On this page

Dry vs Wet Cough: The Basics
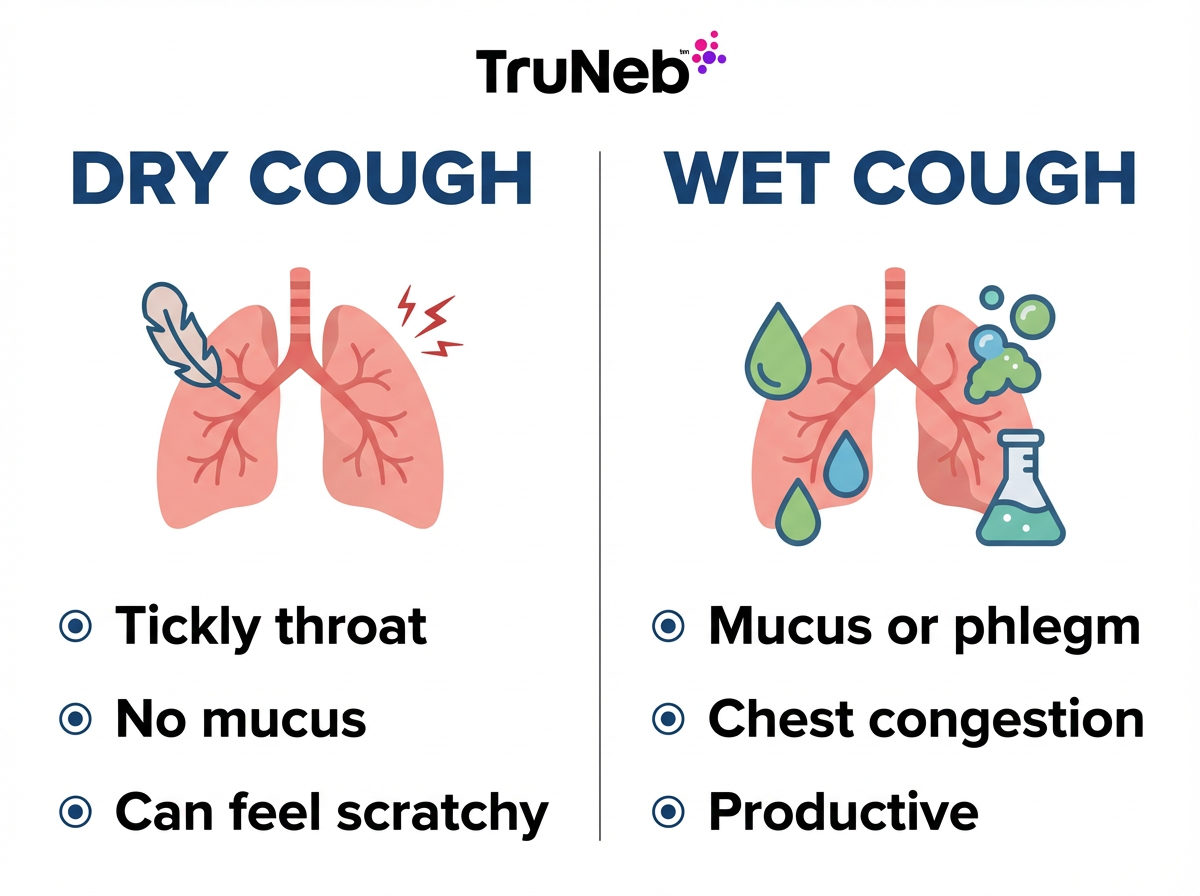
A dry (non-productive) cough doesn’t bring up mucus; a wet (productive, chesty) cough does. That simple clue helps you choose care that fits what your body needs. Both cough types protect your airways by reacting to irritation or clearing out mucus.
At-a-glance: Dry cough doesn’t bring up mucus; wet cough does. Soothe a dry cough, clear a wet cough, and see a doctor for red flags.
| What to compare | Dry cough (non-productive) | Wet cough (productive) |
|---|---|---|
| Mucus | No mucus comes up | Mucus/phlegm comes up |
| Feel/sound | Tickle or itch in throat, hacking | Chesty rattle or gurgly |
| Common triggers | Irritants/allergies, early cold or flu, asthma, GERD | Later cold/flu, bronchitis, pneumonia, COPD, post-nasal drip |
| Home focus | Soothe throat: fluids, honey, humidifier, rest | Thin and clear mucus: hydration, steam, expectorant |
| Medicine approach | Suppressants are used for dry, irritating coughs—ask a doctor or pharmacist | Expectorants are used to keep the cough productive—ask a doctor or pharmacist |
| See a doctor if | Cough lasts weeks, you have trouble breathing, high fever, chest pain, or blood in mucus | |
Key takeaway: A dry cough doesn’t bring up mucus, while a wet cough does.
What Causes a Dry Cough?
Most dry coughs come from irritation, not gunk.
- Irritants and allergies: smoke, dust, pollution, or pollen can tickle your airways and spark a dry hack.
- Viral infections: at the start of a cold or flu, coughs usually start out dry before mucus builds. A dry after-cough can also linger for days or weeks while airways heal. Early COVID-19 can also cause a dry cough.
- Asthma: a dry cough at night can be a clue, sometimes with wheezing.
- Acid reflux (GERD): stomach acid can irritate your throat, especially when you lie down.
- Medicines: ACE inhibitors for blood pressure can cause a persistent dry cough.
In all of these, your airways are irritated but not filled with extra mucus, so the cough stays dry.
Key takeaway: Dry coughs usually come from irritation and inflammation without extra mucus.
What Causes a Wet Cough (Chesty, Productive Cough)?
A wet cough means your airways are making extra mucus and your body is trying to clear it.
- Cold or flu (later days): the cough can turn wet as mucus builds.
- Bronchitis: inflamed airways make thick phlegm—classic chesty cough.
- Pneumonia: lung infection usually brings fever and a deep, wet cough.
- Chronic lung disease: COPD and chronic bronchitis can cause a daily productive cough.
- Cystic fibrosis: thick, sticky mucus leads to frequent wet coughs.
- Post‑nasal drip: drainage from your nose/sinuses can make your cough feel wet.
Mucus can come from the upper airways (post‑nasal drip) or from the lungs during an infection in the lower airways. A wet cough that sticks around or keeps getting worse should be checked by a doctor.
Key takeaway: Wet coughs help you expel excess mucus from infection or chronic lung disease.
Dry vs Wet Cough Symptoms: How to Recognize Each
Dry cough signs:
- Tickle or itch in the back of your throat.
- Hacking or hoarse sound.
- Nothing (or almost nothing) comes up when you cough.
- Can feel worse at night.
Wet cough signs:
- Chesty, moist, or gurgly sound.
- You feel or hear mucus moving.
- You might feel like you need to spit out phlegm.
- It commonly comes with a stuffy nose or chest congestion.
Sound alone can be tricky. What sounds ‘wet’ to one person might seem ‘dry’ to another, so focus on whether you’re actually bringing up mucus.
Key takeaway: No phlegm and a tickle points to dry; phlegm and a chest rattle point to wet.
Treating a Dry Cough (Home Care and Medications)
Your goal is to calm the irritation.
- Sip warm fluids. Tea with honey can soothe your throat (honey is for adults and kids over 1).
- Use lozenges to keep your throat moist (not for young children due to choking risk).
- Run a cool‑mist humidifier and avoid smoke or strong fumes.
- Elevate your head at night to reduce the tickle.
- Some people use an OTC cough suppressant at bedtime (like dextromethorphan) when a dry cough keeps them from sleeping—ask your doctor or pharmacist what’s right for you. Cough and cold medicines aren’t recommended for young children; check with your child’s doctor before giving any.
- If allergies are the trigger, an antihistamine can help. If reflux is the cause, treating GERD can ease the cough.
- Expectorants don’t help a truly dry cough.
Safety note: Check with your doctor or pharmacist before starting any new medication.
Key takeaway: Soothe and, if needed, gently suppress a dry cough so you can rest.
Treating a Wet Cough (Clearing the Mucus)
Your goal is to thin and move the mucus—don’t shut the cough down.
- Hydrate well. Water and warm soups help thin phlegm.
- Use steam or a warm shower to loosen mucus. Don’t put medications in a steam inhaler—only use them in a nebulizer exactly as your doctor prescribes.
- An expectorant (like guaifenesin) is commonly used to make mucus easier to cough up—ask your doctor or pharmacist before choosing a medicine.
- Keep your head and chest slightly elevated when you rest.
- Gentle chest claps (if taught by your care team) can help loosen secretions.
- Nebulizer support: a portable mesh nebulizer like the TruNeb™ portable nebulizer can deliver normal saline or doctor‑recommended hypertonic saline (for example, 3%) to moisten airways and loosen thick mucus. Only use saline or medications in your nebulizer that your doctor has prescribed for you. Your doctor might also prescribe a nebulized medication if you have wheezing or chronic lung disease.
- Avoid heavy use of cough suppressants for a wet cough. Shutting down a wet cough too much can trap mucus in your lungs. If you need rest, clear mucus first, then use the smallest amount your doctor recommends.
Safety note: Talk to your doctor before trying a new medication. Cough and cold medicines aren’t recommended for young children; ask your child’s doctor before giving any over‑the‑counter cough medicine.
Key takeaway: For wet coughs, thin the mucus and let the cough do its job.
When to See a Doctor for a Cough
Most simple coughs improve with time and care.
- A cough that lasts more than a few weeks, or over 8 weeks in adults (chronic cough).
- High fever, shaking chills, night sweats, or unintended weight loss.
- Trouble breathing, fast breathing, or wheezing that won’t stop.
- Chest pain with breathing or coughing.
- Blood in your mucus, even small streaks.
- A weak immune system or lung disease and your cough is getting worse.
- Babies under 3 months: any cough. For older kids: fast breathing, dehydration, or a barking cough needs prompt care—call your child’s doctor right away.
⚠️ Call 911 or your local emergency number right away if you have severe trouble breathing, new chest pain, or blue lips or face. If you’re ever unsure, it’s safer to have a doctor check your cough.
Key takeaway: If a cough is severe, lasts weeks, or brings red flags like fever, pain, or blood, see a doctor.
Frequently Asked Questions
Tap or click a question below to see the answer:
Check for mucus. If you never bring up phlegm and it feels like a throat tickle, it’s likely dry. If you feel or cough up mucus, it’s wet. Sound can help but isn’t perfect, so focus on whether mucus actually comes up. Quick rule: If phlegm comes up, it’s wet; if not, it’s dry.
Suppressants are used for dry, irritating coughs (especially at night) and expectorants help thin mucus for wet, phlegmy coughs. Ask your doctor or pharmacist which option fits your symptoms and other medicines, and follow the label. Cough and cold medicines aren’t recommended for young children—check with your child’s doctor first.
Yes. Early in a cold, a cough can start dry and turn wet as mucus builds. As you recover, a dry “after‑cough” can linger for days or even weeks.
Neither type is automatically worse. What matters are red flags like breathing trouble, chest pain, blood in mucus, high fever, or a cough that lasts for weeks. See a doctor if you’re unsure or have any of these symptoms.
Conclusion: Dry coughs don’t bring up mucus and need soothing; wet coughs do bring up mucus and need help clearing it. Treat based on the type, and see a doctor for severe or long‑lasting symptoms.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk to your doctor about your symptoms and any treatments you’re considering.







