On this page

Emergency vs. Home-Care Wheezing Checklist
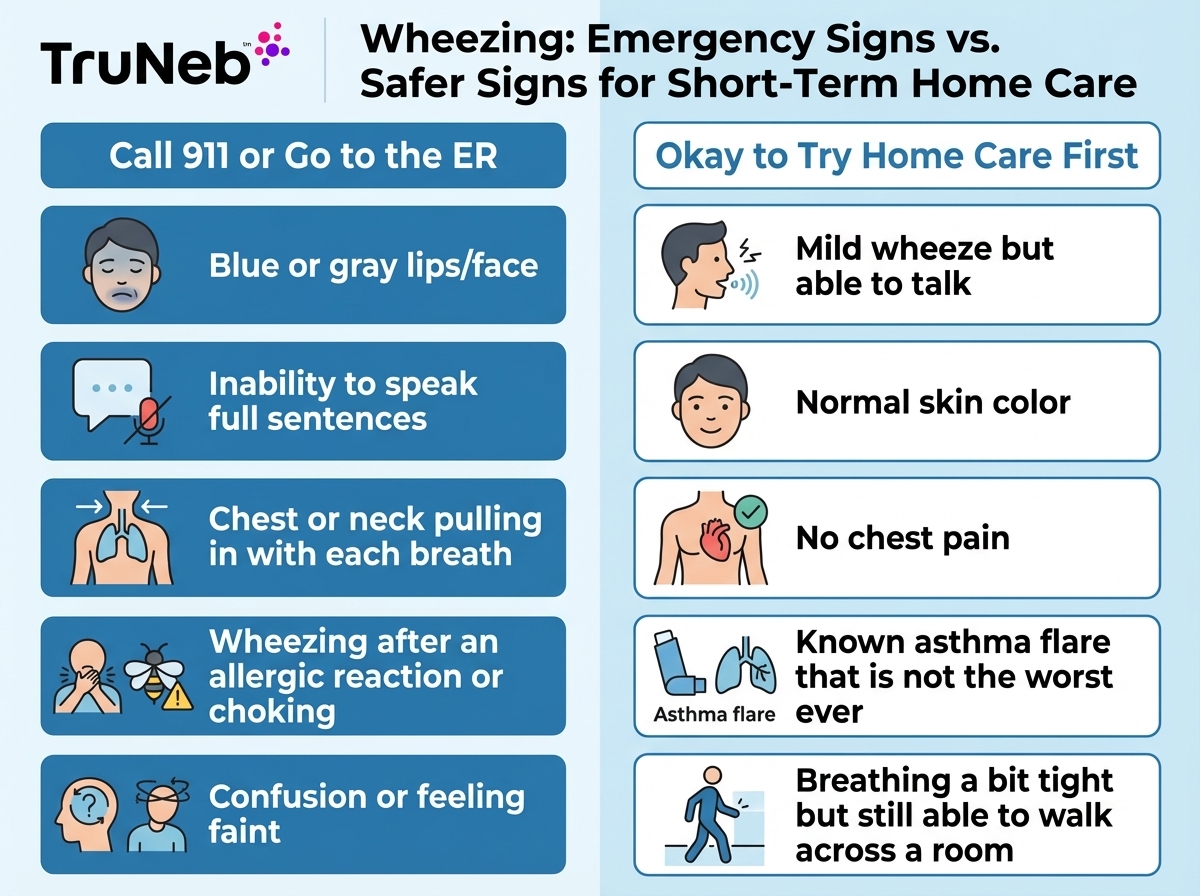
Use this quick checklist to decide how to stop wheezing immediately at home and when it is actually an emergency.
🚨 Signs You Need Emergency Care
Call 911 or your local emergency number or go to the ER right away if:
- You are so short of breath you can't speak in full sentences.
- Lips, face, or fingernails look blue or gray.
- Wheezing starts right after a bee sting, new medicine, or food (possible severe allergic reaction).
- You hear a harsh, high-pitched noise when breathing in, or it sounds like choking (see the 'Wheezing or Stridor?' section below).
- The chest or neck pulls in with each breath, or you feel confused, dizzy, or like you may pass out.
- You have chest pain or tightness along with wheezing.
⚠️ Call 911 or your local emergency number right away if you have any of the emergency signs above.
✔️ When It’s Safer to Try Home Care First
You can try home steps first if your wheezing is mild to moderate, your color looks normal, you can still talk in full sentences, and this feels like a usual flare from asthma or allergies rather than the worst episode you have ever had.
If it feels safe to stay home, sit upright, loosen tight clothing, and focus on slow, steady breaths. Use your rescue inhaler if your doctor has prescribed one, move away from smoke or strong fumes, and add warm, moist air with a steamy bathroom or humidifier. Watch your symptoms closely. If breathing gets worse or any red-flag sign appears, treat it as an emergency.
Key point: Mild wheezing with easy breathing is usually manageable at home for a short time, but any sign of low oxygen or severe trouble breathing means you need emergency care.
If You Have an Inhaler or Nebulizer: Using Rescue Medications First
If you have a rescue inhaler or nebulizer that your doctor prescribed, use it as your first step for fast wheezing relief. Using your prescribed rescue inhaler or nebulizer is usually the fastest way to ease wheezing.
Use your rescue inhaler the way your doctor and your asthma action plan describe. That usually means taking one or two puffs and giving it a few minutes to work. If you have a spacer, use it with your inhaler to get more medicine into your lungs.
If your usual rescue inhaler dose does not ease your breathing or your symptoms are severe, treat that as an emergency rather than taking extra doses on your own.
If you also have a nebulizer with medicine like albuterol solution, set it up the way you were shown in the clinic, using the medication your doctor prescribed, and breathe in the mist until the treatment is finished. A nebulizer can be helpful when your chest feels too tight to use an inhaler well, because it delivers medicine as a gentle mist over several minutes.
An inhaler with a spacer works well for most people, while a nebulizer delivers medicine as a mist over several minutes and can be easier when your chest feels too tight to use an inhaler well.
This table compares key differences between rescue inhalers and nebulizers so you can understand how each fits into the wheeze-relief plan you and your doctor create.
| Feature | Rescue inhaler | Nebulizer |
|---|---|---|
| How medicine is given | Short bursts of medicine you breathe in with a fast, deep breath | Continuous mist you breathe in slowly over several minutes |
| Portability | Very small and easy to carry in a pocket or bag | Machine or portable device that is larger than an inhaler |
| When it is most helpful | Quick relief for people who can take a strong, deep breath | During bad flares, for young children, or when your chest feels too tight to use an inhaler well |
| Setup and cleaning | Needs a spacer for best use and occasional cleaning of the mouthpiece | Needs regular cleaning of the cup, mask or mouthpiece, and sometimes tubing |
| Who decides what to use | Your doctor decides whether an inhaler, nebulizer, or both belong in your treatment plan. | |
A portable mesh nebulizer like the TruNeb™ portable nebulizer makes it easier to take a breathing treatment at home or on the go without a bulky compressor.
For people with chronic lung conditions and thick mucus, such as cystic fibrosis or bronchiectasis, some clinicians also prescribe hypertonic saline solutions, such as TruNeb 3% sterile hypertonic saline solution or TruNeb 7% sterile hypertonic saline solution, to help loosen mucus during nebulizer treatments. Hypertonic saline is usually prescribed for specific chronic lung diseases and is not a do-it-yourself remedy.
Always talk to your doctor before starting new medications or changing how you use your inhaler or nebulizer. Using your prescribed rescue inhaler or nebulizer, exactly as your doctor instructed, is usually the fastest way to ease a wheezing flare.
No Inhaler? Quick Home Remedies to Relieve Wheezing
If you don't have a rescue inhaler nearby, you can still use simple home steps to help calm mild wheezing.
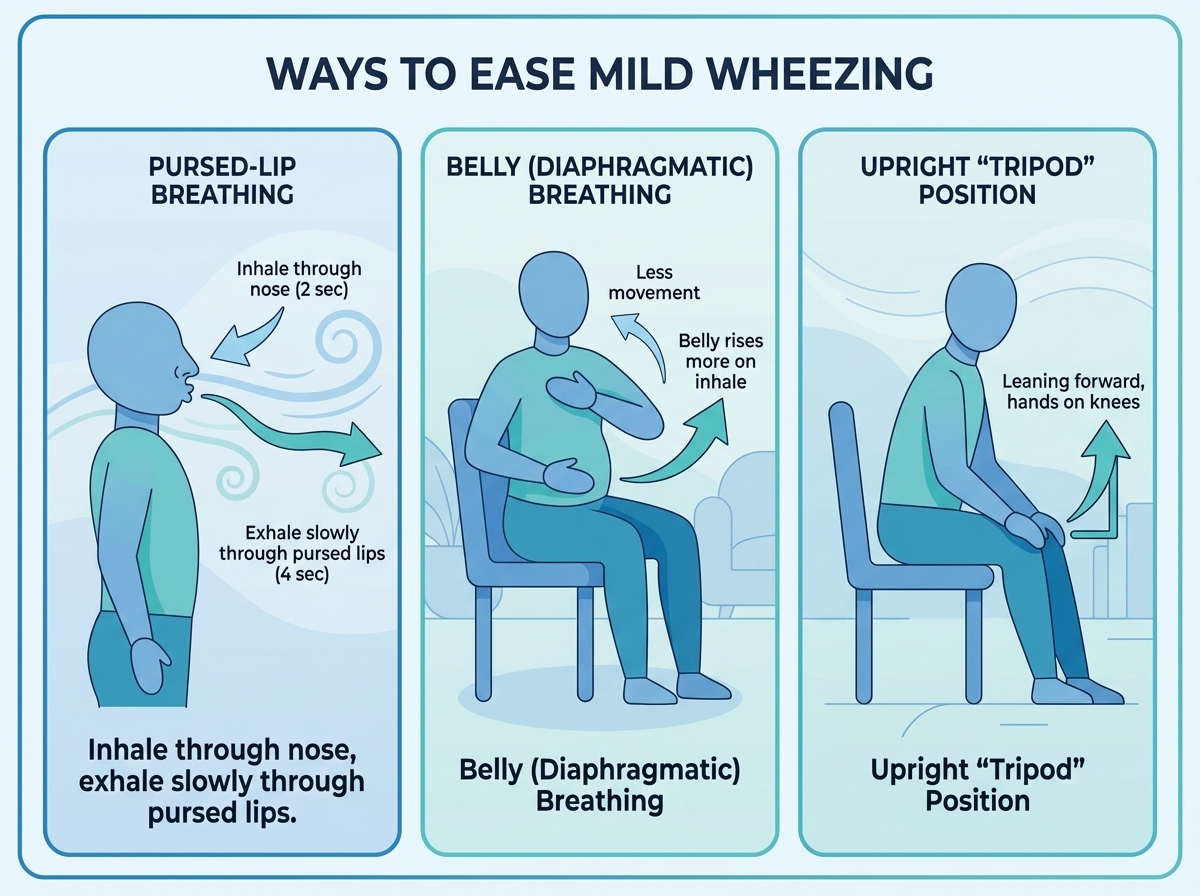
Start with your breathing. Try pursed-lip breathing: breathe in slowly through your nose for about two seconds, then breathe out gently through lips that are lightly pressed together, as if you are whistling. Make your exhale about twice as long as your inhale. This gentle back pressure can help keep small airways open longer so more air can move out.
Then try belly breathing. Place one hand on your chest and one on your stomach. Breathe in through your nose so your stomach rises more than your chest, then breathe out slowly through your mouth. This uses your diaphragm and can ease the tight feeling in your chest while also helping you stay calm.
Shift your position to make breathing easier. Stop what you are doing and sit upright in a chair or on the edge of the bed. Let your shoulders relax and lean forward slightly with your hands on your knees or on a table. This "tripod" position lets your diaphragm move more freely so each breath takes less effort.
Add warm, moist air. Go into a steamy bathroom, or sit over a bowl of hot water with a towel over your head and breathe in the warm mist for a few minutes. A warm shower does the same. Moist air can loosen mucus and soothe irritated airways.
Sipping warm water, herbal tea, or even a small cup of coffee can also help some people. The warmth relaxes the airway lining, and for some people the caffeine in coffee acts like a mild airway opener.
A nebulizer is for breathing medications. Steam inhalers, facial steamers, and humidifiers are for moist air only, and they are not safe ways to take prescription meds. ⚠️ Don't put prescription medicines into a humidifier, facial steamer, or bowl of hot water, because those devices are not designed to deliver medications the way a nebulizer does.
Clear obvious triggers around you. Move away from smoke, dust, strong perfume, cleaning sprays, or very cold air. Open a window for fresh air if pollen is not a big trigger for you, or switch on an air purifier if you have one.
These steps usually start to ease mild wheezing within a few minutes if it feels safe to stay home. Only use these home steps if your breathing is uncomfortable but still manageable. If you're struggling to breathe, treat it as an emergency.
Slow, controlled breathing plus warm, moist air can ease mild wheezing when you don't have medicine, but you still need emergency care if breathing becomes hard or you develop any red-flag signs from the checklist.
⚠️ If breathing becomes hard, you feel like you can't get air in, or any red-flag sign appears, stop home steps and get emergency care right away.
How to Stop Wheezing at Night
Nighttime wheezing can feel scary and make it hard to sleep. A few simple changes can help your breathing settle down so you can rest.
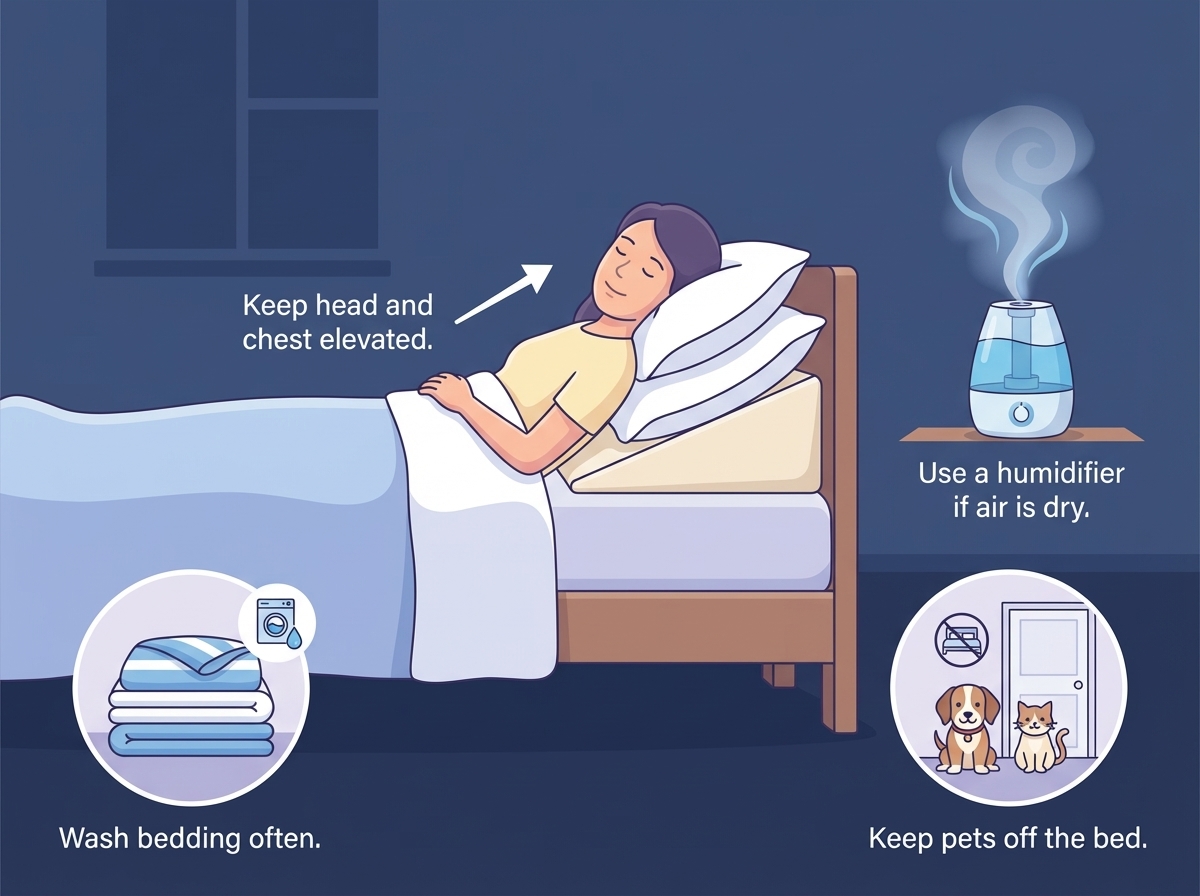
First, change how you lie down. Don't lie flat if you are wheezing. Prop your upper body up with extra pillows or a wedge so your head and chest are higher than your stomach. You can also sit on the edge of the bed with your feet on the floor until your breathing eases. This uses gravity to take pressure off your lungs and help mucus drain instead of sitting in your airways.
Keep your bedroom air friendly to your lungs. A lot of people breathe better at night with a cool-mist humidifier running, which keeps the air from getting too dry. Wash bedding often in hot water and use dust-mite covers on your pillows and mattress if dust seems to trigger you. Keep pets off the bed and out of the bedroom if pet dander makes you wheeze.
Think about what you do in the hour or two before bed. Large meals or lying down right after eating can cause acid reflux. Acid reflux can irritate your airways when you lie down and trigger night wheezing. Try to finish eating at least a couple of hours before you lie down, and avoid foods that usually cause heartburn for you. If your doctor has given you a controller inhaler or nightly medicine, take it exactly as prescribed and tell them if you still wake up wheezing.
If nighttime wheezing wakes you up again and again, or it does not settle after you sit up, use your prescribed medicine, and try these steps, your doctor needs to know so you can adjust your long-term plan.
Changing your sleep position, bedroom air, and evening habits can sharply cut down on nighttime wheezing and help you rest.
Wheezing or Stridor? Telling Noisy Breathing Apart
Not all noisy breathing is the same. Knowing the difference between wheezing and stridor helps you judge how urgent the situation is.
Wheezing is a high-pitched, musical whistling sound that usually happens when you breathe out. It comes from the smaller airways inside the lungs being narrowed, like what happens in asthma, bronchitis, or COPD. The noise tends to spread across both sides of the chest.
Stridor is a harsher, louder sound that is usually heard when a person breathes in. It comes from a blockage or severe narrowing higher up, in the throat or windpipe. Croup in children, choking on food, or swelling from a severe allergic reaction can all cause stridor. Stridor almost always needs urgent medical attention.
A simple rule of thumb: a whistling sound mainly on the out-breath points to wheezing in the lungs, while a harsh, squeaky noise on the in-breath can mean stridor in the upper airway and is an emergency.
If you're not sure which sound you hear but breathing looks or feels very hard, treat it as urgent and seek medical help right away instead of trying home care alone.
After the Wheezing Stops: Next Steps and Prevention
Once your breathing has eased and the wheeze is gone or much softer, take time to plan what comes next.
Keep an eye on how you feel for the rest of the day and night. Wheezing can return if your trigger is still around or if rescue medicine wears off. Keep your inhaler or nebulizer close for several hours after a flare, and avoid smoke, strong fumes, and cold air while you recover.
Think about what likely set this episode off. Was it exercise, a cold, dust, pollen, stress, or lying flat after a big meal? Write down when it started, what you were doing, and what helped. A simple wheeze diary on your phone or a notepad can help you and your doctor spot patterns over time.
If this was your first wheezing episode, if attacks are happening more, or if you don't have a clear asthma or lung diagnosis, make an appointment with your doctor. They might do breathing tests, talk about triggers, and set up an asthma action plan or other treatment plan. Some people need a daily controller inhaler or regular nebulizer treatments to keep symptoms under control. If you have asthma, ask your doctor to help you create or update an asthma action plan so you know exactly what to do for future flares.
Breathing exercises like pursed-lip and belly breathing can also become part of your daily routine, not just an emergency tool. Over time, this type of practice can make your lungs more efficient and help you stay calmer during flares.
Key point: Stopping one wheezing spell is important, but the real protection comes from a clear plan you build with your doctor to prevent and treat future episodes safely.
Talk to your doctor before trying a new medication or changing how often you use your inhaler or nebulizer. This article is for general education and not a personal medical plan.
Frequently Asked Questions
Tap or click a question below to see the answer:
To stop wheezing immediately without an inhaler, sit upright, stay calm, and focus on slow pursed-lip breathing so you can push air out of narrowed airways. You can also try belly breathing, warm steam from a shower or steamy bathroom, and moving away from smoke, dust, or strong smells. Use the pursed-lip breathing steps in the section above as your guide. If your breathing gets worse or any emergency sign from the checklist appears, seek emergency care right away instead of staying at home.
The fastest way to relieve wheezing for most people is to use a rescue bronchodilator inhaler, such as albuterol, exactly as prescribed by your doctor. While you wait for it to work, sit upright, stay as relaxed as you can, and use pursed-lip breathing. If your usual inhaler or nebulizer dose does not improve your breathing within a few minutes, or you feel very short of breath, treat that as an emergency and get urgent medical care instead of taking extra doses on your own.
If wheezing starts when you lie down, raise your head and chest with extra pillows or a wedge instead of lying flat. Keeping a cool-mist humidifier in the bedroom and washing bedding regularly can cut down on dry air and dust that irritate your lungs. Try not to eat big meals right before bed, especially if you get heartburn, because acid reflux can trigger nighttime wheezing when you lie down. If this keeps happening night after night, talk with your doctor about nighttime asthma or reflux and whether your long-term treatment needs an adjustment.
Wheezing does not always mean you have asthma. It is a sign that air is having trouble moving through narrowed airways, and asthma is only one common cause. Infections like bronchitis, allergies, COPD, and heart or reflux problems can also lead to wheezing. If you wheeze a lot or don't know the cause, see your doctor so they can test your lungs and help you find the right diagnosis.
A nebulizer is not automatically better than an inhaler for wheezing. Both can give fast relief when they use the right medicine for you. An inhaler with a spacer works well for most people and is quick and portable, while a nebulizer delivers medicine as a mist over several minutes and can be easier during a bad flare or for young children. A small mesh nebulizer such as the TruNeb portable nebulizer is one home option some doctors recommend when a nebulizer fits your treatment plan. Your doctor is the best person to tell you whether an inhaler, nebulizer, or both are right for you.
Always talk to your doctor before trying a new medication, changing how you use your inhaler or nebulizer, or starting treatments like hypertonic saline. These answers are for general education and are not a personal medical plan.