follow this pattern if it’s written in your personal asthma action plan, and call emergency services if you’re not improving.
If you need your reliever more than two times a week, wake more than two nights a month, or need more than two rescue refills per year, your asthma isn’t well controlled and your plan needs a change.
Your body clock (circadian rhythm) lowers cortisol overnight, airways can be more reactive, lying down can worsen reflux and drip, bedrooms hold allergens, and night air is usually cooler and drier. Together, these raise the chance of cough.
Warm liquids (water or decaf tea) can soothe the throat. Honey can calm throat irritation in adults and children over one year old. A small amount of caffeine might act as a mild bronchodilator but isn’t a substitute for your prescribed inhaler and can affect sleep.
Vicks can feel soothing, but it doesn’t open the airways. For some people, strong smells can irritate the lungs. Use your prescribed inhaler or nebulizer for relief and follow your asthma action plan.
One-liner: Quick rules to remember – your action plan usually puts your inhaler first, uses a 4-4-4–style emergency pattern, and applies the Rule of Twos to check if your asthma is under control.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms and before changing any medications or treatment plan. If you think you’re having a medical emergency, call emergency services right away.