On this page

Introduction: What Exercise-Induced Asthma (EIB) Means
Exercise-induced bronchoconstriction (EIB), often called exercise-induced asthma or sports-induced asthma, is when your airways narrow during or after physical activity. You might notice coughing, wheezing, chest tightness, or shortness of breath a few minutes into a hard workout or soon after you stop. It's common and very manageable.
EIB can happen if you have asthma and even if you don't. With the right plan, you can keep moving and do the sports you love. This guide covers exercise-induced asthma treatment and prevention so you can stay active.
Signs and Symptoms of Exercise-Induced Asthma
Know the pattern: EIB symptoms show up with exercise and take time to fade.
- Cough during or after exercise (sometimes the only sign), wheeze, chest tightness, or shortness of breath
- Symptoms typically peak 5–10 minutes after you stop and ease after 20–30 minutes of rest
Feeling winded from being out of shape usually improves quickly once you stop. EIB tends to hang on longer and can require a rescue inhaler.
Why Exercise Triggers Asthma Symptoms
During hard exercise you usually breathe faster through your mouth. Cool, dry air rushes in and dries the lining of your airways. That can make the muscles around your airways tighten and narrow.
Certain settings make this more likely. Cold weather, dry indoor air, high pollen or pollution, and strong fumes like chlorine can all raise your risk. Skipping a warm-up can also trigger symptoms. If your day-to-day asthma or allergies aren't well controlled, exercise symptoms are more likely. Symptoms are more common in endurance or cold‑weather sports.
In simple terms, fast breathing of cool, dry air during hard exercise dries and irritates your airways, which makes them tighten.
How Doctors Diagnose Exercise-Induced Asthma
Your doctor will ask about your symptoms and can run breathing tests. A common test is spirometry to measure how much and how fast you can blow air out. Your doctor might then have you exercise and repeat the test. A clear drop after exercise supports the diagnosis. Some clinics use special challenge tests when needed.
Other problems can look like EIB, such as vocal cord dysfunction or heart issues in older adults. That's why an exam helps. If you respond well to an asthma medicine after exercise, that also points to EIB. Your doctor can also create an asthma action plan that explains how to handle exercise and flare-ups.
Doctors usually confirm exercise-induced asthma by checking your breathing before and after exercise and ruling out other causes of shortness of breath.
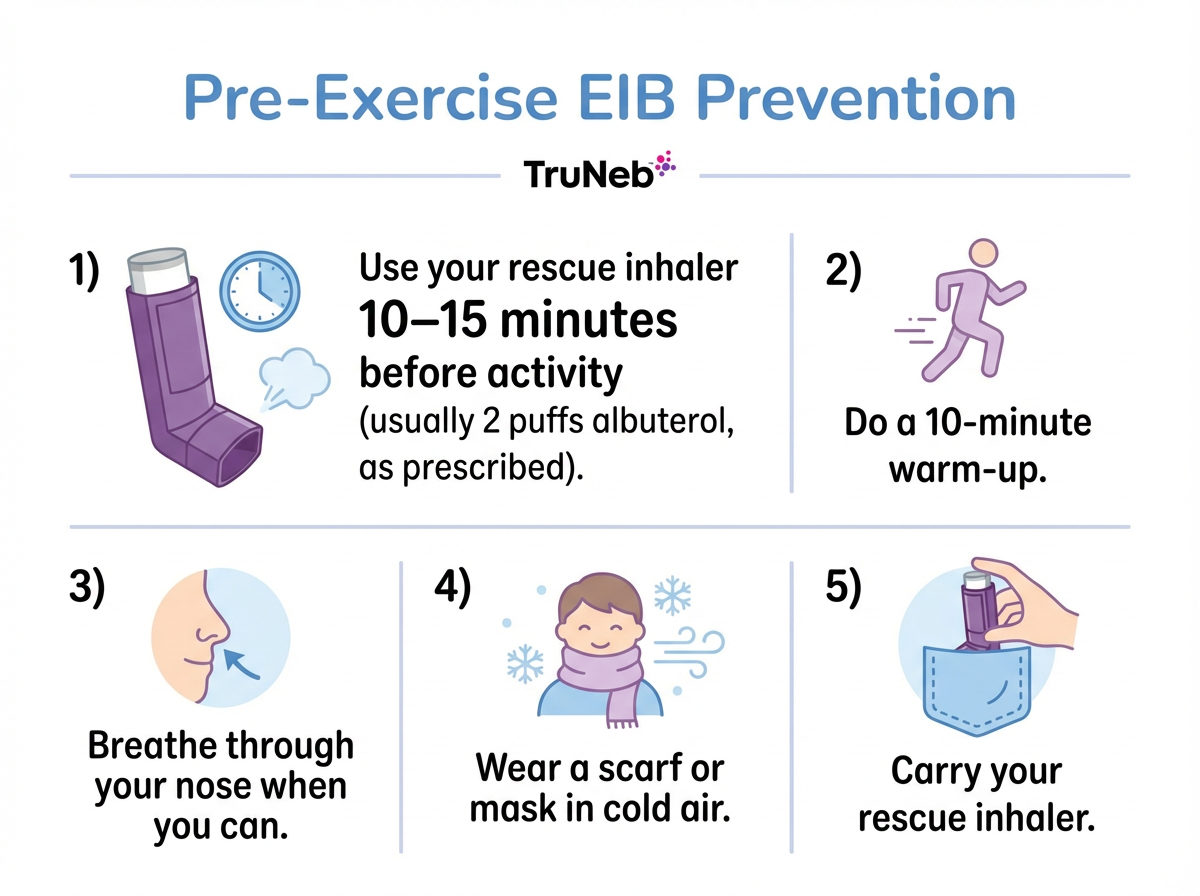
Quick-Relief Treatment Before You Work Out
Fast relief before workouts starts with a rescue inhaler. A short-acting beta agonist such as albuterol opens the airway muscles. Doctors commonly prescribe using a rescue inhaler shortly before exercise, such as taking two puffs about 10 to 15 minutes before you start. For many people, this can help protect against symptoms for a couple of hours, but your exact plan should follow your doctor's instructions. Some people use levalbuterol if they feel jittery with albuterol. Use a spacer if you have one to help the medicine reach your lungs.
Key point: Using a quick-relief inhaler shortly before activity is one of the fastest, most reliable steps doctors use to help prevent exercise symptoms.
Don't overuse your rescue inhaler. If you need it frequently or it wears off fast, your plan needs an update with your doctor.
Safety note: Talk to your doctor before trying a new medication.
Daily Controller Treatment for Frequent Symptoms
If you still have frequent symptoms, a daily controller can calm your airways. Inhaled corticosteroids reduce inflammation and make the lungs less reactive. They work over time, not instantly.
Some people use a combination inhaler that pairs a steroid with a long-acting bronchodilator. Combinations with formoterol can also be used before exercise when prescribed. Long-acting bronchodilators shouldn't be used without a steroid for asthma. If you reach for your rescue inhaler most days, ask your doctor about adding a controller.
Montelukast and Other Add-On Medications
Montelukast is a leukotriene blocker taken as a pill. It can help reduce exercise symptoms for some people, especially if allergies also play a role. It can be taken daily or, in some cases, a few hours before activity as directed. It isn't a rescue medicine.
Pros include ease of use and help with allergy-related swelling. Cons include that it doesn't work for everyone and, rarely, it can affect mood, behavior, or sleep. If you or your child notice mood changes, behavior changes, or trouble sleeping, contact your doctor right away. Older options like cromolyn may be used before exercise in select cases. Treating your allergies can also help.
Montelukast is an add-on pill, not a rescue medicine, and it's only helpful for exercise symptoms in some people.
Non-Drug Strategies to Prevent Exercise-Induced Asthma
Medicine is only part of the plan. Smart habits make exercise easier. A steady warm-up, breathing through your nose when you can, picking kinder conditions, and a cool-down all help. These steps work best alongside your prescribed treatment.
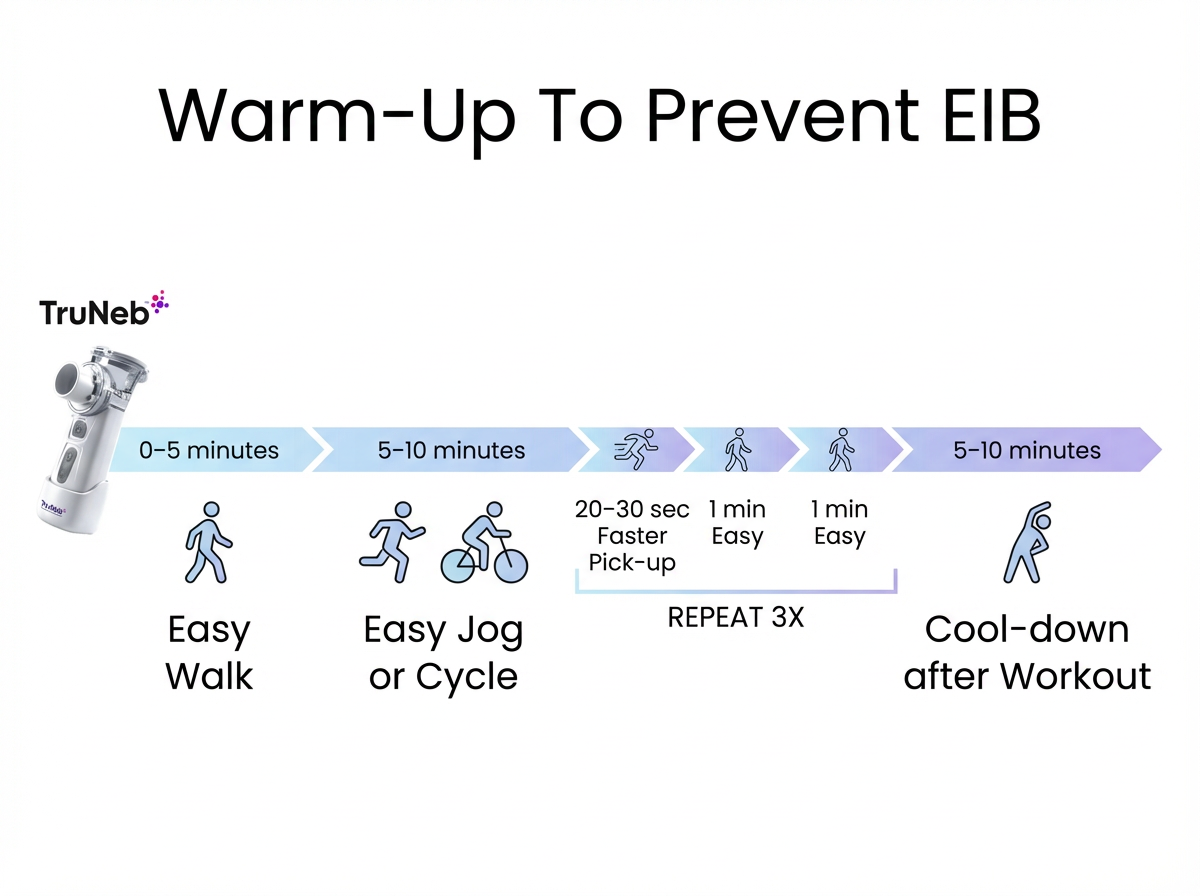
Warm-Up Routine That Helps Prevent Symptoms
A good warm-up prepares your lungs like it prepares your legs. Start with 5 to 10 minutes of easy movement such as brisk walking or light cycling. Then add a few short pick-ups of faster effort with rests in between. This can create a refractory period, so your airways are less reactive for the next hour or two. After your workout, ease down with a slow jog or walk and gentle stretches.
Breathe Smart While You Move
Try to breathe through your nose during moderate parts of your workout. Your nose warms and moistens the air before it reaches your lungs. In cold weather, wear a scarf or a heat-exchange mask over your mouth and nose. If you feel short of breath, slow down and try nose-in, slow lips-out breathing to regain control. Staying calm helps your breathing settle faster.
Choose Better Conditions and Pace Your Workouts
When air is very cold, very dry, or full of pollen or pollution, move your workout indoors if you can. Choose milder days for outdoor runs. A lot of people find stop-and-go sports like volleyball or baseball easier than long, continuous efforts like distance running. You don't have to avoid a sport you love, but plan ahead and use your pre-exercise steps.
What About Natural Remedies for Exercise-Induced Asthma
There is no herbal cure for EIB. The most effective natural steps are the ones you control every day: warm up, breathe through your nose, cover your mouth in cold air, and cool down. Build fitness gradually and stay hydrated. Use supplements only with your doctor's advice and don't replace proven treatment.
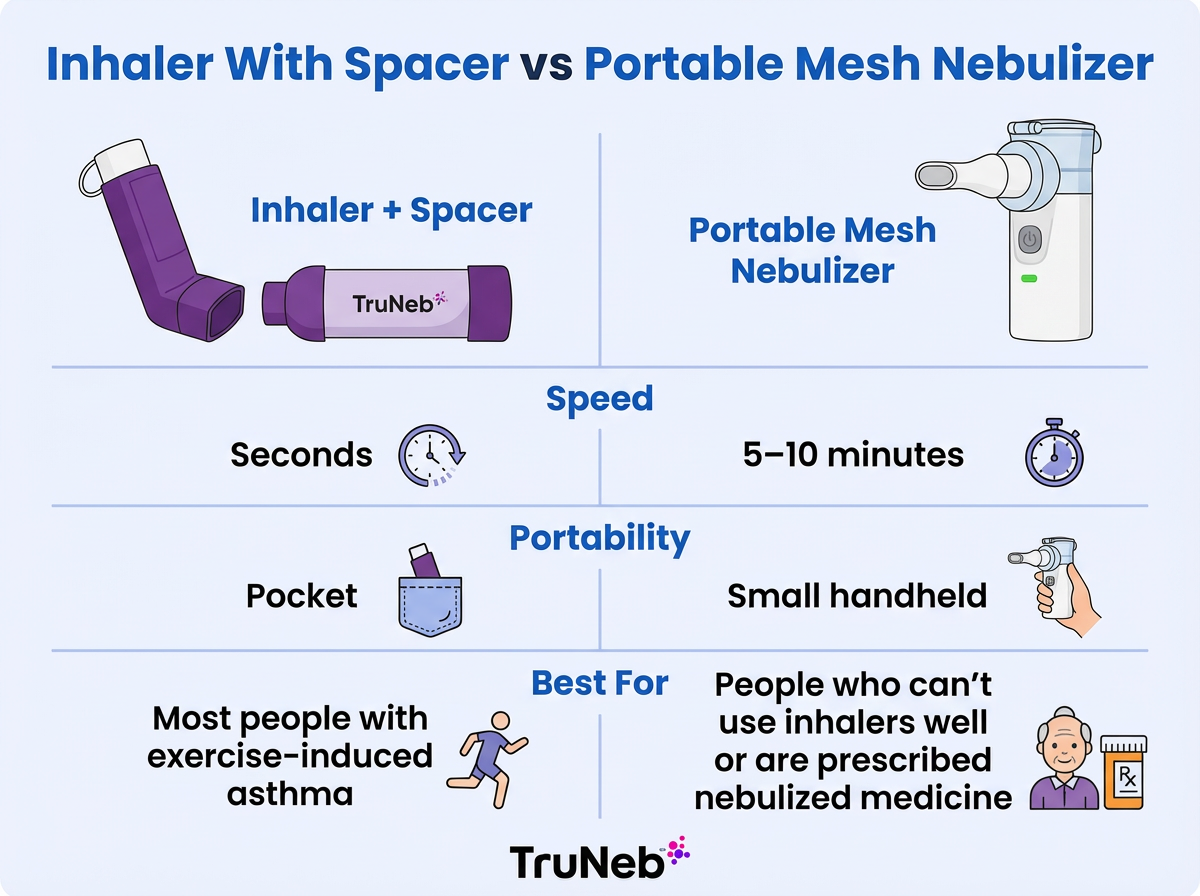
Inhalers, Spacers, and Nebulizers
How you take medicine matters. A metered-dose inhaler used with a spacer helps more medication reach your lungs. It's quick to use before a workout.
Nebulizers turn liquid medicine into a mist you breathe for several minutes. They're helpful for people who can't use inhalers well or who are prescribed nebulized medicines. For routine exercise prevention, inhalers are usually faster and easier.
Most people manage exercise-induced asthma best with an inhaler plus spacer; a portable mesh nebulizer is reserved for those who truly need nebulized medicine as prescribed by a doctor.
| Feature | Inhaler + spacer | Portable mesh nebulizer |
|---|---|---|
| Setup & speed | Ready in seconds | Runs for 5–10 minutes per treatment |
| Portability | Pocket-size | Small handheld device |
| Use before exercise | Common first choice for most people | Use only if your doctor prescribes nebulized meds |
| Medication delivery | Metered-dose or dry-powder inhalers | Nebulized bronchodilators or saline, as prescribed |
| Best for | Most people with EIB | Those who can't use inhalers well or need nebulized medicine |
| Cleaning | Spacer rinsed periodically | Parts cleaned and air-dried after use |
Note: Steam inhalers are for warm mist only and should not be used to deliver asthma medications.
Only use nebulized medications and solutions that your doctor has prescribed for you. A device like the TruNeb portable mesh nebulizer is small and travel-friendly and can deliver bronchodilator or saline treatments your doctor prescribes. It doesn't replace your asthma action plan or regular inhalers. Use the device your doctor recommends and make sure your technique is checked.
Key point: For most people with exercise-induced asthma, an inhaler with a spacer is the go-to option. Nebulizers are for special situations your doctor recommends.
Plan for During and After Exercise
If symptoms start during exercise, slow down or stop. Use your quick-relief inhaler as directed in your asthma action plan or by your doctor. Wait until your breathing feels normal before you continue, and keep it light. Don't push through a flare. Let a coach or workout partner know about your plan so they can help if needed.
Some people have a late return of symptoms hours later, so watch how you feel and tell your doctor if this keeps happening. When symptoms start, follow your asthma action plan or your doctor's instructions.
If your breathing doesn't return to normal after using your rescue inhaler and resting, stop exercising and follow your asthma action plan or seek medical care.
When to Seek Medical Help for Exercise-Induced Asthma
⚠️ Call 911 or seek emergency care right away if any of these happen:
- Severe shortness of breath that doesn't improve after your rescue inhaler
- Trouble speaking in full sentences
- Lips or fingernails turning blue
- Skin pulling in between ribs or at the neck when you breathe
- Breathing that's getting worse quickly
- Chest pain
Err on the side of caution. Quick care can save a life.
You Can Stay Active With Exercise-Induced Asthma
With the right treatment and habits, you can be as active as your friends. Plenty of athletes have asthma and manage it well. Regular training, done safely, can make your breathing stronger over time. Track what works for you and share it at your visits. Keep your inhaler with you and celebrate the small wins.
FAQs: Exercise-Induced Asthma Treatment and Prevention
Tap or click a question below to see the answer:
Exercise-induced bronchoconstriction is airway narrowing triggered by exercise. It can occur in people with chronic asthma and in some people without chronic asthma. A lot of people with asthma do get exercise symptoms, but EIB is specific to exertion.
Being out of shape feels like heavy breathing that quickly improves with rest. EIB brings cough, wheeze, or chest tightness that typically peaks after you stop and can take 20–30 minutes to fade. A rescue inhaler usually helps EIB.
Albuterol is the standard quick-relief choice. It opens airways within minutes. Some people use levalbuterol. Proper technique matters as much as brand.
A common plan is to use your rescue inhaler shortly (about 10–15 minutes) before activity, usually 1–2 puffs. This can protect you for 2–4 hours, but always follow your doctor's instructions for your exact dose and timing. See the Quick-Relief section above.
See your doctor if you suspect EIB or if symptoms break through your plan. Go to the ER or call 911 if breathing is severe, you can't speak in full sentences, your lips turn blue, or your rescue inhaler doesn't bring quick relief.
Most people do best with an inhaler and a spacer because it's fast and portable. A nebulizer helps if you can't use inhalers well or if you're prescribed nebulized medicine. Portable mesh nebulizers like TruNeb can be useful in those cases.
Warm-ups, nose breathing, covering your mouth in cold air, and smart pacing help the most. Supplements haven't proven to replace your inhaler. Use any add-ons only with your doctor's guidance.
There is no cure, but with good control most people have few or no symptoms. Kids and teens sometimes see improvement as they grow. Keep your plan in place and be prepared.
Disclaimer: This article is for informational purposes only and isn't a substitute for professional medical advice, diagnosis, or treatment. Always talk to your doctor about your symptoms and before starting, stopping, or changing any medication or exercise plan.