On this page

Signs and Symptoms of Cough Variant Asthma
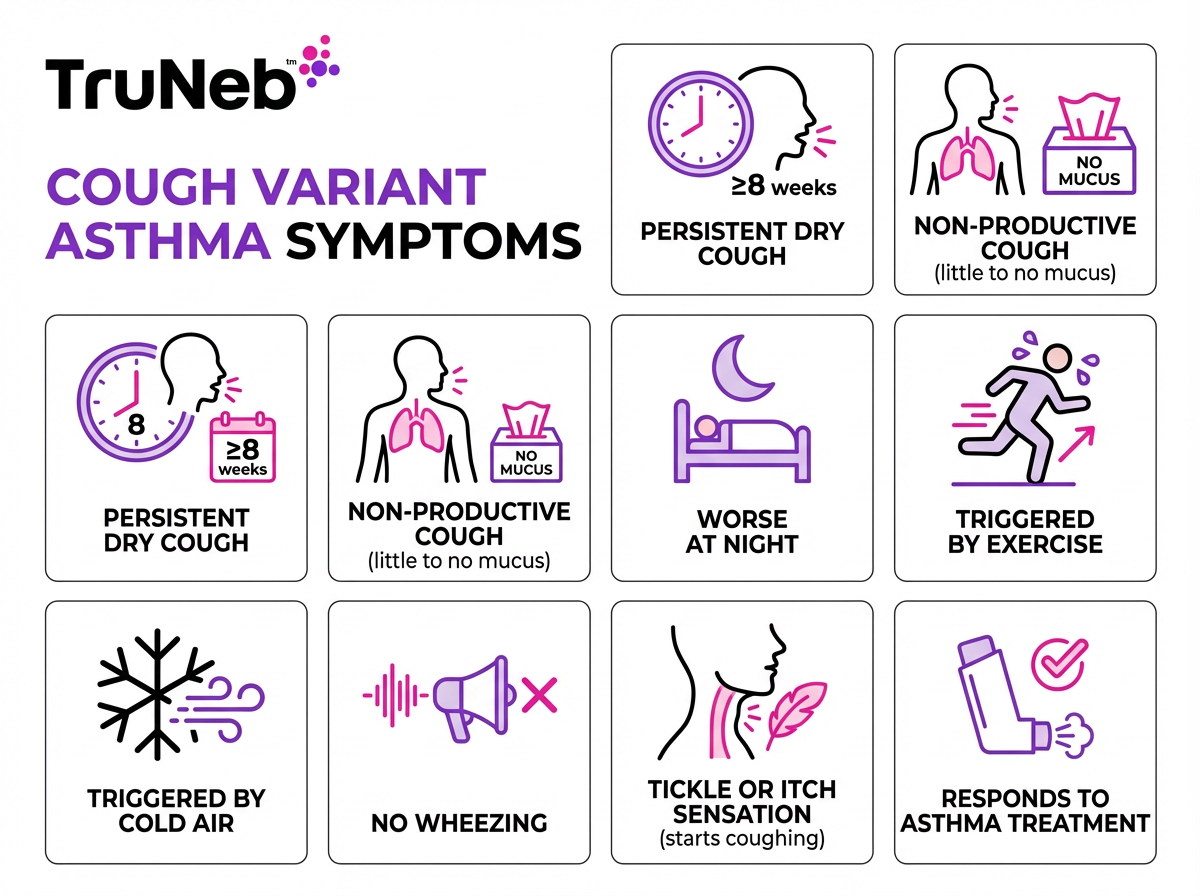
Cough-variant asthma (CVA) means the only symptom is a cough. It’s a chronic, dry cough asthma pattern that lasts 8 weeks or more and usually improves with asthma treatment.
What it looks like day to day:
- Persistent, dry, non-productive cough (little to no mucus)
- Worse at night, with exercise, or in cold air
- No wheezing, no chest tightness, and no obvious shortness of breath between coughs
- Feels like a tickle or itch in the airways that triggers bouts of coughing
- Mild chest irritation from frequent coughs; a small amount of mucus can show up in some people
These cough variant asthma symptoms can look like allergies or a lingering cold, which is why CVA is easy to miss.
Adults typically notice an annoying nighttime cough or a cough during exertion. Children can have a chronic nighttime cough that can even lead to vomiting, but still no wheeze. Because there’s no wheezing, CVA gets mistaken for allergies or a lingering cold.
⚠️ Safety note: If your cough lasts longer than 6–8 weeks, talk with your doctor about it.
Key takeaway: Cough‑variant asthma is asthma that shows up as a long‑lasting dry cough without wheezing.
Causes and Common Triggers
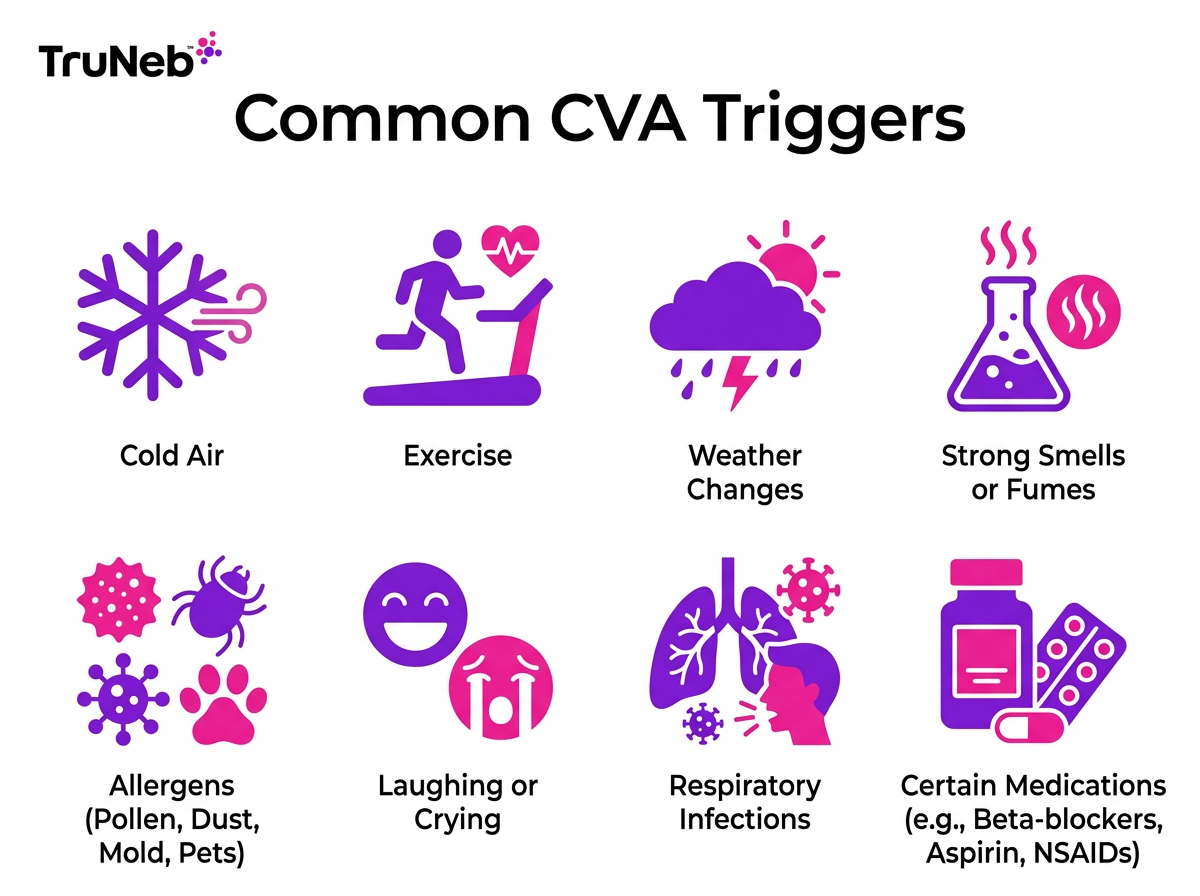
The causes of cough variant asthma are the same as classic asthma: airway inflammation and hyper-reactivity, meaning the breathing tubes are irritated and extra sensitive. For some people, that inflamed airway mainly triggers cough rather than wheeze. Doctors don’t fully understand why some people only develop a cough instead of wheezing, but it likely relates to individual differences in how sensitive their airways are.
Common triggers that set off coughing fits:
- Cold or dry air (stepping outside on a cold day)
- Exercise, especially in cool air
- Weather or temperature swings
- Strong smells and fumes (perfume, smoke, air pollution)
- Laughing or crying hard
- Allergens (pollen, dust, mold, pet dander)
- Respiratory infections (a cold or bronchitis that never fully went away)
- Certain medicines in susceptible people (beta-blockers; aspirin/NSAIDs)
Triggers don’t cause asthma by themselves; they spark symptoms in someone who already has CVA.
Key takeaway: Cold air, exercise, allergens, infections, and some medicines can trigger the cough in cough‑variant asthma.
Who Is at Risk for Cough Variant Asthma?
Anyone can develop cough variant asthma. Factors that raise the odds:
- Childhood onset is common
- Personal or family history of allergies, eczema, or asthma
- Smoking or secondhand smoke exposure
- Air pollution or workplace dust/chemicals
- Obesity
- Past asthma or wheezing that seemed to go away
Key takeaway: The risk of cough‑variant asthma rises with family history, allergies, smoke exposure, pollution, and obesity.
Cough Variant Asthma in Children
Cough‑variant asthma in children is common. A lot of kids show a stubborn dry cough as the first or only sign of asthma.
What parents notice:
- A dry cough that lingers long after a cold
- Nighttime cough that wakes the child or sometimes leads to vomiting
- Cough with play or running
Diagnosing CVA in young kids is hard because it’s tough for them to do spirometry well. Doctors sometimes use history and a short, doctor‑supervised trial of asthma medicine to see if the cough improves. Methacholine challenge tests are rarely done in very young children.
How treatment is given: kids usually use a spacer with an inhaler or a mask nebulizer, since it’s easier to breathe normally during a treatment. A quiet portable mesh nebulizer can make home treatments easier for toddlers and preschoolers.
Early treatment matters. Untreated CVA in kids can progress to classic asthma with wheezing, but with proper care most children do very well.
Key takeaway: In children, a dry nighttime cough without wheeze is a common sign of cough‑variant asthma, and this cough usually improves with asthma medications.
How Is Cough Variant Asthma Diagnosed?
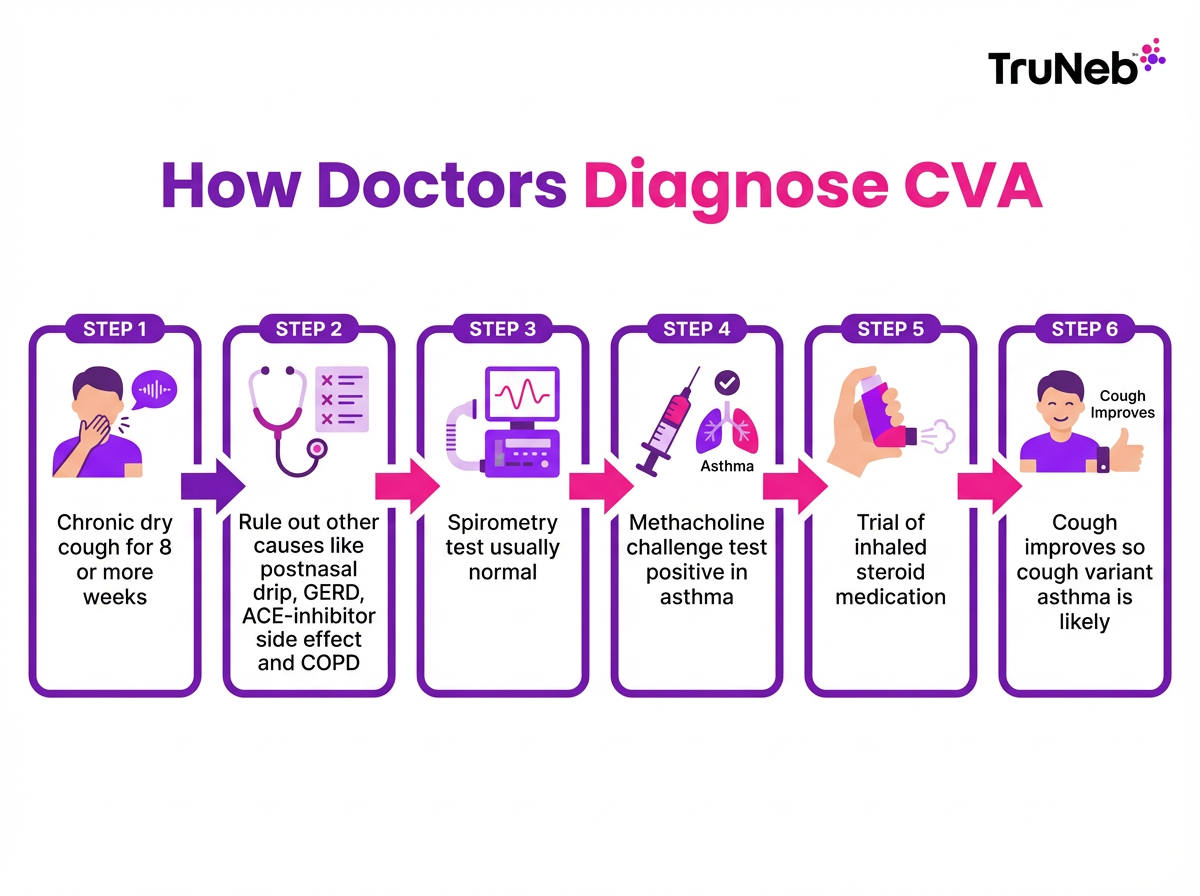
Diagnosing CVA can take time because cough is common and has multiple causes. Doctors first rule out other reasons for chronic cough, then confirm asthma.
How doctors test for cough‑variant asthma:
- Medical history and exam. A chest X-ray is usually normal, which helps rule out infections.
- Spirometry (lung function). It’s a breathing test where you blow into a tube to see how well air moves in and out of your lungs. Results are usually normal at rest in cough‑variant asthma.
- Methacholine challenge test. Methacholine is a medication that gently narrows the airways in people with asthma so doctors can see how reactive your lungs are. You inhale a special mist in small steps while doing spirometry; the test is positive when lung function drops by a set amount and then improves with a bronchodilator (a medicine that opens narrowed airways).
- Excluding mimics. Your doctor will also check for postnasal drip, GERD, chronic bronchitis/COPD in smokers, or ACE-inhibitor cough.
- Therapeutic trial. Sometimes the clearest answer is a short trial of an inhaled steroid under a doctor’s guidance. If the cough improves, that supports CVA.
Tip: Keep a simple cough diary to share patterns and response to treatment.
Key takeaway: Normal test results don’t rule out cough‑variant asthma; a positive methacholine challenge or a clear improvement with asthma medications often confirms the diagnosis.
How Is Cough Variant Asthma Treated?
Cough‑variant asthma treatment mirrors that of typical asthma. The goal is to stop coughing spells now and prevent the cough from coming back.
Treatment basics:
- Quick‑relief inhaler (such as albuterol). This type of inhaler is used to relax airway muscles and calm a coughing fit under your doctor’s direction.
- Daily controller inhaler (inhaled corticosteroid). Low‑dose steroids (like fluticasone or budesonide) reduce airway inflammation and help prevent the cough. Consistent use for several weeks is key.
- Leukotriene modifier (montelukast). A daily pill that can help, especially when allergies play a role.
- Combination inhalers (ICS + long‑acting bronchodilator). Used if control isn’t enough with ICS alone. Long‑acting bronchodilators aren’t used by themselves in asthma.
- Allergy care. Antihistamines or nasal steroid sprays, and sometimes allergy shots, can help if allergies trigger the cough.
Treatment plans are individualized, and only your doctor can decide which medicines and doses are appropriate. Most people notice improvement over 2–8 weeks with the right plan.
⚠️ Safety note: Talk to your doctor before trying a new medication or changing doses.
Key takeaway: In cough‑variant asthma, rescue inhalers can help stop coughing spells, and daily inhaled steroids help prevent them from starting.
Inhalers vs. Nebulizers – Which Is Better for CVA?
Both inhalers and nebulizers deliver the same asthma medicines. The best choice is the one you can use correctly every time.
| Device | How it works | Pros | Best for | Considerations |
|---|---|---|---|---|
| Metered‑dose inhaler (MDI) + spacer | Pressurized canister releases medicine; breathe in slowly through a spacer | Quick, portable, widely available | Most adults and older kids with good technique | Needs proper timing/technique; spacer recommended |
| Dry powder inhaler (DPI) | Powder dose is inhaled with a strong, fast breath | Small; no spacer needed | Older kids/teens/adults who can inhale forcefully | Not ideal during a flare if you can’t take a strong breath |
| Jet nebulizer (compressor) | Compressor turns liquid medicine into a mist over 5–10 minutes | Hands‑free breathing; useful during illnesses | Infants/toddlers; people who struggle with inhalers | Larger, noisy, needs outlet and cleaning |
| Portable mesh nebulizer | Vibrating mesh creates an ultra‑fine mist in a few minutes | Quiet, pocket‑size, battery‑powered; easy for kids | Home or on‑the‑go treatments when coordination is hard | Requires cleaning and correct assembly; higher upfront cost |
Key takeaway: Inhalers and nebulizers deliver the same medicines; choose the device you can use correctly and consistently.
Modern portable mesh nebulizers, such as TruNeb, are battery‑powered, pocket‑size, and very quiet, which can make treatments easier at home or on the go.
Nebulizers aren’t stronger than inhalers—they deliver the same medicine in a different way.
⚠️ Steam inhalers are not the same as nebulizers and shouldn’t be used to deliver prescription asthma medications.
Follow your doctor’s advice on which device fits your plan. Some people keep both: an inhaler for quick use and a nebulizer for sick days.
Key takeaway: Use the device you can use correctly—both deliver the same medicines.
Managing Cough Variant Asthma Day-to-Day
Daily habits make a big difference.
- Avoid or reduce triggers. Keep windows closed on high‑pollen days; clean bedding for dust mites; wear a scarf or mask in cold air; warm up before exercise and use your inhaler as prescribed.
- Keep a cough/trigger diary. Note when coughing happens and what you were doing. Patterns help you and your doctor fine‑tune care.
- Take medicines only as your doctor prescribes. Ask your doctor whether you should keep a rescue inhaler with you and whether a peak flow meter would help you track changes.
- Get an asthma action plan. Know your green, yellow, and red zones and what to do in each.
- Nebulizer care at home. Under medical guidance, some people add sterile hypertonic saline by nebulizer. Hypertonic saline is a sterile, salty solution (3% or 7%) that can draw water into the airways and loosen mucus. This should only be used if your doctor recommends it, since the mist can trigger coughing or irritation in some people.
- Healthy basics. Don’t smoke; aim for a healthy weight; stay hydrated; manage reflux; stay up to date on vaccines.
⚠️ Safety note: Talk to your doctor before trying hypertonic saline or any new treatment.
Key takeaway: Consistency—avoid triggers, take meds, track symptoms—is what keeps CVA quiet.
When to See a Doctor and When to Seek Emergency Care
See your doctor if a cough lasts more than 6–8 weeks or is getting worse. Early care brings faster relief and can prevent complications.
Go to urgent or emergency care now if you have:
- Trouble breathing at rest or can’t speak full sentences
- Wheezing or chest tightness with the cough
- Blue lips or fingernails (cyanosis)
- Fast heartbeat, faintness, or confusion
- Coughing up blood
- Severe, relentless coughing that prevents sleep or doesn’t improve with your rescue inhaler
⚠️ If you have any of these severe symptoms, call 911 (or your local emergency number) or go to the emergency room right away.
Most CVA is managed without the ER. Knowing your action plan and warning signs keeps you safe.
Key takeaway: A cough longer than 8 weeks or any trouble breathing needs prompt medical care.
Frequently Asked Questions about Cough Variant Asthma
Tap or click a question below to see the answer:
This FAQ answers common questions about what cough‑variant asthma sounds like, how serious it is, how doctors test for it, treatment options, and whether it can go away.
It usually sounds like a dry, hacking cough that doesn’t quit, with no wheeze. People describe a tickle or itch in the throat or chest. It’s typically worse at night or with exercise.
It’s manageable for most people with the right care. About 30–40% of people with cough‑variant asthma go on to develop classic asthma symptoms like wheezing and shortness of breath. Work with your doctor to lower your risk and keep symptoms controlled.
Doctors start with your history, exam, and spirometry; results can be normal in cough‑variant asthma. A methacholine challenge can show airway reactivity, and doctors also rule out other causes of chronic cough. Sometimes a short, doctor‑guided trial of an inhaled steroid helps confirm the diagnosis if the cough improves.
It’s treated like regular asthma using rescue inhalers for quick relief and daily controller medicines, such as inhaled corticosteroids, to prevent symptoms. Your doctor decides which medicines and doses are right for you.
Symptoms can go quiet for long stretches, especially in children. Some people can step off daily medicines under a doctor’s guidance, but the tendency toward asthma remains, so stay watchful and restart treatment if symptoms return.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms and before starting, stopping, or changing any medication or treatment.