On this page

What Is Popcorn Lung (Bronchiolitis Obliterans)?
Popcorn lung, or bronchiolitis obliterans, is a rare disease that scars and narrows your smallest airways (bronchioles) and makes breathing hard.
The name started with workers in microwave popcorn factories who breathed in diacetyl, a butter flavor chemical, and got sick. Today, doctors know several causes: breathing certain chemicals (including diacetyl in some e-cigarette flavors), a complication after a lung transplant, or after a severe lung infection or some autoimmune diseases; other harsh industrial gases like chlorine, ammonia, or nitrogen oxides can also trigger bronchiolitis obliterans.
It's rare, but it's serious. Most people with a cough or shortness of breath don't have popcorn lung, but it's important to recognize when symptoms fit this pattern.
Think of it like tiny air tubes turning into stiff, narrowed straws. Air can't flow like it used to.
Early Signs and Symptoms of Popcorn Lung
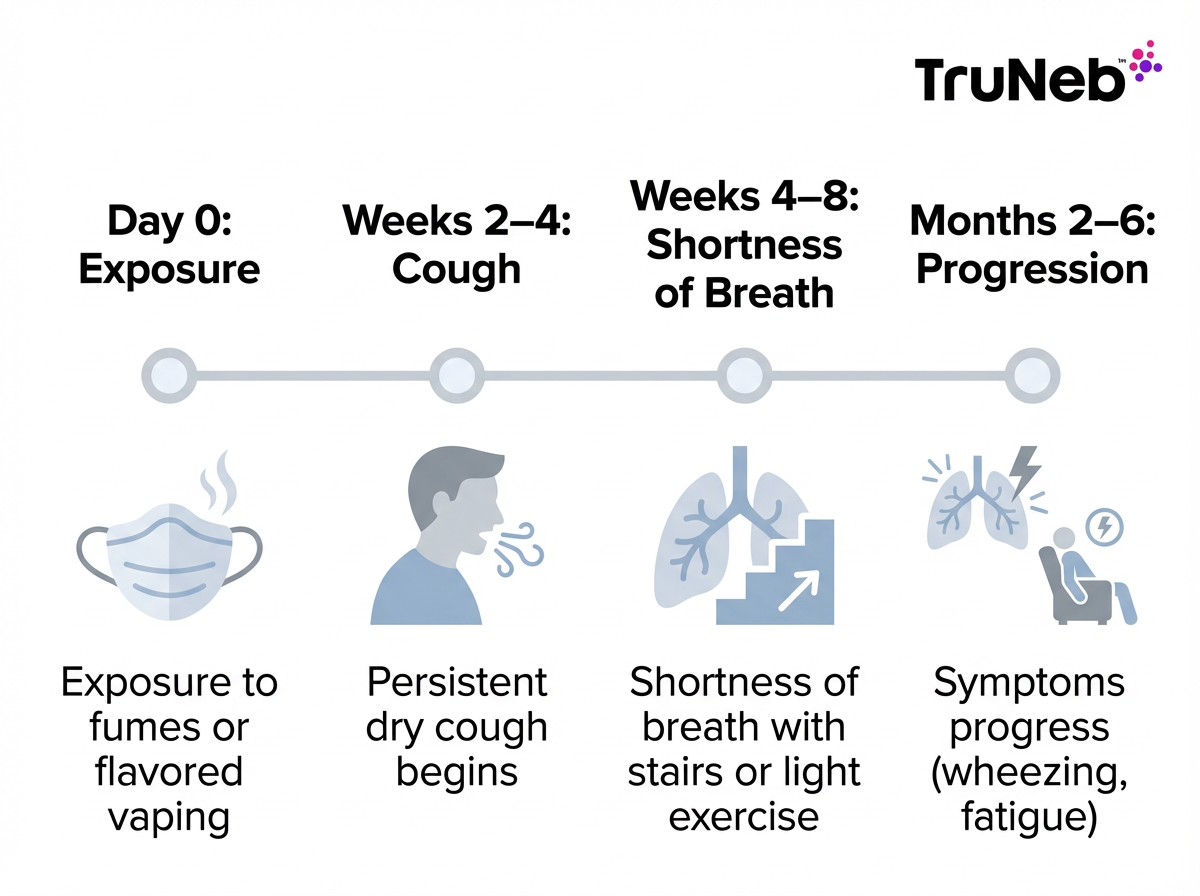
Early signs of popcorn lung usually appear 2 to 8 weeks after exposure and start with a persistent dry cough and shortness of breath during activity.
Symptoms usually start slowly. At first, you might think it's a leftover cold that just hangs on.
Common early signs include a persistent dry cough that doesn't bring up much mucus and won't go away. Shortness of breath shows up during everyday effort, like climbing one flight of stairs or walking uphill. Some people notice a soft wheeze or chest tightness after activity. Feeling more tired than normal can also appear, especially after exertion.
Early signs are more concerning when they begin soon after heavy vaping or a big fume exposure and don't fade. Track when your cough started and what makes your breathing worse. That timeline helps your doctor spot patterns early.
Worsening Symptoms and Progression of Popcorn Lung
Popcorn lung symptoms tend to get worse over weeks to months if the damage continues.
- Shortness of breath moves from effort to daily tasks, and sometimes even at rest.
- Wheezing becomes more frequent and easier to hear.
- Fatigue feels constant and limits your routine.
- Some people develop low fevers or night sweats.
- Unplanned weight loss can appear in advanced disease.
- A skin rash can occur when an underlying condition is involved.
Over time, even simple chores can leave you winded. Unlike asthma, these symptoms don't come and go; they keep building if the cause isn't removed. Severe cases can need oxygen support. In advanced cases, severe scarring can lead to respiratory failure, which can be life‑threatening.
⚠️ If you're struggling to breathe at rest, feel dizzy, or notice blue lips or face, seek emergency medical care right away.
Popcorn Lung vs Other Conditions
Popcorn lung causes chronic, steadily worsening breathing problems that don't respond well to inhalers, which helps distinguish it from asthma, bronchitis, COPD, and lung cancer.
Popcorn Lung vs Asthma
Asthma tends to come in episodes with clear triggers like allergens or cold air. People usually feel normal between flares, and quick‑relief inhalers work fast. Popcorn lung feels steady and progressive. Inhalers can help a little, but the fixed scarring means relief is limited.
Popcorn Lung vs Bronchitis and COPD
Acute bronchitis is short‑lived and usually produces mucus. Chronic bronchitis (a type of COPD) comes with years of daily, phlegmy cough in heavy smokers, with ups and downs. Popcorn lung's cough is usually dry, can appear in non‑smokers, and progresses over weeks to months after a clear exposure.
Popcorn Lung vs Lung Cancer
Popcorn lung isn't cancer. Lung cancer can cause coughing blood, chest pain, and a mass on scans. In popcorn lung, scans can show a diffuse pattern (a mosaic look) rather than a single tumor. Age and history matter: a young non‑smoker with a new dry cough after chemical exposure is less likely to have lung cancer, though lung cancer can still occur in non‑smokers, so any lasting symptoms deserve a full workup.
Popcorn lung's airflow blockage usually doesn't improve much with bronchodilator inhalers, while asthma typically does.
Key takeaway: Popcorn lung causes a steady, non‑episodic airflow obstruction that responds poorly to inhalers; asthma tends to flare and responds well. History and imaging help tell them apart.
| Condition | Cough | Pattern | Typical triggers/history | Response to inhaler | Imaging/testing clue |
|---|---|---|---|---|---|
| Popcorn lung (bronchiolitis obliterans) | Usually dry | Chronic, steadily worsens | Chemical fumes or flavored vaping; transplant, severe infection, autoimmune disease | Poor or limited response | HRCT “mosaic” air‑trapping; obstructive PFT that doesn't normalize |
| Asthma | Dry or with scant mucus | Episodic flares with symptom‑free periods | Allergens, cold air, exercise | Good response to bronchodilators | Normal imaging between attacks; reversible obstruction on PFT |
| Chronic bronchitis/COPD | Daily, phlegmy | Chronic with ups and downs | Long smoking history or biomass exposure | Partial response | Hyperinflation; fixed obstruction on PFT |
| Acute bronchitis | Temporary, typically with mucus | Short‑lived, post‑infection | Recent viral illness | Symptomatic relief only | No specific imaging findings; resolves over weeks |
| Lung cancer | Variable; can include coughing blood | Progressive | Age, smoking history; can occur in non‑smokers | No consistent relief | Discrete mass or nodule on imaging |
This table is a quick comparison, not a diagnosis. Talk to your doctor about your specific symptoms and tests.
How Doctors Diagnose Popcorn Lung
Doctors confirm popcorn lung with breathing tests, high‑resolution CT scans, and sometimes bronchoscopy or biopsy.
Your doctor starts with your story: when the cough began, any vaping or chemical exposure, and how your breathing has changed. A pulmonologist usually coordinates these tests.
Pulmonary function tests (like spirometry) check how fast and how much air you blow out. In popcorn lung, results show obstructed flow that doesn't improve much after a bronchodilator. A high‑resolution CT scan gives a close look inside your lungs; it can show a mosaic pattern that suggests uneven airflow.
If needed, a pulmonologist can perform bronchoscopy to look inside the airways and collect samples. In some cases, a lung biopsy confirms the scarred, narrowed bronchioles that define bronchiolitis obliterans.
Is Popcorn Lung Curable? Treatment and Management
Popcorn lung is not reversible, but treatment can help symptoms and slow further damage.
There is no cure for popcorn lung. The scarring in the bronchioles can't be undone. But there are ways to help you breathe better and protect the lung function you have.
First, your doctors will focus on removing the cause. That usually means stopping exposure to the chemical that started it. Medications like corticosteroids can calm inflammation, especially early on or in certain causes. Inhaled bronchodilators and sometimes inhaled steroids can open airways and ease tightness. Some people need oxygen at home, particularly during activity or sleep. Pulmonary rehab teaches breathing techniques and safe exercise. In the most severe cases, lung transplant might be considered.
Some people stabilize and live with manageable symptoms for years, while others with advanced damage can keep getting worse even with treatment.
Safety note: Talk to your doctor before trying a new medication.

Living With Popcorn Lung
Daily habits and prescribed inhaled treatments can help you breathe easier and stay active.
Follow your care plan closely. Take medicines exactly as prescribed and keep regular checkups with your pulmonologist.
Protect your lungs day to day: avoid smoke, dust, and chemical fumes as much as possible, and stay up to date on flu and pneumonia vaccines.
People use inhaled therapies at home. Only use nebulized bronchodilators or saline if your doctor has prescribed them for you; sometimes a stronger salt solution (hypertonic saline) is used if your doctor recommends it. For convenience, some people use a portable mesh nebulizer such as TruNeb™ to take their breathing treatments at home or on the go. It's a tool to deliver medicine or saline; it's not a cure. ⚠️ Don't use a steam inhaler for prescription nebulizer medicines. Steam devices aren't designed to deliver these treatments safely.
Pulmonary rehab can teach breathing techniques and safe exercise so you can do more with less breath. Support groups and stress-management practices can also make daily life easier. Talk to your doctor if your symptoms get worse, or before changing how you use your inhalers or nebulizer.
When to Seek Medical Attention
Don't ignore a cough and breathlessness that linger for weeks, especially after chemical exposure.
See a doctor if a dry cough and shortness of breath last more than a few weeks, or keep getting worse. This is especially important if you vape, work around flavoring chemicals, or recently had a severe lung infection. Early care can slow damage.
⚠️ Call emergency services or go to the ER right away if:
- You're having severe trouble breathing at rest or struggling to speak full sentences.
- Your lips or face turn blue, or you feel dizzy, confused, or have chest pain.
- You cough up blood.
If asthma medicines aren't helping and symptoms persist, ask for a referral to a pulmonologist. Bring your exposure history with you.
Frequently Asked Questions
Tap or click a question below to see the answer:
The early signs of popcorn lung are a persistent dry cough and shortness of breath during activity, usually starting 2 to 8 weeks after an exposure.
Yes. Exposure to diacetyl in some flavored e-liquids has been linked to popcorn lung; cases tied to vaping are rare but reported. If you vape and develop a chronic cough or breathlessness, see a doctor.
No. The airway scarring isn't reversible; treatment can help symptoms and sometimes slows further damage.
Doctors confirm popcorn lung with breathing tests, a high-resolution CT scan, and sometimes bronchoscopy or lung biopsy, along with your exposure history.
They're the same as popcorn lung symptoms described above: a long-lasting dry cough, worsening shortness of breath, wheezing, and fatigue.
The term comes from microwave popcorn factory workers who developed bronchiolitis obliterans after breathing diacetyl.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about any questions you have about your health or before starting or changing any treatment.