On this page
What Mold in Your Lungs Really Means
People sometimes say they have 'mold in their lungs' when a musty home and a stubborn cough collide. In medical terms, having 'mold in your lungs' usually means either your airways are reacting to mold like an allergy, or a mold called Aspergillus has started to grow in lung tissue—a condition doctors call aspergillosis.
Mold spores float in the air every day. Most healthy bodies clear them. Your risk goes up if you have asthma, COPD, cystic fibrosis, old lung damage, or a weak immune system. In those cases, spores can trigger swelling, thick mucus, and sometimes a true infection.
There are patterns doctors watch for. Allergic bronchopulmonary aspergillosis (ABPA) flares asthma and can cause thick mucus plugs. Chronic pulmonary aspergillosis can bring a long cough and weight loss. Rarely, invasive aspergillosis spreads fast in people with weak immunity. You might also hear people say 'black mold.' That’s a household nickname, not a diagnosis. Any indoor mold can irritate your lungs.
In short, 'mold in your lungs' almost always means either an allergic reaction to mold or a fungal infection called aspergillosis—not mold growing like it does on walls.
Early Signs vs Serious Symptoms of Mold in the Lungs
Here are common mold in lungs symptoms, from mild allergy-like issues to serious signs of infection. Mild symptoms can include a nagging dry cough, a stuffy or runny nose, throat or eye irritation, and wheezing that feels like an asthma flare. These usually show up soon after you spend time in a damp, musty space and ease when you leave.
Serious lung symptoms build with deeper inflammation or infection. Watch for a cough that brings up phlegm day after day, shortness of breath that limits simple tasks, chest pain, fever or chills, night sweats, fatigue, and unintentional weight loss. ⚠️ Coughing up blood (hemoptysis) is a red flag and needs emergency medical care. In chronic cases, a fungus ball (aspergilloma) can form in an old lung cavity and cause repeated bleeding. In people with weak immunity, invasive aspergillosis can cause high fever, chest pain, and rapid breathing problems.
Mild mold exposure usually feels like allergies, while serious mold infections cause high fevers, chest pain, weight loss, or coughing up blood. These symptom patterns overlap with other illnesses like pneumonia or tuberculosis, so symptoms alone can’t confirm mold—only a doctor can.
Key point: allergy signs tend to improve away from the moldy place; infection signs get worse over days to weeks and can include fever, chest pain, or blood in mucus.

How to Tell If Mold Is Making You Sick
Look at your pattern. If you're wondering how you can tell if you have mold in your lungs, start by noticing when and where symptoms flare. Do your breathing symptoms get worse in a damp or musty space and ease when you spend a day or two away? Do family or coworkers in the same space have similar cough or wheeze? Did your asthma or COPD control slip after a leak, flood, or a move to a humid home? These clues point to mold as a trigger.
See a doctor to sort out what’s going on, and bring details about your home and work, and when your symptoms started, flared, and eased. Doctors connect exposure with symptoms and plan next steps. Two helpful questions to ask: "Do my symptoms fit an allergy or an infection?" and "What tests could confirm or rule out a mold-related illness?"
- Make an appointment with your doctor if a cough or wheeze lasts more than 2–3 weeks, your asthma or COPD suddenly gets harder to control, or your symptoms keep coming back when you return to a moldy place.
- ⚠️ Get emergency care now if you cough up blood, have severe shortness of breath, high fever, or chest pain, or if you have a weak immune system and new breathing trouble.
In short: if symptoms fade away from a moldy space and return when you go back, mold is a likely driver.
Testing for Mold Exposure and Lung Infections
There isn’t an at-home test that proves mold is in your lungs. Here’s how doctors test for mold exposure in your body and lungs.
They start with your story and exam, then can test for mold allergy with a skin prick or blood IgE test. A chest X‑ray or CT scan can show a nodule, a cavity, or a fungus ball. If you bring up sputum, the lab can try to grow fungus from it. In tougher cases, a pulmonologist can do a bronchoscopy or a small biopsy to confirm aspergillosis under a microscope. These steps help separate allergy from infection and guide the right treatment.
Home mold tests can show if there’s mold in your space but can’t tell if it’s in your lungs—only medical tests can do that.
Testing options at a glance
| Test | What it shows | Confirms mold in lungs? | Who orders it |
|---|---|---|---|
| Skin prick or specific IgE blood test | Allergy to Aspergillus or other molds | No, shows allergy only | Allergist or primary care |
| Chest X‑ray or CT scan | Cavities, nodules, or a fungus ball; signs that suggest infection | No, imaging can’t prove fungus | Primary care or pulmonologist |
| Sputum culture or PCR | Aspergillus detected in mucus; supports infection | Sometimes; helps support the diagnosis | Pulmonologist or hospital lab |
| Bronchoscopy or lung biopsy | Tissue sample showing fungus under the microscope | Yes; gold standard to prove infection | Pulmonologist |
| Total IgE, eosinophils (blood) | Allergic inflammation or ABPA clues | No, supports allergic disease | Allergist or primary care |
Key takeaway: Only medical tests—not home kits—can diagnose mold‑related lung disease.
Bottom line: doctors confirm mold‑related illness in your body and lungs with allergy tests, imaging, lab cultures, and sometimes biopsy.
Causes of Mold-Related Lung Problems and Who’s at Risk
Mold thrives where moisture lingers: leaky roofs, wet drywall, basements, bathrooms, and around windows or HVAC. Outdoors, piles of leaves, compost, and barns stir up spores. Breathing a lot of spores indoors can irritate airways and, in some people, cause disease. If you're asking whether mold in a house can cause lung issues, the answer is yes—especially in damp, poorly ventilated spaces.
Your risk goes up if you have asthma, COPD, cystic fibrosis, old lung cavities from infections like tuberculosis, or a weakened immune system from chemotherapy, transplants, or high-dose steroids. Heavy, repeated exposure matters too. Recent research links household mold growth to hypersensitivity pneumonitis (an inflammatory lung disease that causes cough and shortness of breath when your immune system overreacts to inhaled spores). Most healthy people won't get a lung infection from everyday mold, but damp homes can still trigger symptoms.
Damp spaces plus a vulnerable airway or immune system raise the chance of serious mold problems.
Treatment for Mold in the Lungs
Care tackles two things at once: the air you breathe and what’s happening in your lungs. Cleaning up or avoiding the mold source is step one. Medication depends on the diagnosis.
For allergic reactions or ABPA, doctors typically use corticosteroids to calm swelling, sometimes with an antifungal pill to lower the mold load. For chronic pulmonary aspergillosis, long courses of oral antifungals such as itraconazole or voriconazole are used to control infection. If a fungus ball causes repeated bleeding, surgeons sometimes remove the affected part of the lung. Invasive aspergillosis needs hospital care and IV antifungal medicine right away. For mild mold allergies, your doctor might suggest medicines like antihistamines or nasal steroid sprays to control symptoms.
Key point: antibiotics don't treat mold; doctors usually rely on antifungal medicines when they confirm or strongly suspect a fungal lung infection.
Safety note: Talk to your doctor before trying a new medication.
Clearing the Lungs: Supportive Care and Mucus Clearance
Thick mucus can make every breath feel heavy. Keeping airways clear helps you breathe easier while you recover.
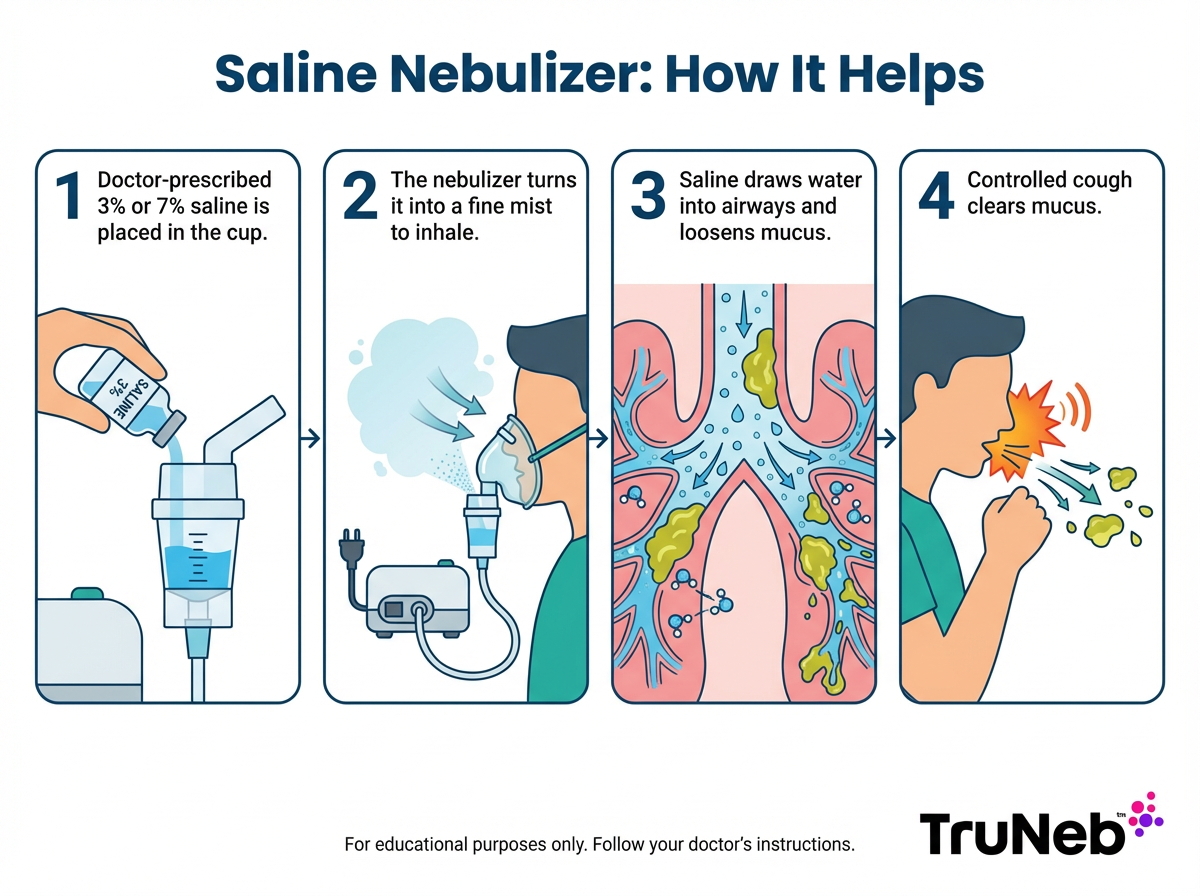
Staying well hydrated thins secretions. Brief warm steam can loosen congestion, but keep your home humidity low the rest of the day so mold doesn't grow. Some people also use a nebulizer to inhale a saline mist. Saline moistens the airways and can help loosen sticky mucus so you can cough it out. A steam inhaler or hot shower only adds warm moisture to your nose and throat. A nebulizer, like TruNeb, actually turns saline into a fine mist you breathe deep into your lungs.
A portable mesh nebulizer like the TruNeb™ portable nebulizer lets you do saline treatments at home or when you're away. With your doctor's guidance, some people use hypertonic saline solutions (such as 3% or 7%) in a nebulizer to pull water into the airways and improve mucus clearance. This doesn't replace antifungal or steroid treatment; it supports comfort and airway hygiene. If you have asthma, ask whether to use your bronchodilator before saline.
In short: nebulized saline can thin sticky mucus so you can cough it up more easily.
Preventing Mold-Related Lung Issues
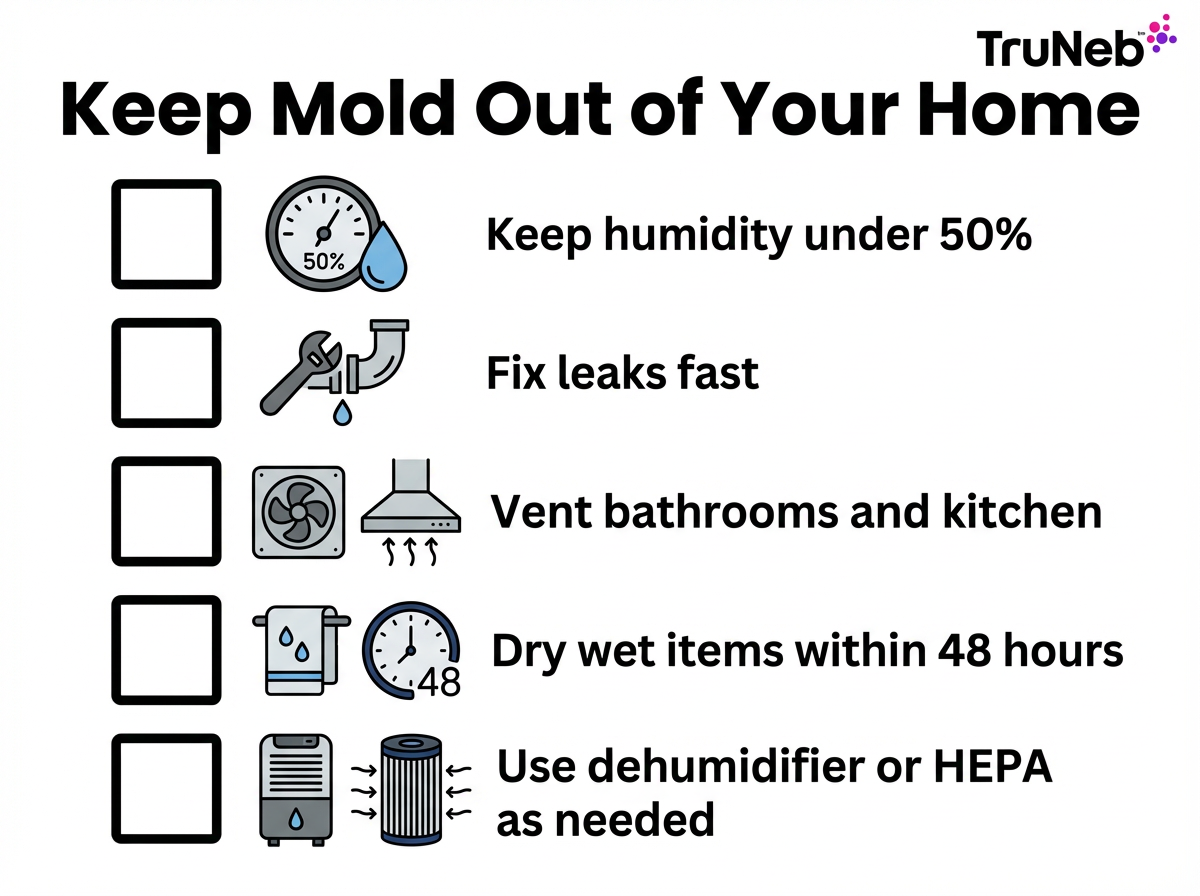
Prevention starts with moisture control and fresh air. If you smell must, act early. If you’re at risk, wear an N95 mask when cleaning moldy areas or doing dusty yard work.
- Keep humidity under 50%; fix leaks quickly; dry wet items within 48 hours; ventilate after showers and cooking; use a dehumidifier or HEPA air purifier in damp rooms.
⚠️ If you live in a space with visible mold and your breathing is getting worse, don't ignore it—talk with your doctor and address the mold problem as soon as possible.
In short: dry, clean, and well-ventilated spaces keep indoor mold in check.
Disclaimer: This article is for informational purposes only and isn't a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms and treatment options.
Frequently Asked Questions
Tap or click a question below to see the answer:
Yes. Breathing air from a moldy space can trigger coughing, wheezing, and other breathing problems. In people at risk, it can lead to lung infections such as aspergillosis.
Aspergillosis is the medical term for lung disease caused by Aspergillus mold. It ranges from allergic forms like ABPA to chronic infection and, rarely, invasive disease.
Common symptoms include a persistent cough, shortness of breath, chest pain, fatigue, and sometimes fever or coughing up blood. Chronic cases can bring weight loss and night sweats, while allergic forms flare asthma and cause mucus plugs.
Sometimes you might see dark flecks from dried blood or debris, but mold itself doesn’t usually create black specks in mucus. There aren’t unique “black mold in lungs symptoms”—so‑called black mold acts like other indoor molds. If you notice black specks or blood, talk with your doctor.
Doctors start with your history and exam, then order tests as needed. Here’s how doctors test for mold exposure in your body and lungs: allergy testing (skin prick or blood IgE), chest imaging (X‑ray or CT), lab studies on sputum, and, if needed, bronchoscopy or a small biopsy to confirm infection.
An X‑ray can show clues like a cavity, nodule, or a fungus ball, but it doesn’t prove mold. Doctors usually pair imaging with lab tests, and sometimes a biopsy, to be sure.
Allergy symptoms can appear within minutes to hours after exposure. Infections tend to develop over days to weeks of illness and usually get worse without treatment.
Yes in some cases. Chronic aspergillosis can scar the lungs over time, and severe infections can damage lung tissue. Brief, mild exposure typically doesn’t cause permanent damage once the mold problem is fixed and symptoms are treated.
Start with your primary care doctor. If symptoms are significant or persistent, your doctor can refer you to a pulmonologist or an allergist for testing and treatment.