On this page

Why COPD Treatment Needs a Special Approach in Older Adults
COPD (chronic obstructive pulmonary disease) care in older adults works best when it’s tailored to age-related changes. Lungs can be stiffer, breathing muscles weaker, and recovery slower. A lot of seniors also live with heart disease, diabetes, arthritis, or memory changes. That mix affects which treatments help and which cause side effects.
Daily routines matter. Hand strength, eyesight, and coordination can make inhalers hard to use. Some older adults also take several daily medications, which raises the risk of drug interactions and missed doses.
Your goals can look different, too. The plan should help you breathe easier, prevent flare-ups, and protect independence at home. A team approach helps: your primary doctor, a pulmonologist, a respiratory therapist, and family or a caregiver all play a role.
Key takeaway: In seniors, COPD treatment must balance breathing relief, safety, and independence.
Medication Therapy for Seniors With COPD
Most COPD plans include bronchodilators and sometimes inhaled steroids. The right device matters as much as the medicine.
Bronchodilators and inhaler devices
- Short-acting bronchodilators (like albuterol or ipratropium) ease sudden symptoms.
- Long-acting bronchodilators (LABA or LAMA, such as salmeterol or tiotropium) keep airways open day to day.
- Technique matters. A lot of older adults struggle with timing sprays or inhaling hard enough for dry powder inhalers. A spacer can make a metered-dose inhaler easier. If technique is still tough, a nebulizer delivers the same medicines as an easy-to-breathe mist.
- Modern portable mesh nebulizers, like the TruNeb™ handheld device, are small, quiet, and battery powered. That can make daily treatments simpler at home or on the go.
- You might see products labeled "steam inhaler" on store shelves. These are for warm, moist air and are not meant for breathing in COPD medications.
Corticosteroids and other COPD medicines
- Inhaled corticosteroids can cut flare-ups in moderate to severe COPD. Rinse your mouth after each use to help prevent thrush and hoarseness.
- Some inhalers combine bronchodilators and inhaled steroids in one device. These combination inhalers can simplify routines for seniors who find multiple inhalers hard to manage.
- Short courses of oral prednisone can calm a flare, but long use can raise blood sugar, weaken bones, or affect mood and sleep.
- Some people benefit from roflumilast for chronic bronchitis. Theophylline is rarely used now and needs blood level checks. A few patients with frequent infections get preventive azithromycin under specialist care.
Managing side effects and multiple medications
- Keep an updated medication list for every appointment.
- Ask for an inhaler technique check at least once a year.
- Use a pill organizer and simple alarms to avoid missed doses.
- Report tremors, racing heart, thrush, sleep changes, or mood shifts. Don’t stop a medicine suddenly without medical advice.
Safety note: Talk to your doctor before trying a new medication or changing how you take one.
Key takeaway: The best device is the one you can use correctly every time.
Inhaler vs nebulizer for seniors with COPD: choose the device you can use correctly every time. This quick comparison covers breathing effort, ease of use, portability, medicines, and cleaning.
| Device | Breath needed | Setup & use | Portability & noise | Medicines delivered | Cleaning |
|---|---|---|---|---|---|
| Metered-dose inhaler (MDI) + spacer | Slow, steady breath; timing helped by spacer | Shake inhaler, attach spacer, press-and-breathe | Pocket-size; quiet | Most short- and long-acting bronchodilators; some inhaled steroids | Rinse spacer regularly; follow device instructions |
| Dry powder inhaler (DPI) | Strong, quick inhale to pull powder in | Load capsule or click device, then inhale forcefully | Pocket-size; no propellant; quiet | Selected long-acting bronchodilators and some steroids as powders | Keep dry; wipe mouthpiece |
| Mesh nebulizer | Gentle, normal breathing | Pour prescribed solution, turn on, breathe via mouthpiece or mask for several minutes | Small, battery powered; very quiet | Liquid bronchodilators, inhaled steroids, or saline if prescribed | Rinse after each use; disinfect as directed |
Note: Steam inhalers make warm mist only and aren’t for delivering COPD medications.
Oxygen Therapy for Older Adults With COPD
Supplemental oxygen helps when blood oxygen stays low. It can improve energy, mood, sleep, and in the right patients, even survival.
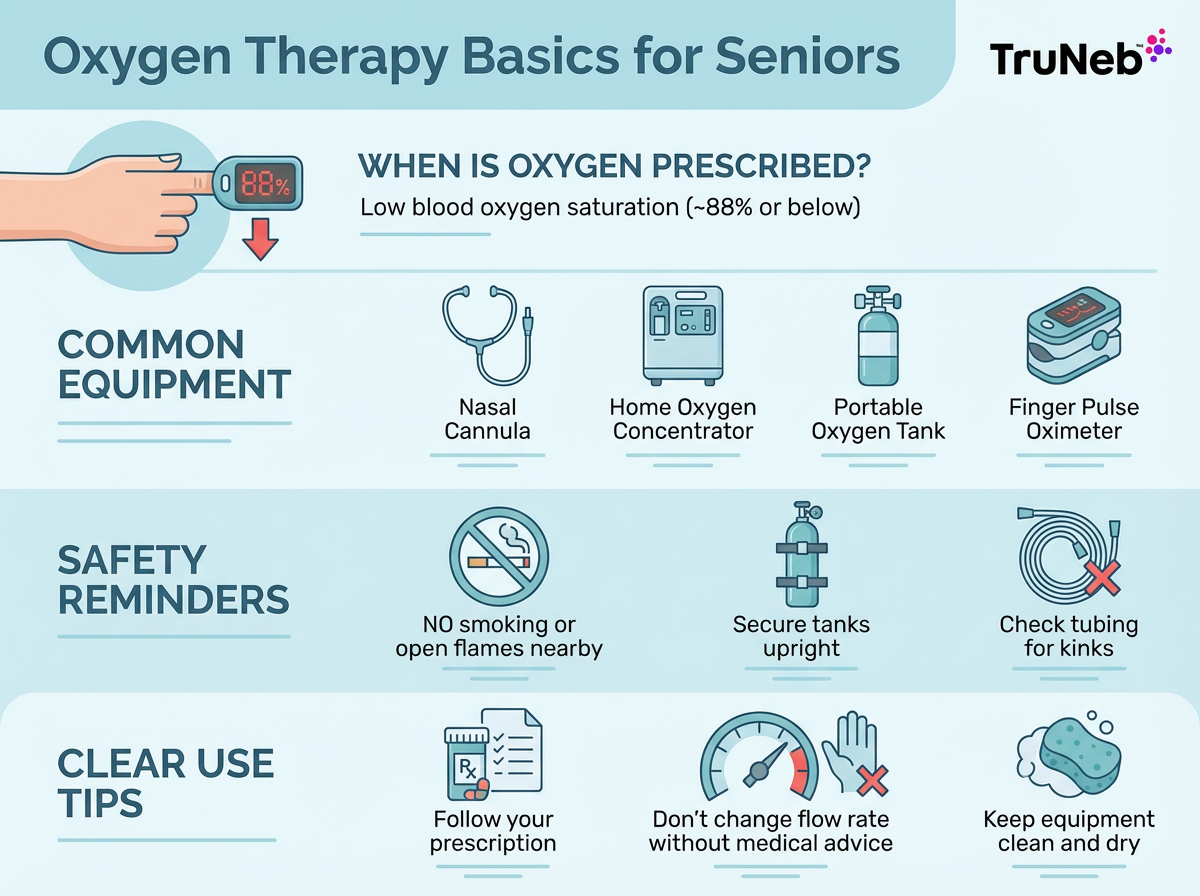
When oxygen is prescribed
- Doctors usually use a resting oxygen saturation of about 88% or lower on room air as a general guide. They also check levels during walking or sleep.
How oxygen helps
- It reduces strain on the heart, eases shortness of breath with activity, and helps you stay more active.
Ways to use it
- Home oxygen concentrator for daily use and smaller portable tanks or portable concentrators for outings. Most people use a soft nasal cannula.
Daily tips and safety
- Wear oxygen as prescribed, including during sleep and activity if it’s part of your plan. Manage tubing to prevent tripping. Keep oxygen away from flames and smoking.
Advanced support
- Some people with CO2 retention use noninvasive ventilation (like BiPAP) at night to support breathing.
Key takeaway: Home oxygen is typically considered when oxygen saturation stays around 88% or lower on room air.
Pulmonary Rehabilitation and Exercise for Seniors With COPD
Pulmonary rehab is a supervised program that teaches you how to move, breathe, and live better with COPD.
What rehab includes
- Exercise training: gentle, tailored workouts to build endurance and strength.
- Breathing training: pursed-lip and diaphragmatic breathing to control breathlessness.
- Education and support: medication skills, nutrition tips, and coping tools.
Why it helps
- Even in your 70s or 80s, rehab can reduce shortness of breath, improve walking distance, and lower hospital visits. Plenty of people feel more confident after completing a program.
Getting started
- Ask your doctor for a referral. In the U.S., Medicare covers pulmonary rehab for COPD, and other regions have similar programs. Programs adjust exercises if you have arthritis, heart disease, or balance issues so workouts stay safe.
Key takeaway: Pulmonary rehab builds strength, eases breathlessness, and can reduce hospital visits.
Preventing COPD Flare Ups in Older Adults
Preventing flare-ups (also called exacerbations) protects your lungs and your independence.
Vaccines and infection prevention
- Stay current on flu, pneumococcal, and COVID-19 vaccines. Wash hands regularly and consider a mask in crowded indoor spaces during peak virus seasons.
Quit smoking
- If you smoke, quitting helps at any age. Ask about nicotine replacement, counseling, or support groups.
Avoid irritants
- Limit secondhand smoke, heavy air pollution days, and poorly ventilated wood fires.
Keep airways clear
- Staying well hydrated can help thin mucus. If you have heart or kidney problems, ask your doctor how much fluid is right for you. Practice huff coughing to move mucus. Ask your doctor or respiratory therapist about airway tools if mucus is a daily problem.
About hypertonic saline
- Some clinicians use 3% or 7% hypertonic saline by nebulizer for very thick mucus, especially when bronchiectasis overlaps. Use this only if your doctor recommends it.
Have an action plan
- Ask for a written COPD action plan for early symptoms. Some people keep a rescue pack of medicines at home and call the clinic when they start it.
- ⚠️ If you or your loved one has severe shortness of breath at rest, chest pain, confusion, blue lips or fingers, or can’t speak in full sentences, seek emergency medical care right away (call 911 in the U.S.).
Check in and monitor
- Regular visits catch small changes early. A simple pulse oximeter at home can help you and your caregiver spot when oxygen is lower than your usual. If your oxygen level is much lower than your usual reading or doesn’t improve with your usual treatments, call your doctor or urgent care promptly.
Safety note: Talk to your doctor before trying hypertonic saline or changing any medication.
Key takeaway: Act early on flare signs to stay stable and avoid the hospital.
Making Life Easier With COPD at Home
Small changes at home can lower stress and save energy.
Nutrition
- If weight is low, try small, frequent, high-protein meals or smoothies. If weight is high, aim for gentle weight loss that preserves muscle. Ask about a dietitian.
Daily movement
- On non-rehab days, short walks, light stretches, or chair exercises can help you stay active. Ask your doctor what level of activity is safe for you, and use oxygen during activity if it’s part of your plan.
Energy and safety
- Sit for tasks like showering or cooking. Keep essentials within easy reach. Use grab bars, a walker with a seat, or a shower chair if needed. Clear tripping hazards, especially if you use oxygen tubing.
Home air quality and backup
- Avoid indoor smoke. Keep humidifiers clean. If you use a concentrator, plan for power outages and ask your power company about medical priority.
Mind and mood
- Anxiety and low mood are common. Breathing techniques, support groups, and counseling can help. Caregivers need breaks and support, too.
Planning ahead
- Talk about care wishes before a crisis. Palliative care can join early to ease symptoms and support the family.
Key takeaway: Simple routines and smart home setups make COPD more manageable day to day.
FAQs on COPD Treatment for Seniors
Key takeaway: These quick answers give you fast, plain-language guidance on common questions about COPD treatment in older adults.
Tap or click a question below to see the answer:
The best device is the one you can use correctly and consistently.
- Spacers make metered-dose inhalers easier.
- Dry powder inhalers need a strong, quick breath.
- If technique is hard or lungs are very tight, a nebulizer is usually the simplest option because you just breathe normally.
- Portable mesh nebulizers are quiet and easy to carry.
Oxygen is based on blood oxygen levels, not stage. Doctors usually prescribe it if your oxygen saturation stays around 88% or lower on room air, following standard COPD guidelines (such as GOLD).
Your doctor can test levels at rest, while walking, and during sleep. See the oxygen therapy section above.
Common ones include tremors or a fast heartbeat from some bronchodilators, dry mouth, thrush or hoarseness with inhaled steroids, and mood or sleep changes with oral steroids.
- Rinse after inhaled steroids to lower thrush risk.
- Tell your doctor about side effects so your plan can be adjusted.
- Don’t stop your medicines suddenly without talking to your doctor.
Focus on simple systems, clean air, and early action.
- Use a pill organizer and reminders; keep an updated medication list.
- Check inhaler or nebulizer technique and keep a simple symptom log.
- Remove smoke and irritants; improve home safety and plan power backup if oxygen is used.
- Learn the written COPD action plan and go to visits together.
- Support mood and energy with light activity, breathing techniques, and breaks for caregivers.
Some seniors with severe emphysema might be candidates for lung volume reduction surgery or endobronchial valves. Lung transplant is rare at advanced ages. A specialty team makes these decisions, so talk with your pulmonologist about whether evaluation makes sense.
It varies widely. Severity, number of flare-ups, activity level, and other health conditions matter more than age alone. Focus on prevention, staying active, and the right treatments to help both quality and length of life.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk to your doctor about your symptoms, diagnosis, and treatment options before making changes to your care.