On this page

Home Treatment for Asthma: Manage It Safely at Home
Home treatment for asthma means adding safe, simple steps to your doctor’s plan. People sometimes call these home remedies for asthma relief, but they should always support your prescribed treatment, not replace it. There’s no cure for asthma, but you can reduce symptoms at home and feel more in control.
Start with a written Asthma Action Plan from your doctor. Keep it handy. Follow it every day. The tips below give you practical asthma home management tips you can start using right away.
At home you can:
- Avoid common triggers in your space.
- Practice breathing and relaxation.
- Stay active with a warm-up and cool-down.
- Eat a balanced diet and work toward a healthy weight.
- Use your inhalers the right way. A spacer helps.
- Use devices wisely, like a portable nebulizer if your doctor recommends it.
- Track symptoms and peak flow so you spot changes early.
Safety note: Talk to your doctor before trying a new medication or supplement.
Key take: Home steps work best when they complement your prescribed plan.
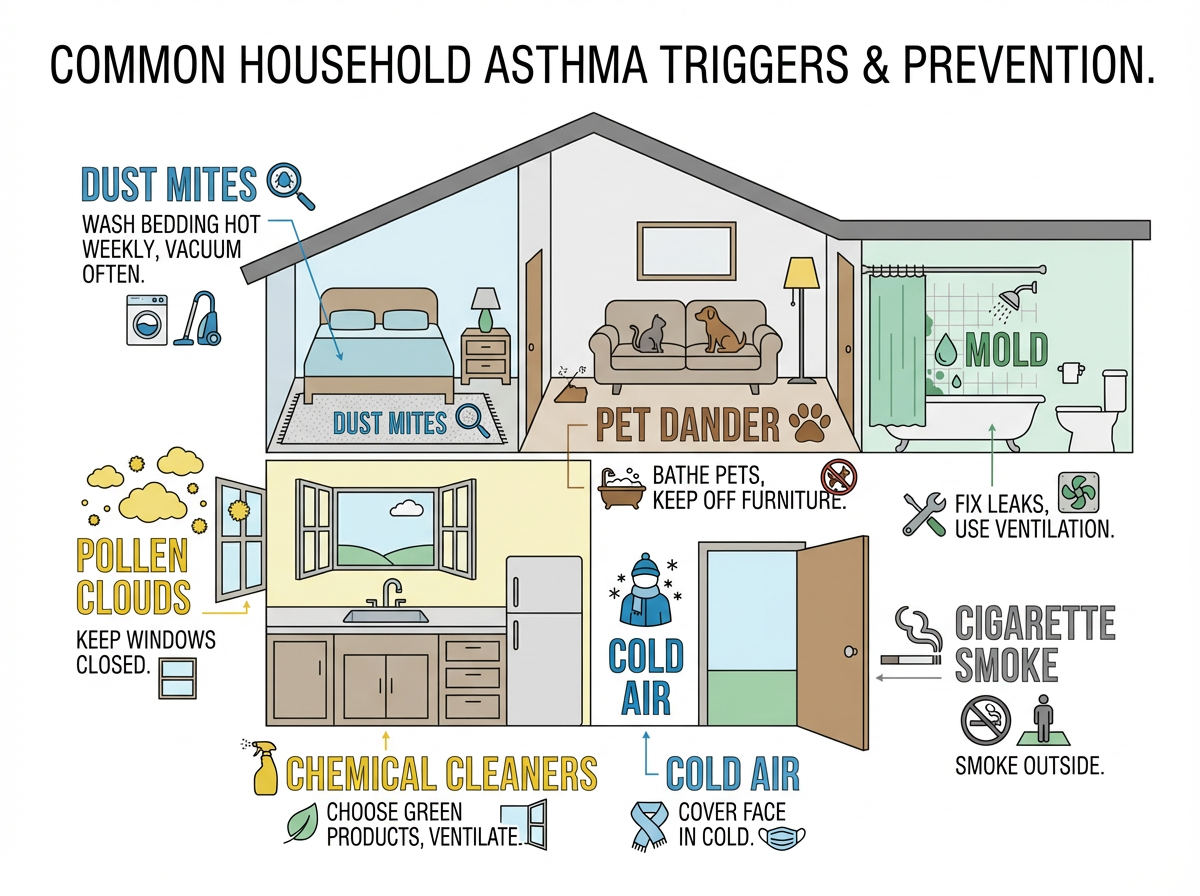
Avoiding Common Asthma Triggers at Home
You breathe easier when you remove what sets you off. Tackle the big triggers first.
- Dust mites: Use zippered covers on pillows and mattress. Wash bedding weekly in hot water. Vacuum with a HEPA filter and damp‑dust hard surfaces.
- Pet dander: Keep pets out of the bedroom. Bathe and brush outside if possible. Consider a HEPA air purifier.
- Mold and dampness: Fix leaks fast. Use a dehumidifier to keep humidity near 30–50%. Vent bathrooms and kitchens.
- Smoke: No smoking or vaping indoors. Avoid secondhand smoke and wildfire smoke. On smoky or high‑pollution days, check your local air quality index (AQI) and keep windows closed; use a HEPA purifier if you have one.
- Pollen: Close windows during high pollen counts. Shower and change clothes after outdoor time. Use air conditioning with a clean filter.
- Cold air: Wear a scarf over your nose and mouth outside to warm the air.
- Strong odors and sprays: Choose unscented cleaners. Skip aerosols. Ventilate while cleaning.
- Pests and crumbs: Keep food sealed and surfaces clean to reduce roaches and dust.
A HEPA filter is a type of filter that traps tiny particles like dust and dander so they’re less likely to end up in your lungs.
Even a few small changes at home can make day‑to‑day breathing feel easier.
Quick tip: When you control your home environment, you control a lot of your asthma symptoms.
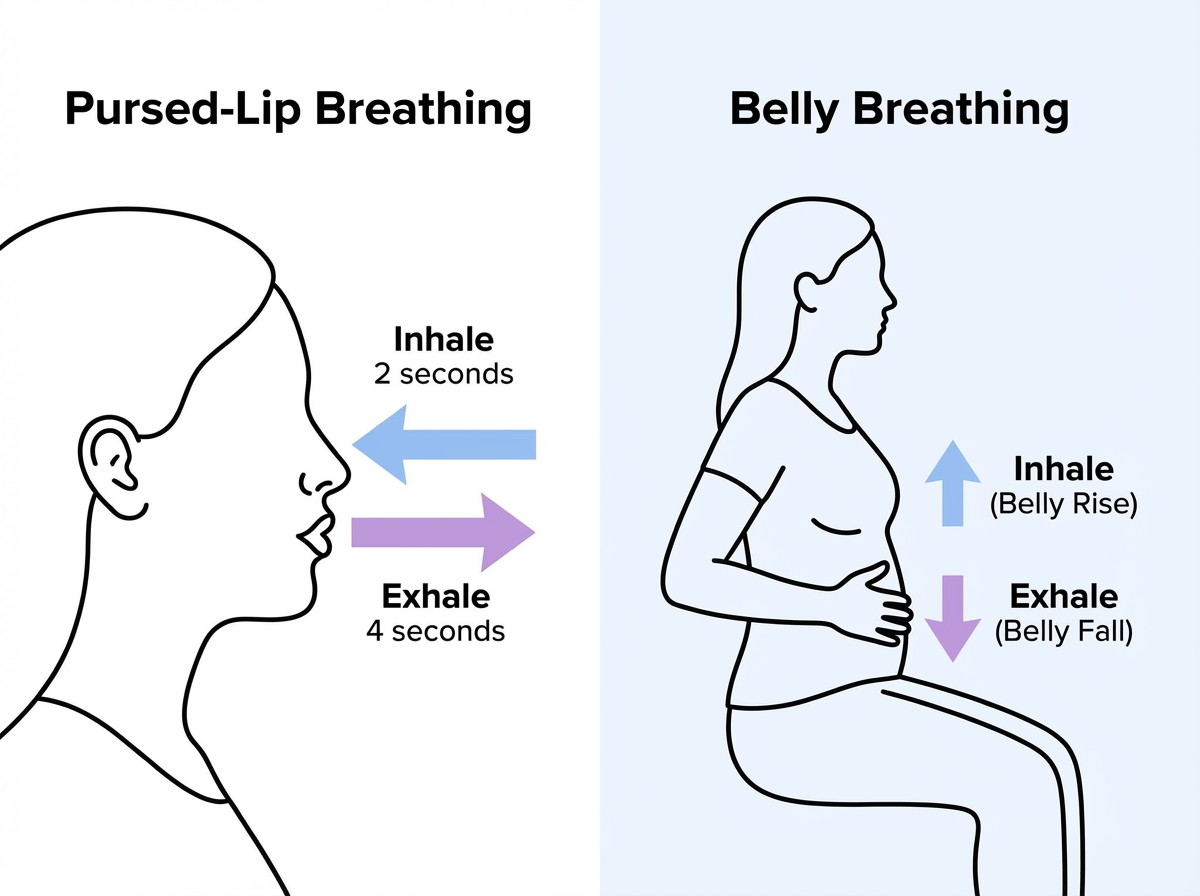
Breathing and Relaxation Techniques for Asthma Relief
Calm breathing exercises for asthma help you feel in control. They can ease mild symptoms and improve how well you use your lungs.
Pursed‑lip breathing (do this anywhere):
1) Inhale slowly through your nose for 2 counts.
2) Purse your lips like you’re blowing out a candle.
3) Exhale gently through pursed lips for 4 counts.
Belly (diaphragmatic) breathing:
1) One hand on your chest, one on your belly.
2) Breathe in through your nose so your belly rises.
3) Exhale slowly. Keep shoulders relaxed.
Methods like Buteyko and Papworth also train gentle nasal breathing and relaxation. Regular practice (5–10 minutes a day) can improve quality of life.
Stress can trigger symptoms. Add simple mindfulness, quiet music, or a short body‑scan to settle your nervous system.
If you’re without an inhaler during mild symptoms, these techniques can help you buy time. They don’t replace your rescue inhaler or emergency care. Only use these for mild symptoms; if you’re really struggling to breathe, call emergency services or go to urgent care instead of trying to manage it alone. Get medical help if breathing doesn’t improve.
Key take: Slow, steady breathing can help you regain control during mild symptoms.
Staying Active Without Triggering Asthma
Exercise is good for asthma when it is well managed. It builds stamina and helps you feel stronger.
Good choices:
- Swimming in warm, humid air.
- Walking or easy cycling.
- Yoga or Pilates for gentle breath control.
Helpful tips:
- Do a full warm‑up and cool‑down.
- If your doctor advised it, follow their instructions for using your quick‑relief inhaler before activity.
- On high pollen or very cold days, move your workout indoors.
- Pace yourself and stay hydrated.
You don’t have to avoid movement. You just need a plan that fits your lungs.
Quick take: Warm up, pace yourself, and use your reliever as directed to keep moving safely.
Healthy Diet and Lifestyle Changes for Asthma
Food and daily habits can support calmer airways. Here’s how:
What to eat more of:
- Fruits and vegetables rich in antioxidants.
- Omega‑3s from fish, flaxseed, or walnuts.
- Vitamin D sources when appropriate.
- Probiotic foods like yogurt or kefir.
Some research links probiotic‑rich foods like yogurt and kefir to calmer immune responses in people with asthma. Ask your doctor if you should check your vitamin D level or take a supplement.
What to limit:
- Sulfite‑heavy foods and drinks if they trigger you (some dried fruits, wine).
- Any known food allergens.
Lifestyle wins:
- Aim for a healthy weight; even modest weight loss can help breathing.
- No smoking. Avoid secondhand smoke.
These steps don’t replace your medicines. They can help them work better day to day.
Key take: A produce‑forward diet, omega‑3s, probiotics, and no smoking support better asthma control.
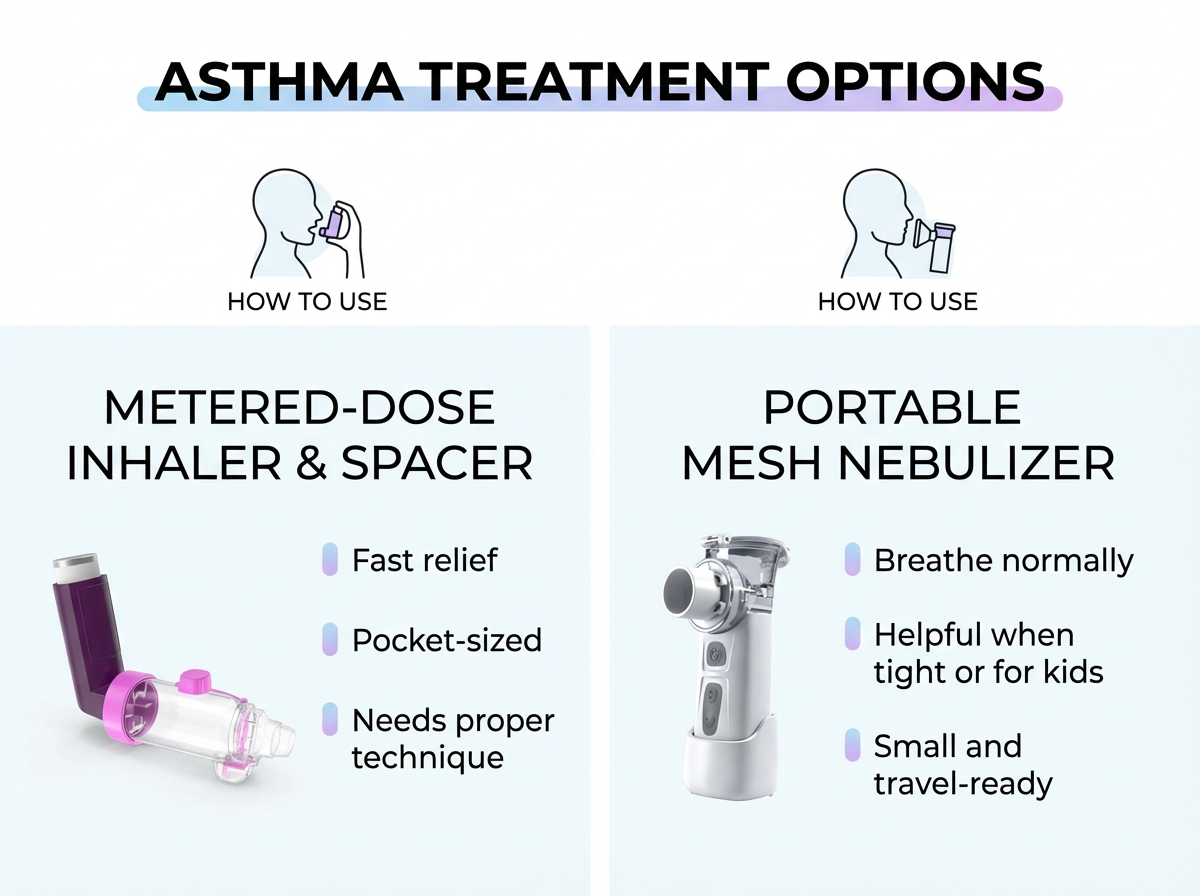
Proper Use of Asthma Medications and Devices at Home
Your medicines work best when you use them right.
Follow your Asthma Action Plan:
- Know your daily controller medicine and your quick‑relief inhaler.
- Know your green, yellow, and red steps. Keep the plan where you can see it.
Use your inhaler with good technique:
In general, these are the basic steps for good metered‑dose inhaler technique (your doctor or pharmacist can show you what’s right for your device):
1) Shake, then exhale fully.
2) Seal lips on the mouthpiece, press, and breathe in slowly and deeply.
3) Hold your breath about 10 seconds, then exhale.
A spacer can make each puff reach your lungs better.
Home nebulizer treatments:
- A nebulizer turns liquid medicine into a mist you breathe normally.
- Modern portable mesh nebulizers, like the TruNeb™ Portable Nebulizer, are small and quiet, which makes daily treatments easier to do at home or on the go.
- Don’t confuse a medical nebulizer with a “steam inhaler” or facial steamer. Those are not designed to deliver asthma medicine.
- Clean your device after each use as directed.
Inhaler or nebulizer?
- Inhalers are fast and pocket‑friendly.
- A nebulizer can help if you are too tight to coordinate inhaler steps, for young children, or when your doctor recommends it.
- For some people, nebulizer treatment for asthma at home is easier than using an inhaler during bad flare‑ups or for young children, when their doctor recommends it.
Inhaler with spacer vs portable nebulizer: quick comparisonKey takeaway: Both deliver similar medicines; use the device your doctor recommends and the one you can use correctly.
| Device | How it’s used | Best when | Portability | Cleaning |
|---|---|---|---|---|
| Inhaler with spacer | Press the canister and inhale slowly through the spacer, then hold your breath briefly. | Everyday control and quick relief when you can use correct technique. | Pocket‑sized, ready to carry. | Rinse spacer regularly and air‑dry as directed. |
| Portable mesh nebulizer | Breathe normally through a mouthpiece or mask while the device makes a fine mist. | When breathing is tight, during bad flare‑ups, or for young children, under doctor guidance. | Small and travel‑ready, can run on batteries. | Rinse and disinfect parts after each use as directed. |
Note: A steam inhaler or facial steamer is not a medical nebulizer.
Monitor your control:
- A peak flow meter is a simple tool to track how fast you blow air out.
- Keep a short diary of symptoms and peak flow. Share it at checkups.
Safety note: Talk to your doctor before changing any medication or device routine.
Key take: Right technique, a clear plan, and smart use of inhalers or a portable nebulizer keep home care on track.
Natural Remedies and Supplements: What Helps and What Doesn’t
When people talk about “natural treatment for asthma at home,” these options can play a small, supportive role. They don’t replace your inhalers or your plan.
What can help a bit:
- Honey can soothe a cough at night.
- Ginger and garlic show anti‑inflammatory effects in lab and animal studies. So far, human studies haven’t shown that these foods can replace asthma medicines.
- Omega‑3s support overall health; benefits vary.
- Caffeine is a mild bronchodilator and can sometimes help briefly for some people, but it’s not a replacement for your rescue inhaler.
Be careful:
- Essential oils and strong scents can trigger symptoms for some. Always stop right away if your breathing feels worse around strong scents.
- Herbal mixes that claim a cure are not proven and can be risky. Some mixes can interact with prescription medicines or trigger allergies.
- Hypertonic saline nebulizers are used for mucus clearance in conditions like bronchiectasis, not as routine asthma therapy. People with asthma should only use saline nebulizers exactly as prescribed; using them on your own for asthma can actually irritate your airways. If your doctor prescribes saline for a special case, follow their instructions. TruNeb offers 3% and 7% medical‑grade hypertonic saline for those specific needs.
Safety note: Some supplements can interact with prescriptions, so always clear new therapies with your doctor first.
Key take: Natural remedies can comfort symptoms, but they don’t replace your inhaler or action plan.
Know When Home Treatment Isn’t Enough
⚠️ Treat these signs as an emergency, not something to watch at home:
- You struggle to speak in full sentences.
- Your rescue inhaler is not helping.
- Your lips or fingernails look bluish.
- You feel very tired or confused.
Follow the red steps in your Asthma Action Plan and seek emergency care. Don’t wait this out at home.
If you need your reliever often, wake at night with symptoms, or limit normal activities, your asthma is not well controlled. If you’re reaching for your reliever most days of the week, that’s a sign to schedule a visit and update your treatment plan.
Safety note: Severe asthma can be life‑threatening. Get help early.
Key take: If your reliever isn’t helping and speaking is hard, treat it as an emergency.
Frequently Asked Questions
These quick answers sum up what most people ask about treating asthma at home. Tap or click a question below to see the answer:
There isn’t one single remedy. The biggest wins are avoiding your triggers, using your inhalers correctly, and practicing simple breathing exercises. These work best together.
Get away from the trigger, sit upright, and try slow pursed‑lip breathing. A strong coffee or tea can help a little for some people, but it’s not a substitute for medical treatment. If you’re finding it hard to speak, walk, or catch your breath, call emergency services right away instead of trying home steps first.
Honey can soothe a cough. Ginger shows promise in lab studies. They can make symptoms feel a bit easier, but they don’t prevent an attack. Use them only as add‑ons with your doctor’s okay.
Inhalers with a spacer are fast and convenient. A nebulizer can help when you’re too tight to coordinate a puff or for young children. Both deliver similar medications; the device your doctor recommends is usually based on what you can use correctly. A portable device like TruNeb can make treatments simpler to fit into your day.
No. There is no natural or medical cure. You can control asthma very well by following your action plan and using smart home habits.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk to your doctor about your symptoms, medications, and any home treatments you want to try. Never stop or change a prescription without your doctor’s guidance.







