On this page
What “Chronic” and “Acute” Mean in Asthma
Asthma is a chronic lung disease. Chronic means long-term. Acute means a sudden, short-term flare-up. An acute flare is an asthma attack.
In other words, the difference between chronic and acute asthma is that 'chronic' refers to the ongoing condition, while 'acute' describes a sudden asthma attack.
Doctors call this an acute exacerbation. You live with the chronic condition day to day, and at times it can surge into an acute attack.
You might see medical codes: J45 for chronic asthma and J46 for a severe, stubborn attack called status asthmaticus.
Think of a campfire. The steady heat is the chronic part. A sudden burst of flame is the acute attack.
Asthma is different from chronic lung diseases like COPD and from infections like bronchitis or pneumonia.
Key takeaway: Asthma is chronic, and an acute episode is the sudden attack on top of it.
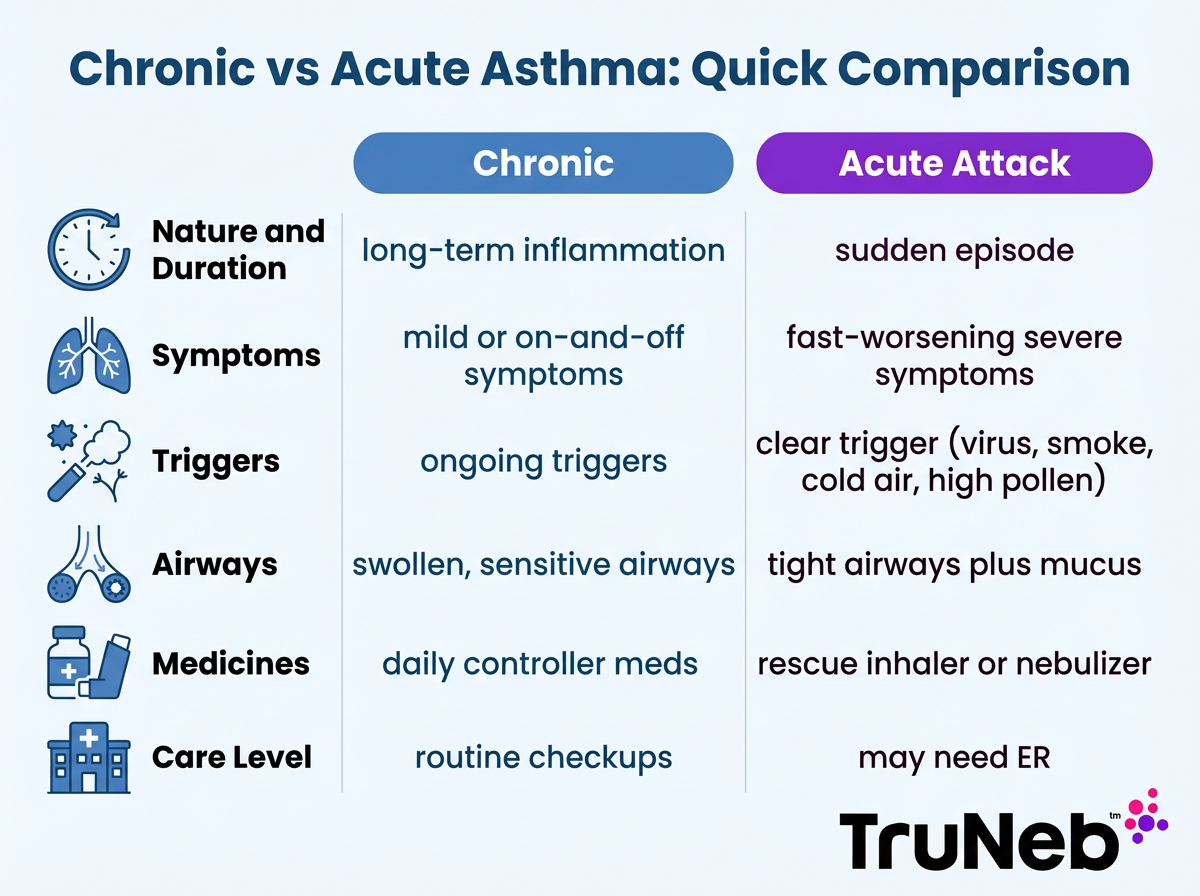
Chronic Asthma vs Acute Asthma at a Glance
Quick comparison
| Category | Chronic Asthma | Acute Asthma Attack |
|---|---|---|
| Nature and Duration | Ongoing condition with long-term airway inflammation. | Sudden episode that can last minutes to hours. |
| Symptom Pattern | Mild or on-and-off symptoms (night cough, wheeze with exercise). | Fast-worsening shortness of breath, louder wheeze, tight chest. |
| Triggers | Ongoing exposures keep airways sensitive (dust mites, smoke). | Clear spark like a cold, heavy pollen day, smoke, cold air, or hard exercise. |
| Airway State | Lining is swollen and sensitive most of the time. | Muscles tighten (bronchospasm), swelling spikes, more mucus. |
| Medicines | Daily controller medicines your doctor prescribes, like inhaled corticosteroids or combination inhalers. | Quick-relief bronchodilator by inhaler or nebulizer; short courses of oral steroids prescribed by a doctor for more severe attacks. |
| Care Level | Routine checkups to keep control. | Urgent or emergency care if severe or not improving. |
Put simply: Chronic is long-term control; acute is a sudden attack needing fast relief.
Symptoms: Daily Asthma Control vs Acute Attack Signs
Daily chronic symptoms:
- Cough that is worse at night or early morning.
- Mild wheeze with exercise or allergies.
- Shortness of breath that improves with rest and your usual rescue medicine when your asthma is well controlled.
Acute attack signs:
- Wheeze that gets loud and constant.
- Hard work of breathing with chest or neck retractions.
- Trouble speaking in full sentences.
- Feeling panicked because air won't move.
- In severe cases, lips or nails can look bluish.
Objective clue: A peak flow reading usually drops a lot during an attack. In a severe flare, it can fall below half of your usual best.
Daily asthma symptoms are usually milder and come and go, while acute attack signs are sudden, severe breathing problems that don't quickly improve with rescue medicine.
Triggers and Causes That Drive Each
Chronic drivers:
- Allergens you live with day to day (dust mites, pet dander, mold).
- Irritants such as smoke and air pollution.
- Weather shifts and strong odors.
- Skipping daily controller medicine can let inflammation build, which can raise your risk of an acute attack.
Acute sparks:
- Respiratory infections like a cold or flu are top triggers and can spark an acute asthma exacerbation.
- Cold, dry air or hard exercise without a warm-up.
- Smoke exposure, sprays, or strong perfume.
- Stress or big emotions that change breathing patterns.
Keep a simple symptom journal to spot your personal triggers and plan around them.
Chronic asthma is driven by ongoing exposures like allergens or smoke, while acute attacks typically follow a clear trigger such as a virus, heavy smoke, cold air, or a pollen spike.
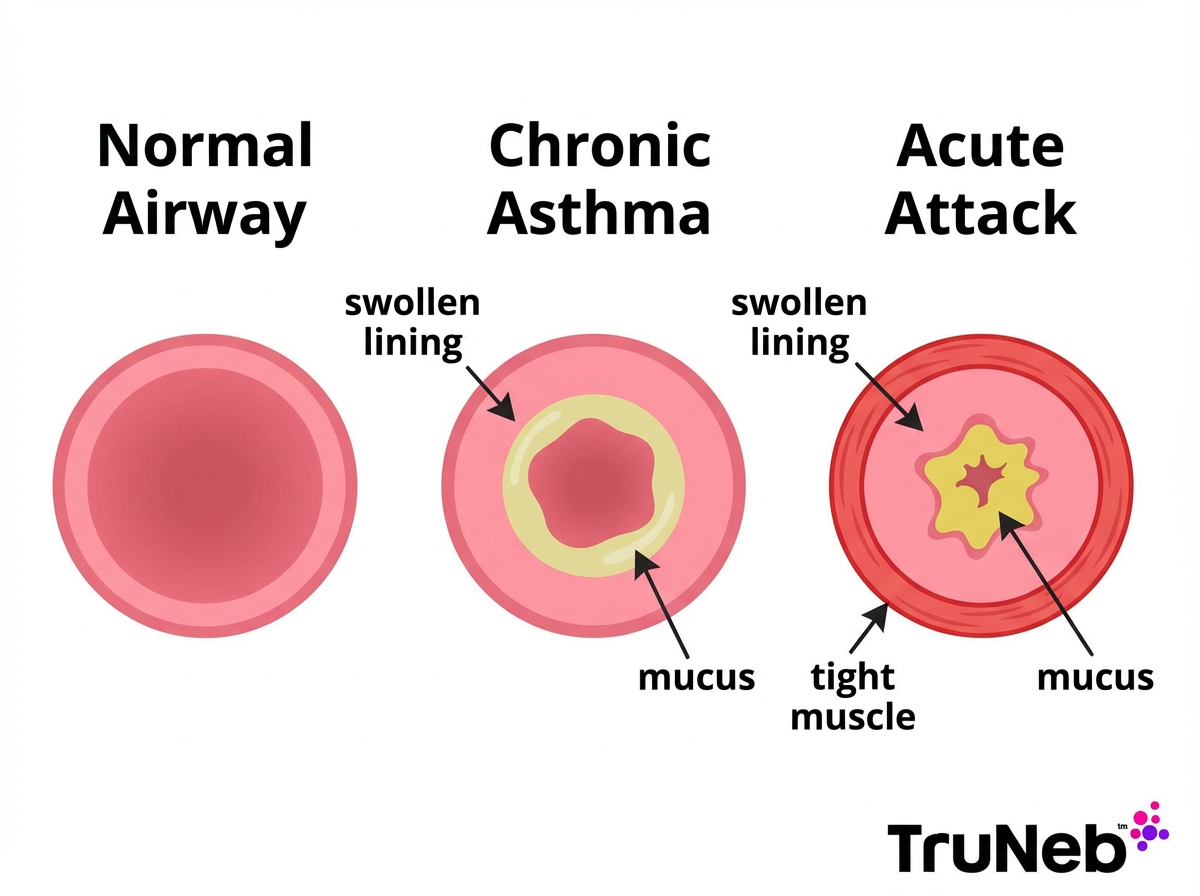
What Happens Inside the Airways
Chronic asthma:
- The airway lining stays inflamed and puffy.
- The airways make extra mucus.
- Nerves and muscles become hyperresponsive, so the tubes react easily.
Acute attack:
- The airway muscles clamp down suddenly (bronchospasm).
- Swelling increases and mucus can clog the narrowed tubes.
- Airflow drops, which causes wheeze or, in very severe cases, a "silent chest."
The good news: in asthma, blockage is usually reversible with proper treatment. Keeping inflammation low day to day lowers the chance of severe attacks. Frequent severe attacks can contribute to more chronic changes in the airways over time. This is the basic pathophysiology of chronic asthma compared to an acute attack.
Chronic asthma means inflamed airways; an acute attack adds sudden muscle tightness and mucus plugs.
Managing Chronic Asthma Day to Day
Your goal is steady control: fewer symptoms, better sleep, and fewer acute attacks.
Controller medicines:
- Inhaled corticosteroids are the foundation for most persistent asthma.
- Some people use an inhaled steroid plus a long-acting bronchodilator in one device.
- Leukotriene modifiers can help, especially with allergies.
- For some people with severe asthma that's not controlled by inhalers alone, biologic injections are used under specialist care.
Your doctor will decide which of these medicines make sense for your asthma; not everyone needs all of them.
Daily habits that help:
- Avoid smoke and known triggers. Use dust-mite covers and keep pets out of the bedroom if you are allergic.
- Stay active with a plan. Warm up before exercise. Many athletes with asthma compete at high levels.
- Get recommended vaccines, like the flu shot, to lower infection risk.
- Track control with a symptom log or peak flow as advised.
- See your doctor regularly to review your plan.
Device options:
- If you struggle with inhalers, ask your doctor if a home nebulizer is right for you. A portable mesh nebulizer can deliver prescribed medicines as a fine mist, which some people find easier.
- For stubborn mucus, your doctor might suggest nebulized saline, including hypertonic saline, in select cases. This is not routine for everyone.
- ⚠️ You might see products labeled 'steam inhaler' near nebulizers, but they're not designed for breathing in prescription asthma medicines.
Safety note: Don't start, stop, or change any medicine on your own. Talk to your doctor before trying a new medication.
Daily controller meds plus smart trigger control keep chronic asthma stable and cut attack risk.
Responding to an Acute Asthma Attack
Act early. Small problems are easier to turn around than severe ones.
Your asthma action plan from your doctor will usually include steps like these. In general, those plans say to:
Step by step:
- Stop activity and sit upright.
- Use your rescue inhaler with a spacer if you have one. Take slow, steady breaths as directed in your plan.
- Try to stay calm. Pursed-lip breathing can help.
- Get away from the trigger if you can and into clean air.
- If your plan includes it and your doctor has prescribed it, use your home nebulizer for quick-relief medicine. A portable mesh nebulizer, like TruNeb, can be easier to breathe from during a bad flare.
- If you track peak flow, a sudden drop toward yellow or red is another warning sign.
- If symptoms are not improving after rescue medicine, or return quickly, follow your action plan for next steps and seek medical care.
Important: If symptoms are severe, don't wait. Call 911.
During an acute asthma attack, quick-relief medicine and following your written asthma action plan are key to getting symptoms under control and knowing when to seek help.
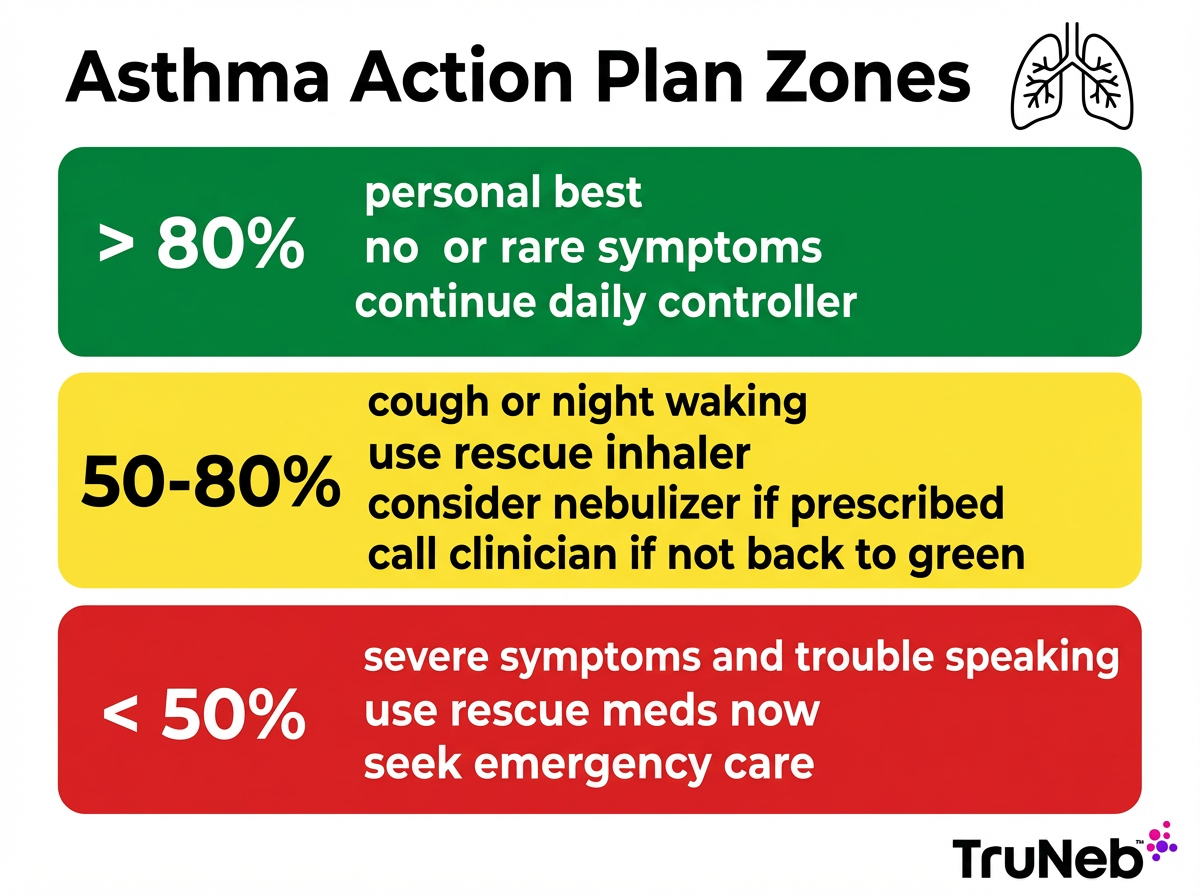
Asthma Action Plan With Green, Yellow, and Red Zones
An asthma action plan is a written guide from your doctor. It tells you what to do every day and what to do when symptoms change. Plans can also be symptom-based if you don't use a peak flow meter.
- Green Zone: You feel well. Peak flow is usually above 80 percent of your personal best. Keep taking your daily controller medicine.
- Yellow Zone: Symptoms are starting or getting worse, or peak flow is about 50 to 80 percent. Use your rescue medicine and follow the step-up directions in your plan. Check in with your doctor if you aren't back in green soon.
- Red Zone: Severe symptoms or peak flow below 50 percent. Use rescue medicine now and seek emergency care.
Written action plans are linked to fewer emergency visits.
Key numbers: Green > 80 percent, Yellow 50 to 80 percent, Red < 50 percent of your personal best.
When To Call the Doctor or Go to the ER
⚠️ If you have severe trouble breathing, bluish lips or face, or can't speak in full sentences—even after rescue medicine—call 911 or your local emergency number right away.
Call 911 or go to the ER if any of these happen:
- You can't speak in full sentences.
- Your lips or face look bluish.
- Your chest or neck skin pulls in with each breath.
- You feel drowsy or confused.
- Your peak flow stays in the red zone after medicine.
- Your rescue medicine isn't helping or relief lasts only a few minutes.
After any serious attack, schedule a follow-up. Your long-term plan might need an update.
If rescue medicine isn't helping and you can't speak in full sentences, call 911.
Living With Asthma and Staying Prepared
Most people live full, active lives with asthma. Being prepared with a plan and your rescue medicines makes a big difference.
Simple habits:
- Carry your rescue inhaler and spacer every day.
- Keep backups at home, school, or work if needed.
- Consider a compact portable nebulizer for travel or for times an inhaler is hard to use. A device like TruNeb can fit in a bag and deliver prescribed medicine as a fine mist.
- Review your action plan at least once a year or after any flare.
- Asthma can change over time, so your plan and medicines need periodic review.
- Stay up to date on vaccines and wash hands frequently during cold and flu season.
With a plan and the right tools, you can keep asthma in the green zone most of the time.
Frequently Asked Questions
Tap or click a question below to see the answer:
Asthma is a chronic illness. Acute refers to a sudden attack on top of the chronic condition. Put simply, the difference between chronic and acute asthma is that the chronic part is the ongoing tendency for inflamed airways, and the acute part is a sudden asthma attack. With good control, you can have long stretches with few or no symptoms, but the tendency for airway inflammation remains.
People sometimes say two types to mean allergic and nonallergic, or intermittent and persistent. Acute asthma isn't a separate type—it describes an attack that can happen in any type of asthma.
There is no confirmed cure, but asthma can improve or go into remission. Many people have long periods with few symptoms. Keep taking medicines as directed until your doctor changes the plan.
Attacks escalate quickly, your rescue inhaler helps little or for a short time, and talking or walking gets hard. A peak flow drop into yellow or red is another clue. When in doubt, follow your action plan for an attack.
A rescue inhaler with a spacer works fast for most people. A nebulizer can be just as effective and is helpful if you can't use an inhaler well, such as during a bad flare or for young children. Use the device your doctor prescribed in your plan.
It is a severe asthma attack that doesn't respond to usual rescue treatment. It is a medical emergency and needs urgent care.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms, medications, and asthma action plan.