On this page

Hemoptysis vs Hematemesis: Key Differences and Definitions
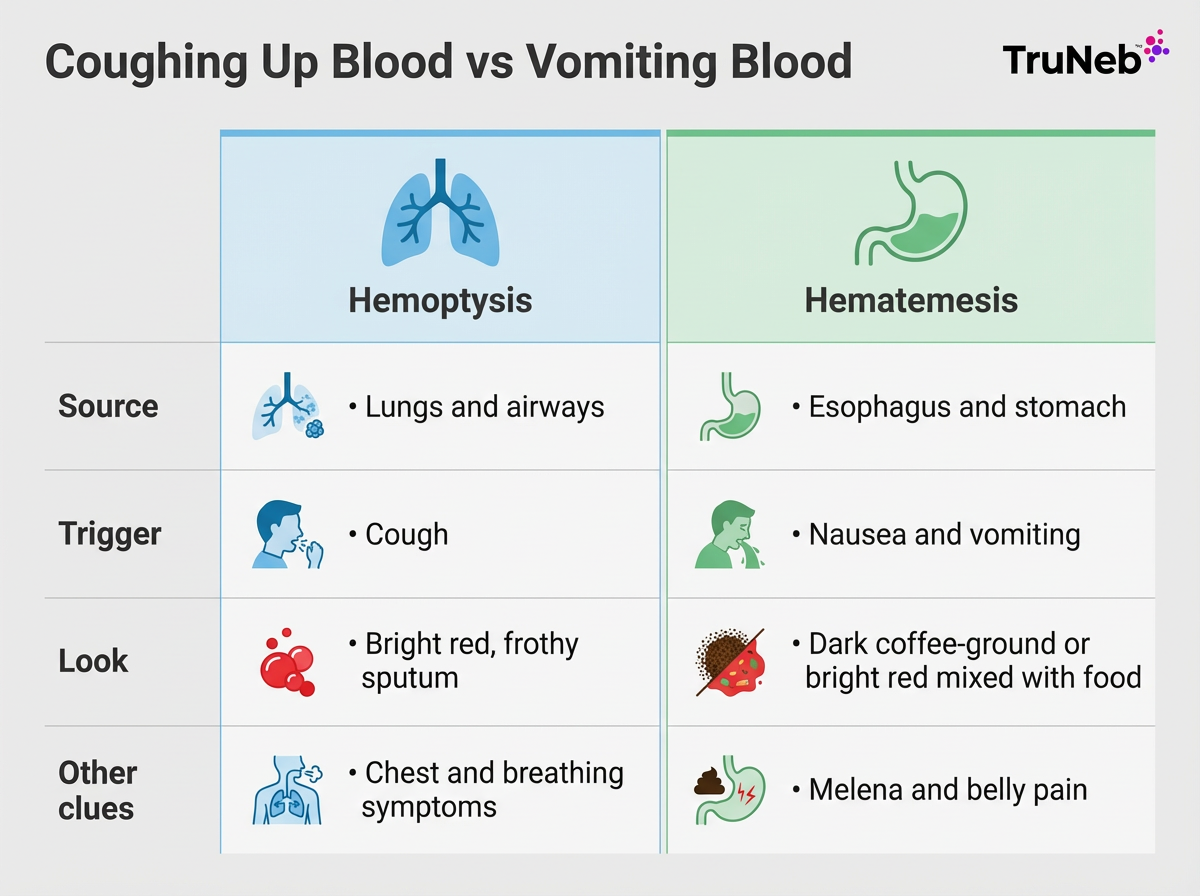
Hemoptysis means you cough up blood from your lungs or airways. Hematemesis means you vomit blood from your esophagus or stomach. They’re not the same.
In plain terms, the difference between hemoptysis and hematemesis is that hemoptysis is coughing up blood from the lungs, while hematemesis is vomiting blood from the stomach or esophagus.
With hemoptysis, blood shows up during a cough, usually in mucus (sputum) from your lungs. It’s usually bright red and can look bubbly or frothy because it mixes with air and mucus. With hematemesis, you feel sick to your stomach first, then vomit blood that can be dark and grainy like coffee grounds or bright red mixed with food and stomach contents.
Other clues can help: bleeding from the lungs can come with chest pain, shortness of breath, or infection symptoms. GI bleeding can bring upper belly pain or black, tarry stools called melena. If you’re trying to sort out coughing up blood vs vomiting blood, focus on whether it happens with a cough or with nausea and vomiting.
Quick comparison: hemoptysis vs hematemesis
| Feature | Hemoptysis (lungs) | Hematemesis (GI) |
|---|---|---|
| Source | Lungs and airways | Esophagus or stomach |
| Trigger | Cough | Nausea and vomiting |
| Appearance | Bright red, frothy or bubbly | Dark coffee‑ground or bright red |
| Mixed with | Mucus (sputum) | Food and stomach contents |
| Other clues | Chest symptoms, breathing issues, infection signs | Upper belly pain, known liver disease |
| Stool change | Usually none | Black, tarry stools (melena) |
Key takeaway: Cough plus frothy red blood in mucus points to the lungs; nausea or retching with coffee‑ground or bright red blood mixed with food points to the GI tract.
Hemoptysis is coughing up frothy, bright red blood from your lungs, while hematemesis is vomiting blood from your esophagus or stomach, usually as dark coffee‑ground material or bright red fluid mixed with food.
Hemoptysis: Causes and Symptoms of Coughing Up Blood
Hemoptysis happens during a cough. The blood is usually bright red and can look bubbly or frothy because it mixes with air and mucus. It can be just a few streaks in phlegm or, sometimes, larger amounts.
Common causes include bronchitis and pneumonia. These usually come with fever, a wet cough, and feeling run down. Tuberculosis can cause a long-lasting cough with weight loss and night sweats. Chronic lung problems like COPD, bronchiectasis, and cystic fibrosis can lead to daily mucus and repeated infections that sometimes bleed.
More serious causes include lung cancer, especially in older people who smoke, and pulmonary embolism, which can cause sudden chest pain, shortness of breath, and blood in sputum. Heart failure can cause pink, frothy sputum. Blood thinners can make any bleed worse.
Fever, weight loss, or night sweats with hemoptysis are red flags that need prompt evaluation. Large or fast bleeding is rare but dangerous because it can block breathing. Doctors call very large amounts of coughing blood massive hemoptysis, which is a medical emergency. Any persistent or unexplained hemoptysis should be checked by a doctor.
Takeaway: In short, hemoptysis means blood that comes up with a cough in your mucus, and it can range from small streaks with bronchitis to heavier bleeding from serious lung or heart problems.
Hematemesis: Causes and Symptoms of Vomiting Blood
Hematemesis is vomiting blood. You usually feel nauseated or retch first. The vomit can look like coffee grounds when blood has mixed with stomach acid. If the bleeding is brisk, it can be bright red instead.
Peptic ulcers are a common cause. They can bleed slowly, leading to coffee‑ground vomit, or suddenly, causing bright red blood. Gastritis (stomach lining irritation) or severe esophagitis (irritation of the esophagus) can cause smaller bleeds and burning upper belly pain. A Mallory–Weiss tear can follow repeated retching and cause streaks of blood. Severe acid reflux can inflame your esophagus (esophagitis) enough to cause small amounts of blood in vomit.
Esophageal varices from liver disease can rupture and cause a large, life‑threatening bleed without much warning. Some cancers of the stomach or esophagus can also bleed. Black, tarry stools called melena can show up when blood travels through the intestines.
Any vomiting of blood is abnormal and can turn serious quickly. Seek emergency care right away by calling 911 or going to the nearest emergency room.
Takeaway: Hematemesis means you’re actually vomiting blood from your upper digestive tract, and the vomit often looks like dark coffee grounds or bright red blood mixed with stomach contents.
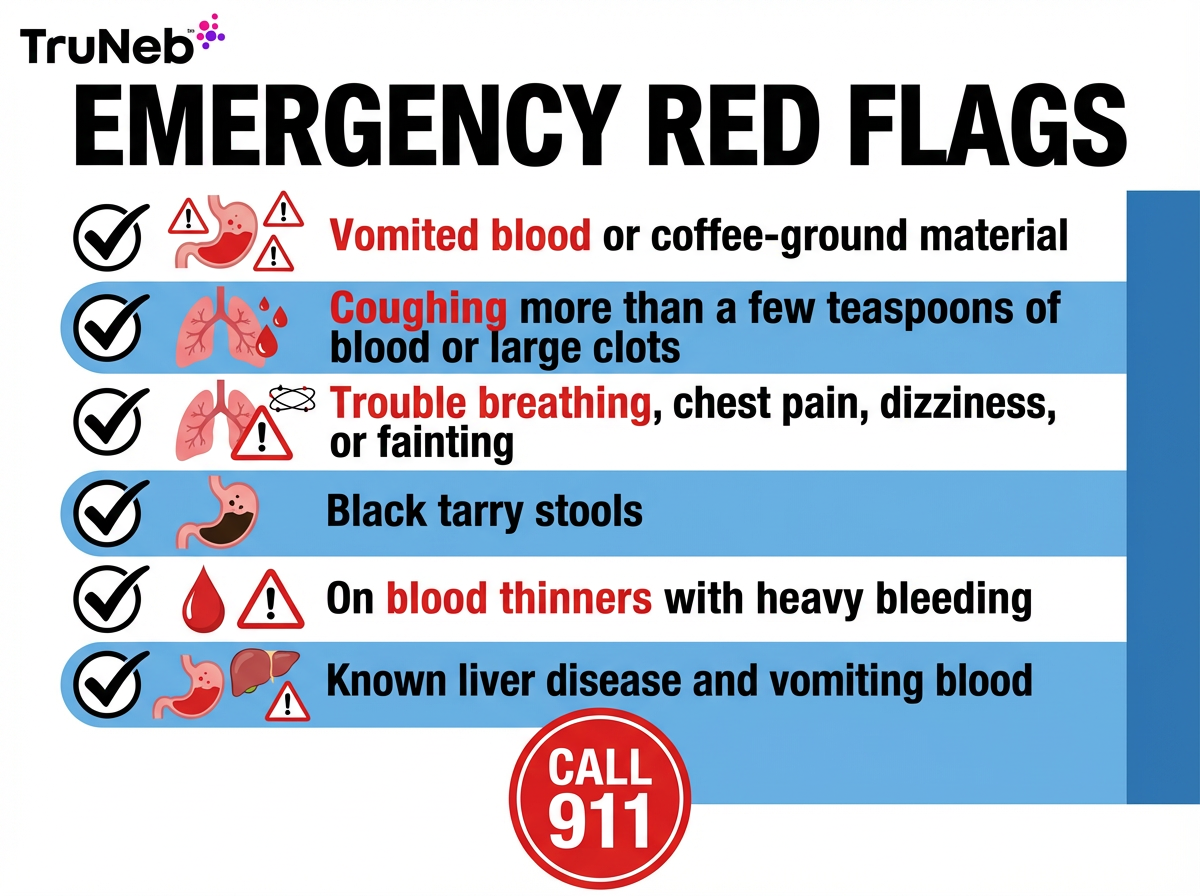
When to Seek Emergency Care
Blood from any source needs medical attention; some situations are emergencies.
⚠️ Call 911 or your local emergency number right away if any of the situations below apply to you.
- Vomited blood of any amount, or dark coffee‑ground material.
- Coughing up more than a few teaspoons, large clots, or bleeding that’s speeding up.
- Trouble breathing, chest pain, dizziness, fainting, or signs of shock.
- Black, tarry stools or known liver disease with vomiting blood.
- Heavy bleeding while on blood thinners, or a recent high‑risk diagnosis like lung cancer or active TB with new bleeding.
Vomiting blood is always an emergency, and coughing up large or rapidly increasing amounts of blood is an emergency too.
If you only see a small streak of blood once but it happens again or you’re worried, contact your doctor or urgent care the same day.
These are general warning signs, not strict cutoffs. If you’re unsure whether your bleeding is serious, it’s safer to get checked right away.
If bleeding starts, try not to eat or drink unless emergency staff tell you to, and stay sitting up or on your side while you wait for help.
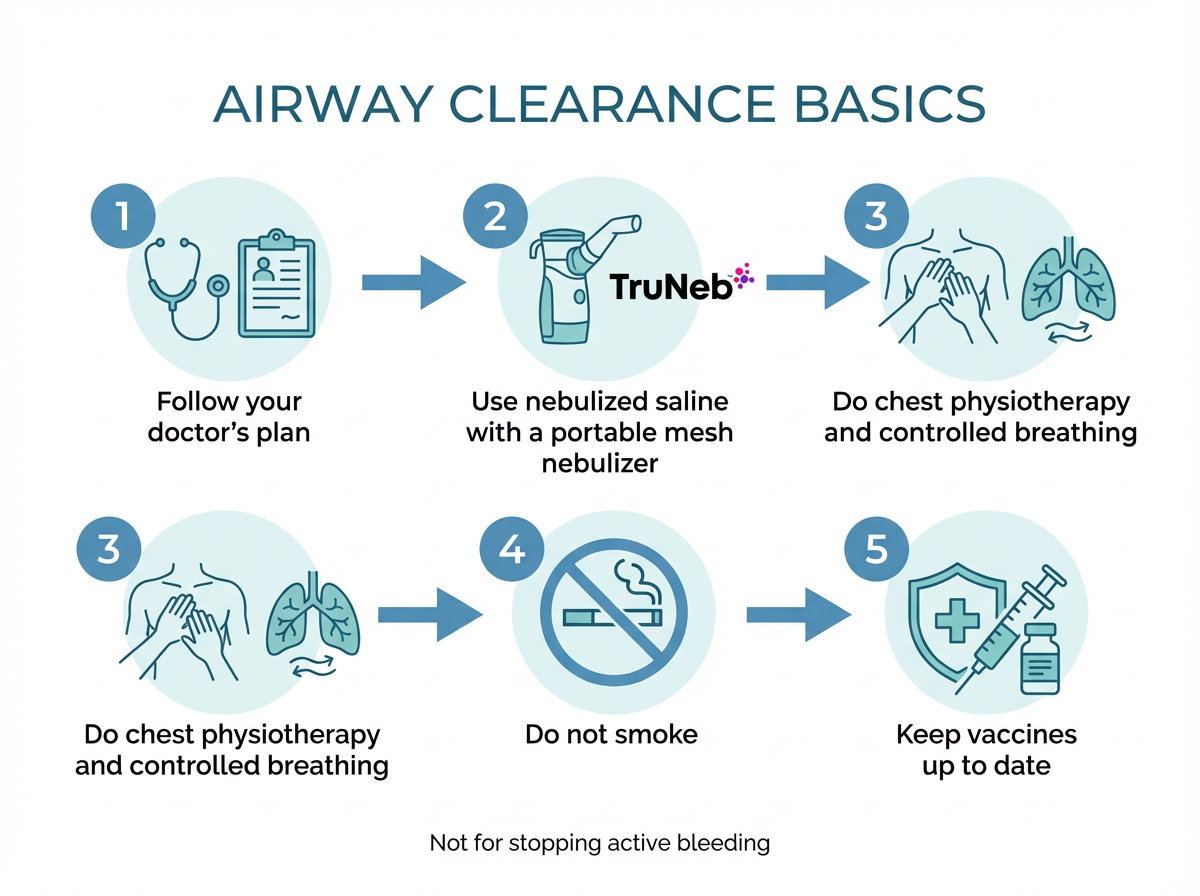
Managing Chronic Lung Conditions to Reduce Hemoptysis
After urgent issues are handled, work with your doctor on a plan to prevent future bleeding. If you live with bronchiectasis, COPD, or cystic fibrosis, airway clearance helps keep mucus moving and lowers infection risk. Not smoking and keeping your flu and pneumonia vaccines up to date can also cut your risk of lung infections that trigger bleeding.
Clinics commonly use hypertonic saline (a salty nebulized solution) to thin mucus so it’s easier to clear. A portable mesh nebulizer like TruNeb™ can make these treatments easier to do at home or on the go as part of a doctor‑guided plan. This can help support better lung hygiene over time as part of your overall treatment plan. Steam inhalers are not the same as nebulizers and aren’t used to deliver prescription medicines into your lungs.
This isn’t a fix for active bleeding and shouldn’t be used to treat a sudden episode of coughing up a lot of blood — use the emergency steps above instead.
Talk to your doctor before trying a new medication or inhaled therapy.
Takeaway: Managing the lung disease that causes your bleeding and sticking with daily airway clearance, including doctor‑guided nebulized saline treatments, can lower your chances of coughing up blood again.
Frequently Asked Questions
These FAQs answer common questions about blood in spit, swallowed nosebleeds, which type of bleeding is more dangerous, and how doctors figure out where the blood started. Tap or click a question below to see the answer:
Vomiting blood is usually more urgent and should be treated as an emergency. Coughing small streaks is usually from irritation, but large or fast hemoptysis is also dangerous and needs immediate care.
They match your symptoms and the look of the blood, then use tests. A bronchoscopy can check the airways, and an endoscopy can check the esophagus and stomach. They might also check blood tests and imaging like a chest X‑ray or CT scan to help locate the bleed and see how much blood you’ve lost.
If you’re seeing blood when you spit but you’re not actually coughing from your chest, it usually isn’t true hemoptysis. It can come from the mouth, throat, or a nosebleed that drained back. Doctors sometimes call bleeding from the nose or throat that looks like hemoptysis “pseudohemoptysis.” If it keeps happening, see a doctor to find the source.
Yes. Swallowed blood can irritate your stomach and get vomited back up, and nosebleed blood can drain into your throat and be coughed out. That can mimic a lung or GI bleed even when the source is the nose. Tell your doctor if you had a recent nosebleed.
It means blood has mixed with stomach acid and darkened, which points to an upper GI bleed. It’s still serious and needs medical care.
⚠️ Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about any symptoms, concerns, or treatment decisions.