On this page

How Often and How Long Should You Use the Incentive Spirometer?
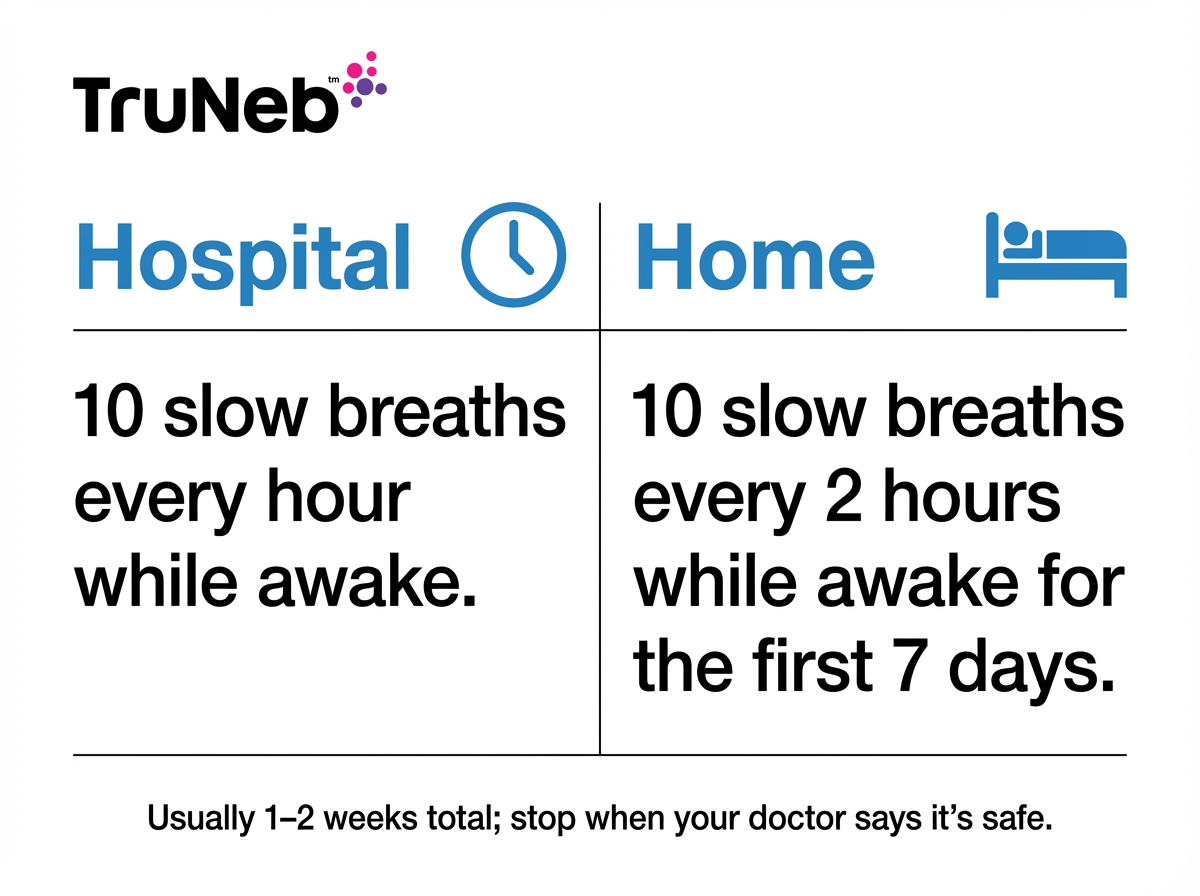
In the hospital, your team usually has you take about 10 slow breaths every hour while you’re awake. Spread those breaths across the hour so your lungs re-expand regularly. At home, a typical plan is about 10 slow breaths every 2 hours while you’re awake for the first week (the first 7 days). You don’t need to wake up at night. Always follow the schedule your doctor or nurse gives you, even if it’s different from this example.
As you heal and move more, you can usually use it less. Most people use it for 1 to 2 weeks after surgery, or until their doctor says it’s okay to stop. Your doctor might let you stop once you’re walking around regularly and can take deep breaths on your own without trouble.
Even after you stop daily spirometer sessions, keep taking a few deep breaths and gentle coughs during the day while you’re still healing.
Key point: Short sets done regularly with an incentive spirometer keep your lungs open better than one long session.
Simple rule: A common plan is 10 slow breaths every hour while you’re awake in the hospital, then about 10 every 2 hours while you’re awake at home for the first week, unless your doctor gives different instructions.
Understanding Your Readings and Setting Goals
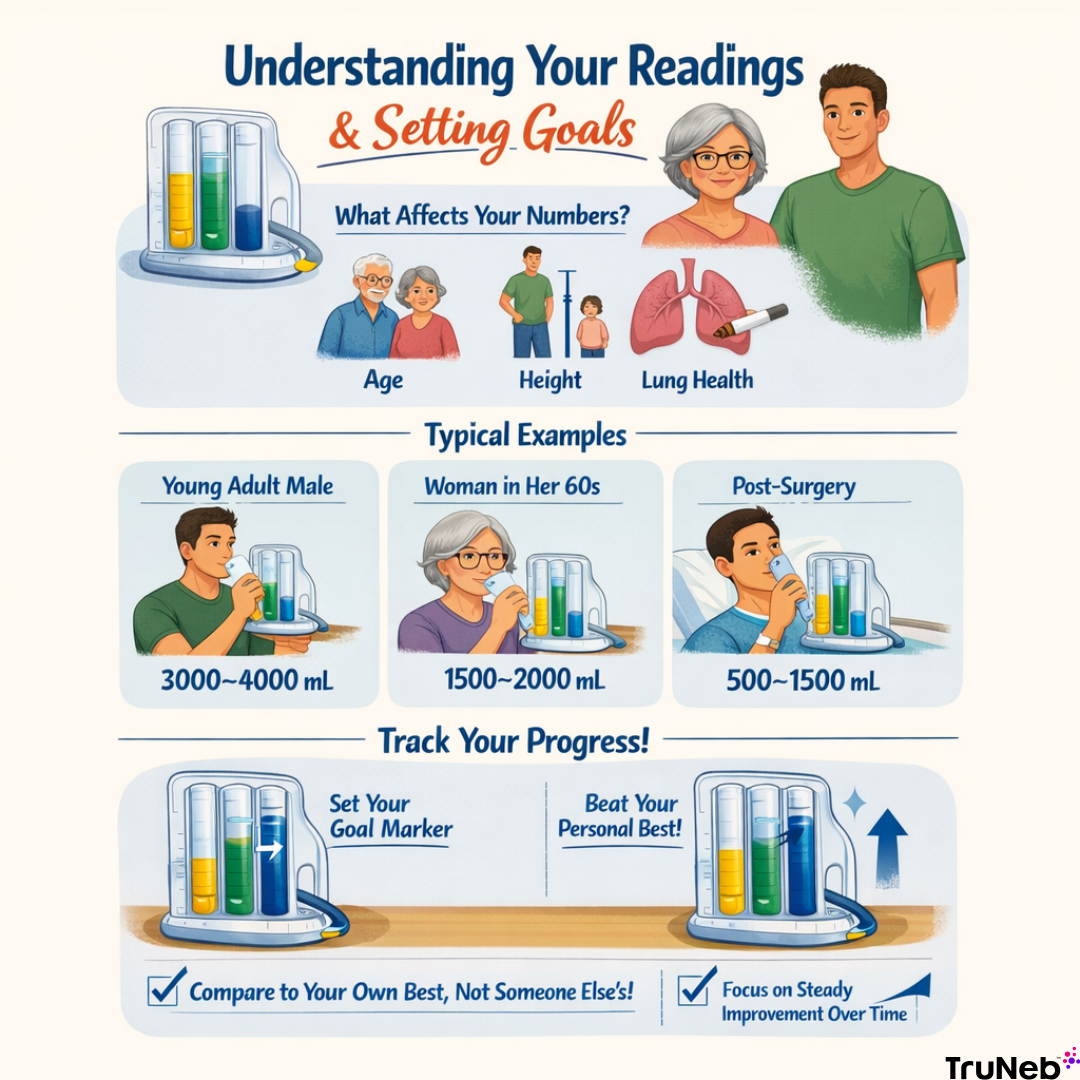
A “good” number depends on you. The spirometer shows volume in milliliters or liters. Your doctor sets a goal marker based on your age, height, sex, and health. Taller people and those with larger lungs generally have higher numbers, while age, smoking, or lung disease can lower them. Start where you are and raise the goal as you get stronger.
Here are ballpark examples: a healthy young adult male typically draws about 3000–4000 mL; a healthy woman in her 60s is usually closer to 1500–2000 mL; right after surgery, it’s common to start around 500–1500 mL. These are examples, not targets.
Use the device’s pointer to mark your personal best. If you beat it, slide it up. If you fall short one day, that’s okay. Focus on steady progress.
An incentive spirometer is a training tool, not a full lung test, so a low number on it doesn’t mean you have a lung disease. If you’re worried about long-term lung function, ask your doctor about formal pulmonary function testing.
Key point: Judge success by your personal best and how it improves over time—not by someone else’s number.
Takeaway: Track your personal best incentive spirometer reading and raise the goal as breathing gets easier.
Tips, Troubleshooting, and Common Mistakes
If it hurts to take a deep breath
Deep breaths can feel rough after surgery—that’s normal. If your doctor prescribed pain medicine, take it the way they told you to, then use the spirometer when it starts working. Hug a pillow over your incision (splinting) during deep breaths and coughs. Start with smaller breaths and build up. If you feel sharp chest pain that doesn’t feel like incision pain, pause and tell your care team.
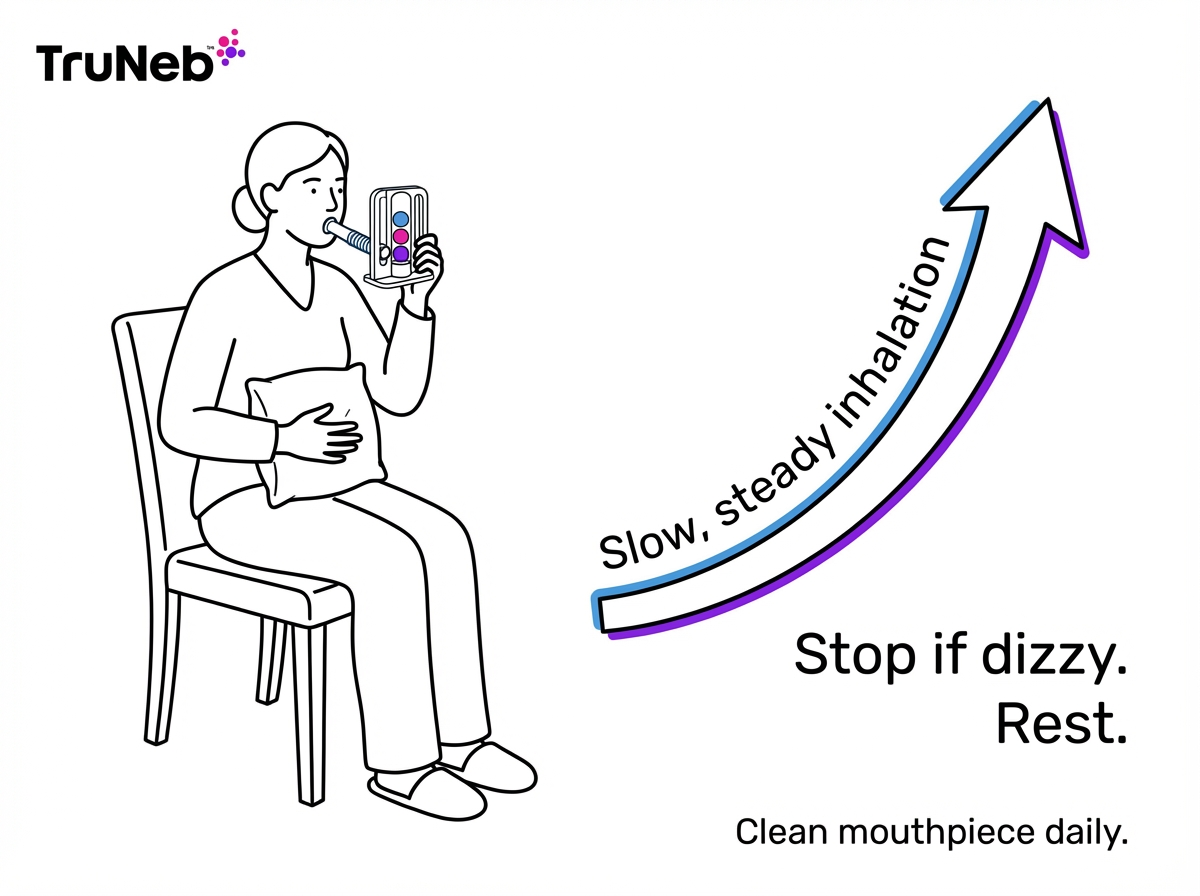
If you feel dizzy or lightheaded
Stop, remove the mouthpiece, and breathe normally for a minute. Dizziness usually happens when you breathe too fast. Go slower and rest between breaths. If dizziness keeps coming back even when you slow down, let your doctor or nurse know.
If you can’t reach your goal marker
Don’t get discouraged. Relax your shoulders and breathe with your belly to draw a steadier inhale. Your numbers usually rise over days as your lungs recover.
If you’re coughing a lot
Some coughing is good—it clears mucus. Take slightly smaller, slower breaths if big breaths trigger a cough fit. Keep tissues nearby and splint with a pillow if coughing hurts. Call your doctor if you cough up blood or thick, unusual mucus.
Common Mistakes to Avoid
- Don’t blow into the spirometer. You inhale through it.
- Don’t rush. A fast sip won’t fill your lungs well.
- Don’t skip sessions. Set gentle reminders.
- Don’t forget to reset the piston between breaths.
- Don’t skip cleaning. Wash the mouthpiece in warm, soapy water daily, rinse, and air-dry.
Check your spirometer’s instructions and follow any specific cleaning directions from the manufacturer.
Quick guide: When you use your incentive spirometer, go slow, rest if you feel dizzy, and splint with a pillow to make deep breaths easier.
⚠️ If you have sudden or worsening chest pain, severe shortness of breath, confusion, blue lips or face, or cough up a lot of blood, call 911 or your local emergency number right away. Call your doctor if you develop a fever, your cough or mucus gets worse, or you feel more short of breath over time.
Beyond the Spirometer: Other Tools to Keep Your Lungs Clear
Your spirometer is the main tool to keep your lungs open. If you have a lot of mucus or a lung condition, your care team sometimes adds other therapies.
Nebulizers turn liquid medicine or saline into a mist you breathe in. This can add moisture, loosen mucus, and help open airways.
A portable mesh nebulizer like the TruNeb™ portable mesh nebulizer is quiet and easy to carry, so you can do treatments at home without a big setup. Doctors sometimes prescribe nebulized saline or bronchodilators to help clear secretions.
Hospitals also use airway clearance tools, like a PEP device (a small valve you breathe out through to help keep airways open) or a flutter device, and hands-on chest physiotherapy to loosen mucus. These are added when you need extra help clearing your lungs.
Safety note: Talk to your doctor before trying a new medication, including any nebulizer treatment or saline solution.
Key takeaway: These breathing devices do different jobs—an incentive spirometer trains slow, deep inhalation; a nebulizer delivers medication or saline mist; a peak flow meter measures how fast you blow air out; and steam inhalers aren’t for prescription meds.
| Device | What it does | Delivers medication? | When it’s used |
|---|---|---|---|
| Incentive spirometer | Trains slow, deep breaths and helps re-expand lungs | No | After surgery or illness to help prevent atelectasis and clear mucus |
| Nebulizer (mesh or jet) | Turns liquid medicine or saline into an inhaled mist | Yes, when prescribed | To deliver bronchodilators or saline when your doctor recommends it |
| Peak flow meter | Measures how fast you exhale | No | To monitor airway narrowing (for example, in asthma) |
| Steam inhaler | Provides warm, humid air | No* | Comfort measure; not for prescription treatments |
*Steam inhalers are not nebulizers and shouldn’t be used for prescription breathing medications.
For most people after surgery, using the incentive spirometer and coughing regularly is enough. Extra tools are added only if your doctor thinks you need them.
Frequently Asked Questions
Tap or click a question below to see the answer:
There isn’t one number that fits everyone. Healthy adults typically pull in roughly 2000 to 4000 mL, but age, sex, height, and health change that range. After surgery, your numbers are usually lower at first. Focus on the goal your doctor set and steady progress, not a generic average.
Most hospital teams use a plan like 10 breaths an hour while you’re awake, then about 10 every 2 hours at home for about a week. See the section “How Often and How Long Should You Use the Incentive Spirometer?” above, and always follow your doctor’s exact instructions.
Most people continue for 1 to 2 weeks or until their doctor says it’s okay to stop. Your doctor might let you stop once you’re walking around regularly and can take deep breaths during normal activities without trouble.
Yes. If it’s your home device, wash the mouthpiece (and any detachable parts) in warm soapy water once a day, rinse well, and air-dry completely. Don’t share your spirometer with others.
No. An incentive spirometer trains slow, deep inhalation. A peak flow meter measures how fast you blow air out. A nebulizer delivers a medicated or saline mist into your lungs. You might also see steam inhalers on shelves. These are not nebulizers and aren’t meant for breathing prescription medications.
Plain takeaway: Use your incentive spirometer regularly, focus on your own progress, and ask your doctor if you’re ever unsure about how or how often to use it.
Disclaimer: This article is for informational purposes only and isn’t a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your health, your incentive spirometer plan, and any medications or devices you use.