On this page
What Is Negative Pressure Breathing? How Your Lungs Naturally Pull Air In
Negative pressure breathing is how you breathe right now. When you inhale, your diaphragm moves down and your ribs lift. Your chest cavity (thoracic cavity) gets bigger, the pressure inside your chest drops below the air outside, and air is pulled into your lungs.
Think of pulling back on a syringe: the space increases and fluid is drawn in. Your chest works the same way with air. When you exhale, your muscles relax, your chest gets smaller, the pressure rises, and air flows out.
Humans and other mammals use negative pressure to breathe. Frogs are different. They push air into their lungs by "gulping" it in.
In medical settings, this normal process is sometimes called negative pressure ventilation because your chest creates a slight vacuum to draw air in.
Key takeaway: In negative pressure breathing, your chest expands, pressure inside drops, and air is pulled into your lungs.
Positive Pressure Ventilation: How a Ventilator Pushes Air Into Your Lungs
Positive pressure ventilation is breathing support delivered by a device. Instead of your chest pulling air in, a ventilator pushes air into your lungs at a higher pressure than the air around you. This is the opposite of normal negative pressure breathing, where your chest muscles pull air in.
How it works:
- During a breath, the device raises airway pressure and drives air into your lungs (like blowing up a balloon).
- During positive pressure ventilation, the pressure inside the chest (intrathoracic pressure) rises above the pressure outside.
- Ventilators can also keep a little pressure in the lungs at the end of a breath (PEEP) to help keep air sacs from collapsing.
- When the push stops, your lungs recoil and air flows out.
Common ways it’s used:
- Invasive: a breathing tube in your windpipe (intubation) connects to a ventilator in the ICU or during surgery.
- Non-invasive: tight masks (CPAP/BiPAP) push air without a tube.
- Manual: during CPR, a bag-valve mask is squeezed by hand to push air in.
Key takeaway: Positive pressure ventilation uses a device to push air into your lungs when you can’t breathe well enough on your own.
Negative vs Positive Pressure Breathing: Key Differences
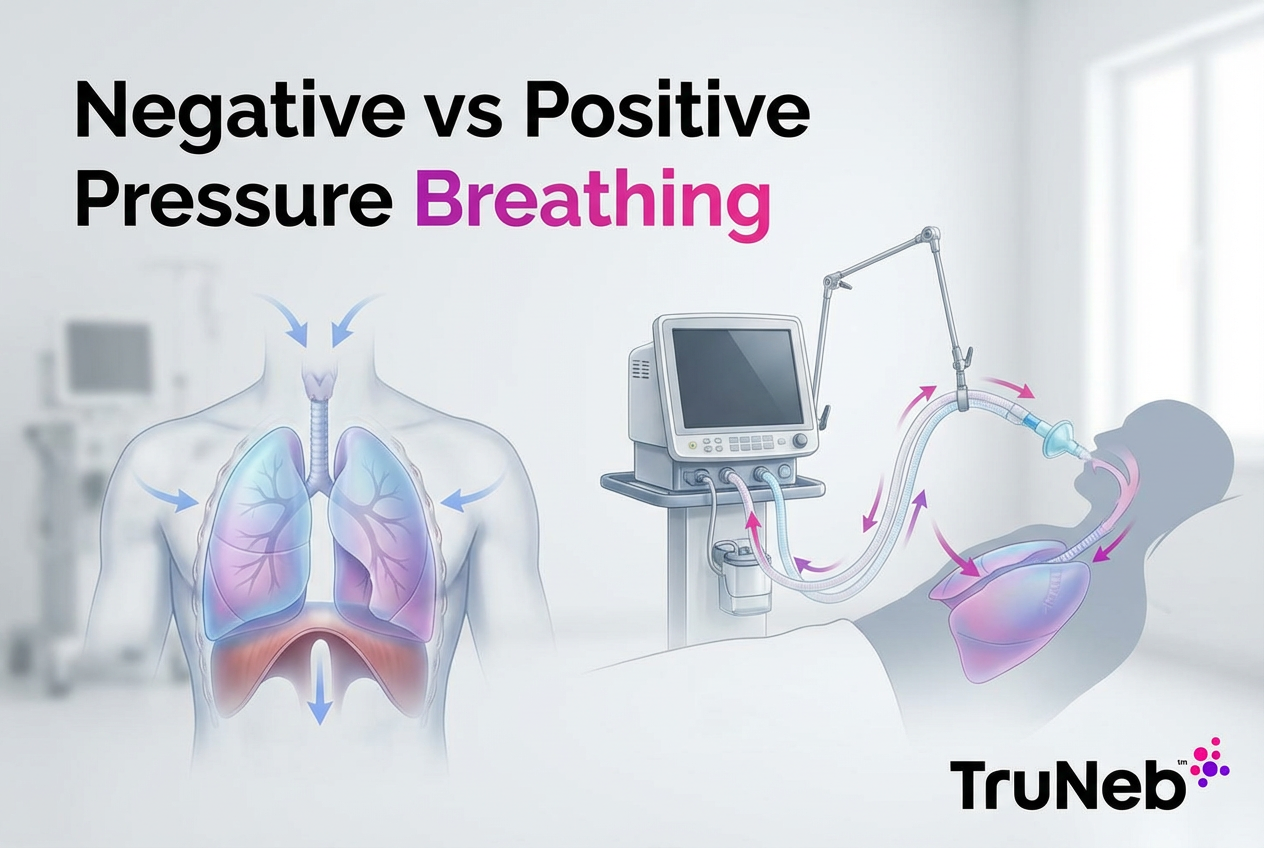
Here’s a quick look at what our infographic shows: how normal negative pressure breathing compares with positive pressure ventilation (breathing with a ventilator). When people ask about negative vs positive pressure ventilation, they’re really asking how normal breathing compares to breathing with a ventilator.
The core difference between positive and negative pressure ventilation is whether your chest pulls air in or a machine pushes it in.
Key takeaway: Negative pressure breathing pulls air into your lungs as your chest expands, while positive pressure ventilation pushes air in by raising airway pressure with a machine.
Negative pressure pulls air in; positive pressure pushes air in. This table summarizes the key differences.
| Feature | Negative pressure breathing | Positive pressure ventilation |
|---|---|---|
| Who moves the air | Your diaphragm and chest muscles | A ventilator or device |
| Pressure change in chest | Pressure inside the chest (intrathoracic) falls below outside air | Pressure inside the chest rises above outside air |
| Result | Air is pulled into the lungs as the chest expands | Air is pushed into the lungs as the machine raises airway pressure |
| Common devices/examples | None needed for healthy breathing; rare devices like iron lung/cuirass | Ventilator via tube (intubation), CPAP/BiPAP mask, bag‑valve mask |
| Typical settings | Daily life, sleep | ICU, surgery, emergencies, respiratory failure |
| Airway protection | No — airway not protected | Yes with a tube — allows suctioning and reduces aspiration risk |
Notes: Research suggests negative pressure can produce more uniform lung expansion in some settings. In the 1952 Copenhagen polio epidemic, switching many patients to positive pressure via tracheostomy was associated with mortality falling from about 90% to about 25%.
When and Why Each Method Is Used: From Everyday Breaths to Life Support
Negative pressure is your daily pattern. You use it all day without thinking.
Where negative pressure ventilators show up:
- History: iron lungs helped people survive polio outbreaks. In 1952, switching many patients to tracheostomy with positive pressure was linked to a sharp drop in deaths.
- Today: chest "cuirass" shells or newer negative pressure devices are rare. They’re mostly used at home in select neuromuscular cases when the person still has some breathing drive.
Today, almost all hospital life-support uses positive pressure ventilators; negative pressure devices are niche and mostly for selected home cases.
You’ll usually see positive pressure ventilation in:
- Emergencies and the ICU: for respiratory failure from severe pneumonia or ARDS, trauma, overdose, or during CPR.
- Surgery: under general anesthesia, a ventilator breathes for you.
- Non-invasive support: CPAP/BiPAP can keep airways open (sleep apnea) or help avoid intubation in some cases.
Key takeaway: Negative pressure is how you breathe in daily life; positive pressure is used when your own breathing isn’t strong enough to keep you safe.
Pros and Cons of Negative vs Positive Pressure Breathing
Negative pressure — benefits:
- Natural blood flow: supports normal venous return to the heart.
- Gentler lungs: lower risk of pressure-related injury; research suggests more even inflation in some situations.
- No tube in select NPV: can avoid deep sedation at home.
Negative pressure — drawbacks:
- Limited in crises: not strong enough when lungs are very stiff or weak.
- Practical limits: devices are bulky, seals can be uncomfortable, and they don’t protect the airway.
Positive pressure — benefits:
- Life-saving: delivers oxygen and ventilation when you can’t.
- Precise control: rate, volume, oxygen, and PEEP are adjustable.
- Airway protection (with a tube): reduces aspiration risk and allows suctioning.
Positive pressure — drawbacks:
- Lung injury risk: too much pressure or volume can cause ventilator-induced lung injury, including barotrauma (pressure-related damage like a pneumothorax).
- Circulation effects: higher chest pressure can lower blood return and blood pressure.
- Comfort/infection: tubes and tight masks can be uncomfortable; invasive ventilation raises infection risk.
Key takeaway: Negative pressure is gentler and more natural, while positive pressure is powerful for emergencies but needs careful settings and monitoring.
Support Your Natural Breathing at Home: Simple Steps to Help Avoid Ventilation
- Gentle movement: simple cardio and easy deep-breathing exercises can help build stamina; ask your doctor which ones are safe for you.
- Clear mucus if that’s an issue: nebulized hypertonic saline (3% or 7%) can thin sticky mucus so it’s easier to cough out, often used in conditions with thick mucus, like cystic fibrosis or bronchiectasis.
- Use a modern nebulizer for meds or saline: a portable mesh nebulizer like the TruNeb™ portable mesh nebulizer turns liquid into a fine mist you inhale while breathing on your own. It’s one option for at-home delivery, and this kind of device can make it easier to fit treatments into your daily routine.
- Daily basics: stay hydrated, avoid smoke and irritants, and follow your care plan to help prevent flare-ups.
Safety note: Talk to your doctor before trying a new medication, including hypertonic saline, and to confirm the right strength and schedule for you. If your breathing symptoms don’t improve, or you feel you’re getting worse, contact your doctor promptly.
⚠️ If you have severe shortness of breath, chest pain, bluish lips or face, or trouble speaking in full sentences, seek emergency care right away (call 911 in the U.S.). Don’t rely on a home nebulizer in a crisis.
Key takeaway: A nebulizer supports your own negative pressure breathing—it doesn’t breathe for you.
Frequently Asked Questions
Tap or click a question below to see the answer:
Negative pressure ventilation uses your chest muscles to create a slight vacuum that pulls air in, while positive pressure ventilation uses a machine to push air into your lungs.
Negative pressure. Your chest expands, pressure drops inside, and air is pulled in.
They are controllable and strong enough for very sick lungs. Clinicians can adjust settings to support oxygen and carbon dioxide while protecting the lungs.
No. A nebulizer delivers medicine or saline as a mist while you breathe on your own. A nebulizer doesn’t create positive or negative pressure — you still breathe in using your own negative pressure breathing.
Yes. Mouth-to-mouth or a bag-valve mask pushes air into the lungs.
Key takeaway: Humans breathe with negative pressure; machines use positive pressure when extra help is needed.
Conclusion: Breathing Easy With the Right Support
Negative pressure is your body’s natural pull. Positive pressure is a controlled push from a device. Knowing both helps you understand daily breathing and what happens when a ventilator steps in.
Simple steps like airway clearance, staying active, and using tools such as nebulizers under your doctor’s guidance help support your natural breathing.
Key takeaway: Normal breathing pulls air into your lungs (negative pressure), while ventilators push air in (positive pressure).
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms, questions, and treatment options.