On this page
The Bottom Line – RSV and Pneumonia Can Occur Together
Yes. You can have RSV and pneumonia at the same time.
RSV is a virus that infects your airways. Pneumonia is an infection in the tiny air sacs of your lungs. RSV can cause viral pneumonia by moving into the lungs. It can also weaken your defenses, which lets bacteria cause a second lung infection.
When RSV infects the lungs, doctors usually call it RSV pneumonia.
This is why some people feel worse after a few days of RSV, not better. Babies, older adults, and people with lung or immune problems are at higher risk.
Key Takeaway: Yes, RSV can cause pneumonia, so RSV and pneumonia can occur together.
Understanding RSV vs. Pneumonia
Respiratory syncytial virus (RSV) is a common virus that spreads through droplets and hands. In most healthy people it looks like a bad cold. In babies and older adults, it can move into the lower lungs.
Pneumonia is a lung infection. The air sacs fill with fluid or pus, making it hard to breathe and get oxygen. Pneumonia is a condition, not a single germ—several types of germs can cause it: viruses like RSV or the flu, and bacteria like pneumococcus.
According to the CDC, RSV can lead to serious lung infections like bronchiolitis and pneumonia, especially in babies and older adults.
Key difference: RSV is a cause; pneumonia is the result in the lungs.
| Condition | What it is | Contagious? | Typical symptoms | Treatment focus |
|---|---|---|---|---|
| RSV | A respiratory virus | Yes | Runny nose, cough, wheeze, low fever | Supportive care; breathing support if needed |
| Pneumonia | Infection in the lung air sacs | Depends on cause | Higher fever, fast or hard breathing, chest pain | Supportive care; doctors use antibiotics for bacterial pneumonia |
RSV is the virus; pneumonia is the lung infection it can cause. Care focuses on supporting breathing, and antibiotics are only used for bacterial pneumonia.
Key Takeaway: RSV is a virus; pneumonia is the lung infection it can cause.
- RSV is a virus; pneumonia is an infection in the lung air sacs.
- RSV can cause pneumonia; pneumonia can be viral or bacterial.
- Antibiotics treat bacterial pneumonia, not RSV.
- In infants, RSV often causes bronchiolitis first; pneumonia occurs if infection reaches the air sacs.
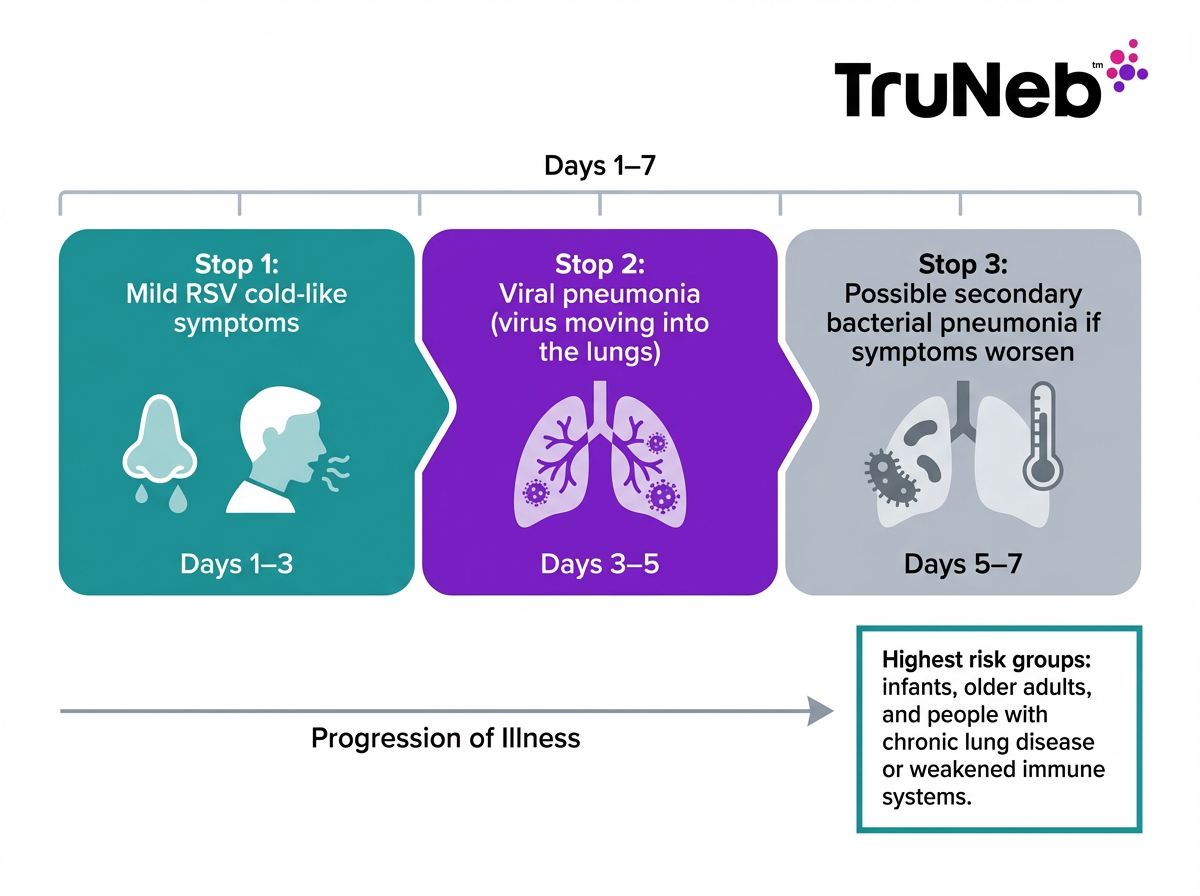
How RSV Infection Can Lead to Pneumonia
There are two main paths:
- Viral pneumonia from RSV: The virus spreads from the upper airways into the lungs and inflames the air sacs.
- Secondary bacterial pneumonia: RSV irritates and weakens the airways. Bacteria can then move in and cause a second lung infection on top of RSV.
In infants, RSV usually causes bronchiolitis first. If the infection reaches the air sacs, it becomes pneumonia. Nearly one-third of hospitalized children with RSV pneumonia have a bacterial co-infection.
Pneumonia can develop during the illness or soon after, especially if symptoms worsen around days 3 to 5.
Key Takeaway: RSV can directly inflame the lungs or open the door to bacteria that cause pneumonia.
Infographic: RSV to Pneumonia Timeline
Who Is Most at Risk for RSV Turning Into Pneumonia
Anyone can get pneumonia from RSV, but some groups face higher risk.
Babies and Young Children
- Highest risk under 1 year, especially premature babies or those with heart or lung problems.
- Small airways and immature immunity make breathing issues develop fast.
- RSV is one of the most common causes of pneumonia and hospital stays in babies under 1.
Older Adults
- Risk rises after age 65. Many have other conditions (heart disease, diabetes) that make recovery harder.
- RSV can go to the chest and become pneumonia more easily in this group.
- Yes, RSV can turn into pneumonia in adults, especially those 65 and older or with other health problems.
Chronic Lung Conditions or Weakened Immunity
- Asthma, COPD, bronchiectasis, and cystic fibrosis can flare with RSV and lead to pneumonia.
- Cancer treatment, transplants, or other immune problems increase risk and can mute early signs.
- In these groups, RSV can move to the lungs and become pneumonia more quickly, and early signs might be subtle.
Tip for chronic lung patients: If your doctor has prescribed inhaled meds, follow the plan they've given you. A portable mesh nebulizer like TruNeb can help deliver bronchodilators or 3–7% hypertonic saline to thin mucus and support airway clearance. This does not cure RSV or pneumonia. Use only as directed by your doctor.
Key Takeaway: Babies, seniors, and people with lung or immune issues are most likely to develop pneumonia from RSV.
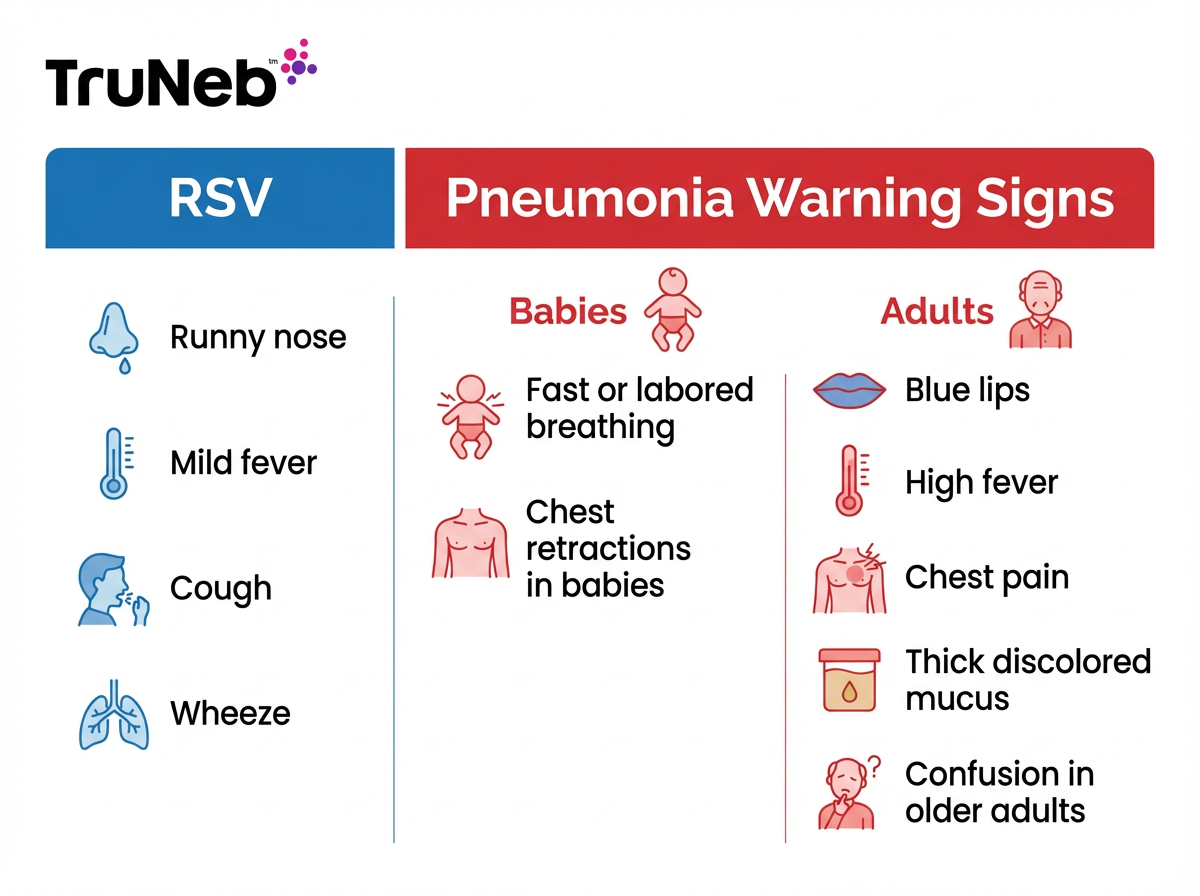
Warning Signs RSV May Have Turned Into Pneumonia
RSV and pneumonia share cough and fever. These red flags are key RSV pneumonia symptoms that suggest the infection has moved into the lungs. Watch for these signs if RSV symptoms suddenly get worse after the first few days.
In Babies and Young Children
- Fast or hard breathing (about 60 breaths per minute or more in infants).
- Chest retractions (skin pulling in between or under the ribs), nasal flaring, or grunting.
- Blue or gray lips or face.
- High fever that persists or spikes after a few days.
- Poor feeding, fewer wet diapers, or dry mouth.
- Lethargy or trouble waking.
In Older Children and Adults
- High fever and chills.
- Chest pain with breathing or coughing.
- Worsening cough with thick, discolored mucus, sometimes with blood.
- Shortness of breath at rest or with light activity.
- Confusion, dizziness, or new weakness (common in seniors).
If you see these signs, it’s time to have a doctor check you or your child.
Key Takeaway: New or worsening breathing trouble, high fever, chest pain, or blue lips are red flags for pneumonia.
Infographic: RSV vs Pneumonia Warning Signs
When To Seek Medical Attention
Getting help at the right time can prevent complications. Here’s how to know when to call your doctor or go to the ER.
Call your doctor if:
- Fever or cough is getting worse after 3 to 4 days.
- You notice early warning signs (mild shortness of breath, poor feeding in a baby).
- The person is high risk (infant, older adult, chronic lung disease, or a weakened immune system).
- You are unsure and need guidance.
⚠️ If breathing looks hard or very fast, or lips turn blue, seek emergency care right away.
If a baby, older adult, or someone with lung disease has any of the ER warning signs, don’t wait—go in right away.
Go to the emergency room now if:
- Breathing is hard, fast, or the person is gasping.
- Lips or face turn blue.
- There is chest pain, severe weakness, or confusion.
- Fever is very high, or an infant under 3 months has a fever.
- There are signs of severe dehydration (no urine for 8 hours, very dry mouth).
If in doubt, seek care. A chest X-ray and oxygen check can help confirm pneumonia and guide treatment.
Key Takeaway: If breathing looks hard or lips turn blue, go to the ER now.
Treatment: Managing RSV and Pneumonia
RSV pneumonia treatment focuses on supporting breathing and treating any bacterial infection if it’s present.
Home care for mild RSV:
- Mild RSV is usually managed with rest and plenty of fluids. For babies, doctors sometimes recommend breastfeeding or offering fluids more frequently.
- Some families use a cool-mist humidifier or sit in a steamy bathroom to ease congestion.
- Doctors sometimes suggest saline nose drops and gentle suction for infants’ stuffy noses.
- Your doctor can recommend safe fever reducers like acetaminophen or ibuprofen (never give aspirin to children).
Medical treatment for pneumonia:
- Supportive care: oxygen if levels are low, IV fluids if needed.
- If a bacterial infection is present, doctors treat it with antibiotics.
- Severe cases (especially in infants and older adults) can require hospitalization and breathing support.
Chronic lung disease support:
- If your doctor has prescribed bronchodilators or steroids for asthma or COPD, they’re sometimes given by nebulizer to ease breathing. A portable mesh nebulizer can help deliver these medicines, but nebulizers do not kill the virus.
Safety note: Talk to your doctor before trying a new medication or hypertonic saline.
Key Takeaway: Doctors focus on supporting breathing first and use antibiotics only when a bacterial pneumonia is confirmed.
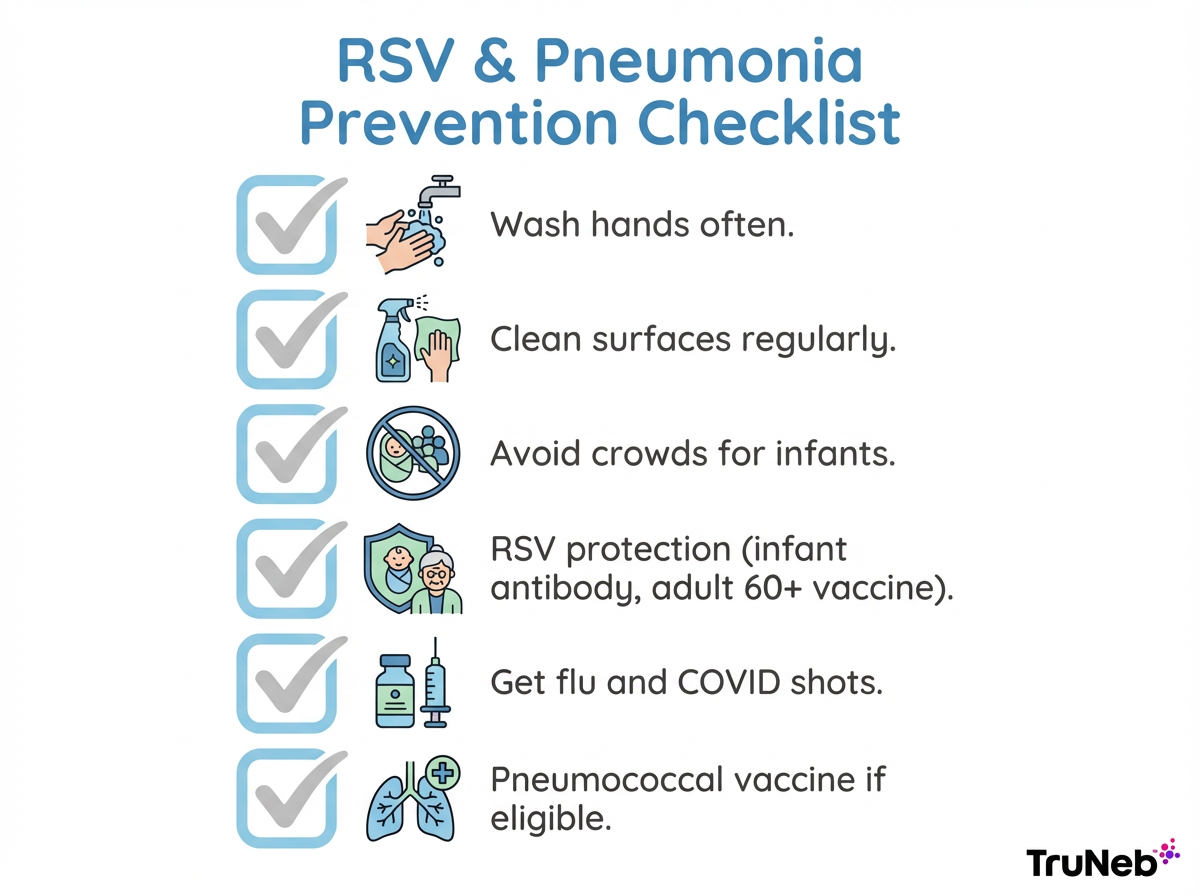
Prevention: Reduce the Risk of RSV and Pneumonia
Hygiene and exposure control:
- Wash hands regularly, clean shared surfaces, and avoid close contact when sick.
- Keep infants away from crowds during RSV season and away from smoke.
Vaccines and immunizations:
- Infants can receive a preventive RSV shot (antibody) before their first RSV season.
- Adults 60 and older can get an RSV vaccine; ask your doctor if it’s right for you.
- Stay up to date on flu and COVID-19 shots.
- If eligible, get pneumococcal vaccination to lower bacterial pneumonia risk.
Healthy lungs recover better:
- Do not smoke. Manage asthma or COPD plans with your care team.
Key Takeaway: Clean hands and the new RSV shots reduce severe illness and pneumonia risk.
Infographic: RSV and Pneumonia Prevention Checklist
Frequently Asked Questions
Tap or click a question below to see the answer:
Pneumonia can develop a few days into RSV if it is going to happen, typically around days 3 to 5 as symptoms worsen instead of improve. In high-risk people, serious lung involvement can appear within 1 to 2 days. Sometimes symptoms improve, then get worse again—this can be a sign of a secondary bacterial pneumonia.
If you’re wondering how bad RSV and pneumonia together can be, it can be very serious for infants, older adults, and people with chronic lung or immune problems. Most healthy older kids and adults recover without pneumonia, but when pneumonia occurs, hospitalization is sometimes needed. Early care improves outcomes.
Treatment focuses on supportive care—rest, fluids, and oxygen if needed. Doctors use antibiotics only when a bacterial infection is present. Severe cases can require hospital care for IV fluids or breathing support; there is no quick cure for RSV itself.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk to your doctor about your symptoms and before starting, stopping, or changing any medication or treatment.