On this page
What Is Pleurisy?
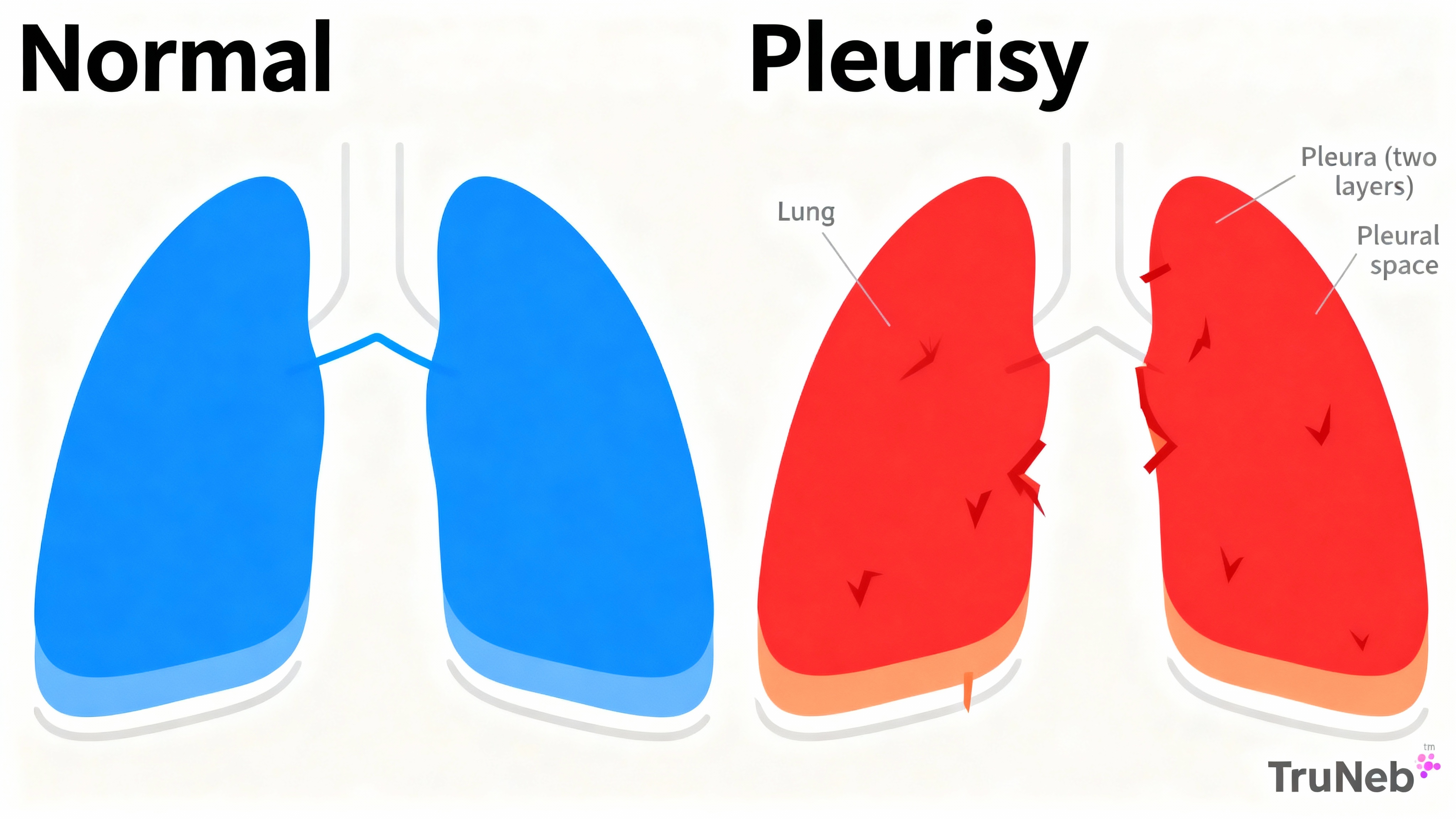
Pleurisy (also called pleuritis) is inflammation of the pleura, the thin two-layer lining around your lungs and chest wall. When inflamed, the layers rub and cause sharp chest pain that gets worse when you breathe, cough, or sneeze. Pleurisy causes pleuritic chest pain—sharp pain that worsens when you breathe in.
Normally, a few drops of fluid let the pleura glide smoothly. With pleurisy, that smooth glide is lost, so every deep breath can feel scratchy or stabbing. Doctors sometimes record pleurisy as ICD-10 code R09.1.
Key takeaway: Pleurisy is inflammation of the lung lining that causes pleuritic chest pain—sharp pain that gets worse when you breathe in.
Signs and Symptoms of Pleurisy
The hallmark sign is pleuritic chest pain—sharp, stabbing chest pain that gets worse with deep breaths, coughing, or sneezing. It usually affects one side of your chest.
Common symptoms:
- Sharp chest pain that worsens with breathing or coughing
- Shallow, quick breaths to avoid pain
- Shortness of breath (especially if pain limits deep breaths)
- Cough (dry or with mucus if an infection is involved)
- Fever and chills when an infection is the cause
A doctor can sometimes hear a "pleural friction rub" with a stethoscope. If fluid builds up (pleural effusion), pain can lessen but breathing can feel heavy or harder. Pain can radiate to your shoulder or back, especially when the diaphragm is involved.
Key takeaway: If chest pain spikes when you inhale or cough, that pleuritic pattern points to pleurisy.
Causes of Pleurisy
Pleurisy happens when something inflames the pleura. Common causes include:
- Infections
- Viral infections like influenza or COVID-19 can inflame the lining.
- Bacterial pneumonia is a frequent cause. Tuberculosis can also trigger pleurisy.
- Autoimmune diseases
- Rheumatoid arthritis and lupus (SLE) can inflame the pleura during a flare.
- Blood clots in the lungs (pulmonary embolism)
- A clot near the pleura can cause pleuritic pain.
- Chest injury or surgery
- Trauma or recent operations can irritate the lining.
- Cancer
- Lung cancer or cancer spreading to the pleura can cause pain or fluid buildup.
You’re more likely to develop pleurisy after a recent respiratory infection or if you live with conditions like lupus or rheumatoid arthritis; smoking raises the risk of lung problems that can lead to pleurisy.
Is pleurisy contagious? Pleurisy itself isn’t contagious; infections that cause it can be.
Key takeaway: Pleurisy is a reaction to another problem—most commonly infections, autoimmune flares, blood clots, injury, or cancer.
| Cause | What’s happening | Typical care |
|---|---|---|
| Viral infection (flu, COVID‑19) | Virus inflames the pleura | Rest; NSAIDs or other pain relievers; antivirals only when indicated† |
| Bacterial pneumonia | Lung infection irritates pleura | Antibiotics; pain control; monitor for effusion |
| Tuberculosis (TB) | TB involves lung/pleura | Multi‑drug anti‑TB regimen; drain fluid if needed |
| Autoimmune flare (RA, lupus) | Immune‑mediated pleural inflammation | Adjust disease therapy; corticosteroids as directed |
| Pulmonary embolism | Clot near pleura causes infarction | Anticoagulation and PE management in hospital |
| Chest injury or surgery | Pleura irritated by trauma/procedure | Pain control; time to heal; monitor for complications |
| Cancer‑related | Tumor or malignant effusion | Cancer therapy; drain fluid; consider pleurodesis if recurrent |
† Antivirals are prescribed only for specific viruses and timing at a clinician’s discretion. Care plans vary by diagnosis.
How Is Pleurisy Diagnosed?
A doctor starts with your symptoms and exam. A doctor can sometimes hear a pleural friction rub with a stethoscope. Tests help confirm the cause and check for fluid.
Common tests:
- Chest X-ray to look for pneumonia or pleural effusion
- Ultrasound to detect even small amounts of pleural fluid
- CT scan if the diagnosis is unclear or to check for clots or tumors
- Blood tests for infection or autoimmune clues
- Thoracentesis if fluid is present (a needle removes fluid for testing and sometimes relief)
Doctors also rule out other causes of chest pain, like heart attack or pericarditis, especially if symptoms overlap.
Key takeaway: Doctors confirm pleurisy by matching your symptoms with exam findings and imaging, and sometimes by testing pleural fluid.
Treatment and Management of Pleurisy
Treatment focuses on relieving pain and fixing the root cause.
Medical treatments:
- Pain relief: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can reduce pain and inflammation. Acetaminophen can help with pain or fever. Severe pain might need prescription options.
- Treat the cause: Antibiotics for bacterial pneumonia; specific TB medicines for tuberculosis; corticosteroids or other adjustments for autoimmune flares; blood thinners for pulmonary embolism; cancer-directed therapy when needed.
- Drainage: If a pleural effusion is large or infected (empyema), doctors can remove fluid with a needle or place a tube.
Home care tips:
- Rest and pace yourself
- Try lying on the painful side to splint the chest and ease breathing
- Your doctor might recommend gentle deep-breathing exercises as tolerated to keep lungs open
- Stay well hydrated and avoid smoke exposure
- Use medicines exactly as prescribed and finish antibiotic courses
If you also have airway symptoms like wheezing from another condition, your doctor might suggest inhalers or a nebulizer to deliver medication. A portable mesh nebulizer can deliver prescription medication as a fine mist when your doctor recommends it.
Key takeaway: Relieve pain, treat the underlying cause, and use simple comfort steps to protect your breathing.
⚠️ Safety Note
- Chest pain needs medical evaluation.
- Seek emergency care now for crushing chest pain; chest pain with sweating, nausea, or pain spreading to your arm or jaw; severe shortness of breath; coughing up blood; or if you suspect a blood clot.
- See a doctor promptly for new chest pain, high fever, worsening shortness of breath, or if pain doesn’t improve after a few days.
- Talk to your doctor before starting or changing any medication.
- Don’t start, stop, or change prescription treatments on your own. Your care plan depends on the cause.
Outlook, Complications, and Prevention
Most people improve once the cause is treated. Viral pleurisy often eases within about a week; bacterial cases typically improve over 1–2 weeks after antibiotics. Autoimmune or cancer-related pleurisy can take longer and can come and go.
Possible complications:
- Pleural effusion (fluid buildup) that can need drainage
- Empyema (infected fluid) needing antibiotics and drainage
- Shallow breathing from pain, which can lead to atelectasis if lungs aren’t expanded
Prevention
- Get recommended vaccinations (flu, pneumococcal).
- Treat respiratory infections early.
- Don’t smoke; avoid secondhand smoke.
- Manage chronic conditions to reduce flares.
- Practice hand hygiene during respiratory virus season.
Key takeaway: With timely care, pleurisy usually improves in days to weeks; prevention focuses on avoiding lung infections and managing chronic conditions.
Frequently Asked Questions
Tap or click a question below to see the answer:
No. Pleurisy itself isn’t contagious. But some causes, like the flu or tuberculosis, can spread from person to person.
It varies. Most cases improve in a few days to two weeks after the cause is treated. Autoimmune or cancer-related pleurisy can last longer or recur.
Mild viral pleurisy sometimes resolves with rest and pain control. Still, it’s important to see a doctor to rule out bacterial infection or other serious causes.
Pneumonia is an infection of the lung tissue. Pleurisy is inflammation of the lining around the lungs. Pneumonia can cause pleurisy. Treatment targets the infection and the pain.
Many people feel better lying on the painful side. It can reduce movement of that side of the chest and make breathing less painful.
Disclaimer: This article is for informational purposes only and isn’t a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms and care.