On this page
What Is Croup?
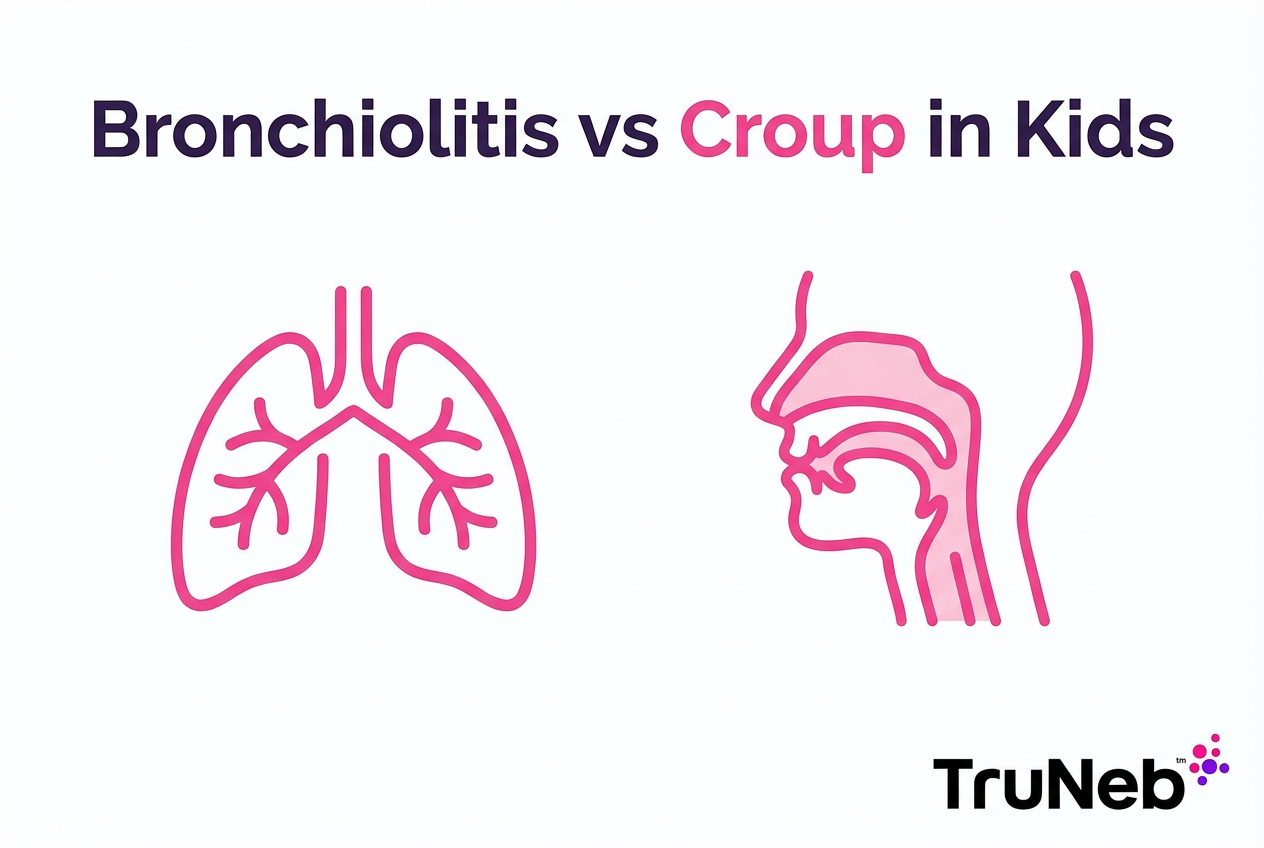
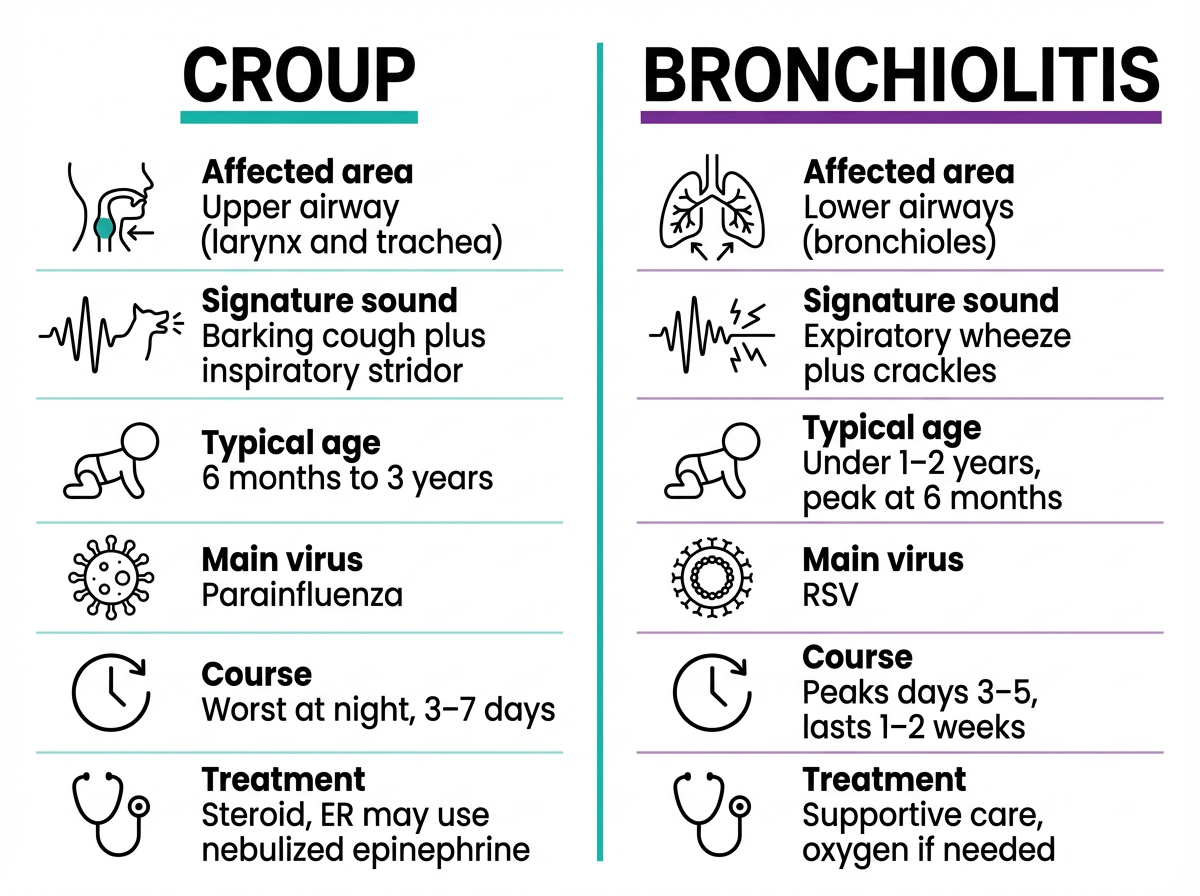
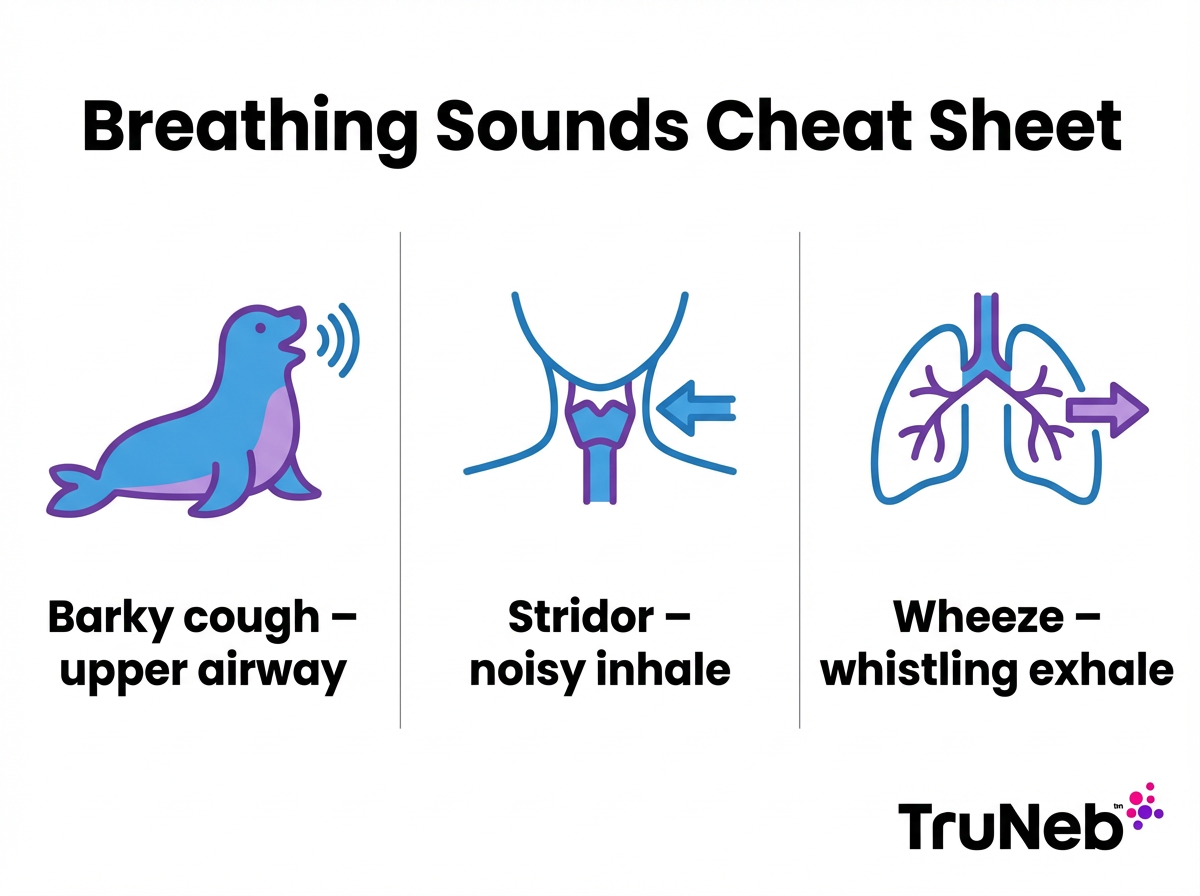
Croup is a viral swelling of the upper airway around the voice box and windpipe. The narrowed airway causes a barking, seal-like cough. Kids can also make a harsh, high-pitched noise on the inhale called stridor. Croup usually starts like a cold, then gets louder at night.
It is most common from 6 months to 3 years. Parainfluenza virus is the usual cause, but RSV or influenza can trigger it too. Croup is contagious and spreads like a cold through coughs, sneezes, and touch. Doctors sometimes call it laryngotracheitis (swelling around the voice box and windpipe).
In one line: Croup is an upper-airway illness that causes a barky cough and stridor.
What Is Bronchiolitis?
Bronchiolitis is a lung infection in infants that inflames the tiny air tubes called bronchioles. Swelling and mucus make breathing harder. Babies develop a wet cough, congestion, fast breathing, and wheezing. It usually starts like a cold and worsens over a few days, peaking around day four or five.
RSV is the main cause, especially in winter, though other viruses can do it. It spreads like a cold through droplets and touch. Bronchiolitis is most common under age two, with a peak around six months. Bronchiolitis is a common reason babies are hospitalized for breathing trouble.
In one line: Bronchiolitis is an infant lung infection of the small airways that leads to cough, congestion, and wheezing.
Causes and Contagiousness
Both croup and bronchiolitis are caused by viruses and both are contagious. Croup is most commonly from parainfluenza. RSV, influenza, and adenovirus can cause it too. Bronchiolitis is usually from Respiratory Syncytial Virus (RSV). Rhinovirus and human metapneumovirus also play a role.
These germs spread through droplets from coughs and sneezes and by touch. Daycare, shared toys, and close contact make spread easy. Croup tends to show up in fall and early winter. RSV bronchiolitis surges in winter. Good handwashing, covering coughs, cleaning shared items, and keeping a sick child home during the worst days help reduce spread. Parents sometimes hear 'RSV' and think it’s a type of croup, but in RSV bronchiolitis vs croup, RSV most commonly causes bronchiolitis in babies and only occasionally triggers croup-like symptoms in older children.
In one line: Parainfluenza commonly triggers croup and RSV drives bronchiolitis, and both spread like a cold.
Symptoms: Barky Cough vs Wheezing
The type of cough or breathing noise gives big clues about bronchiolitis vs croup symptoms.
Croup usually starts with a runny nose, then a sudden barking cough that sounds like a seal. The voice can be hoarse. When the airway is tight, you might hear stridor, a harsh sound when your child breathes in. Nights are usually worse. Fever is typically mild.
Bronchiolitis is different. Babies breathe fast and shallow, and you might see the skin pull in between the ribs and nasal flaring. The cough is wet, with lots of congestion. The key sound is wheezing, a whistling or raspy noise when breathing out. Feeding can be hard because breathing takes work.
Key point: Stridor is a noisy inhale from the throat, while wheeze is a whistling exhale from the lungs.
In one line: Croup and bronchiolitis are two different illnesses: think bark and harsh inhale for croup, and wheeze with fast breathing for bronchiolitis.
Illness Course and Duration
Croup is usually short-lived. After a day or two of cold symptoms, the barky cough and stridor are worst for one or two nights, then improve. Most cases get much better within three days and are gone within a week. With croup, nights tend to be the worst early on.
Bronchiolitis builds more slowly. Symptoms usually worsen on days two to three, peak around days four to five, and then ease. Most infants need one to two weeks to recover, and the cough may linger a bit longer. In bronchiolitis, breathing tends to stay rough over several days before turning the corner.
In one line: Croup often improves within three to seven days, while bronchiolitis commonly lasts one to two weeks.
Home Care: Managing Croup and Bronchiolitis
For croup, keeping your child calm matters because crying can tighten the airway. A cool mist humidifier can make breathing feel easier for some kids. Spending a few minutes in a steamy bathroom (steam from a running shower, with your child away from hot water) or a brief step into cool night air can ease a croupy cough. Offer fluids as tolerated. Watch closely at night when symptoms tend to flare.
For bronchiolitis, clearing the nose before feeds and sleep with saline drops and gentle suction can help. A cool mist humidifier can ease congestion. Small, frequent feeds support hydration. Keep smoke and strong odors away. Over-the-counter cough and cold medicines aren’t recommended for infants.
⚠️ Steam inhalers are not the same as nebulizers and should not be used to deliver breathing medications. Steam is for comfort only, and too-hot steam can burn a child.
In one line: Use humidified air and calm for croup and use saline, suction, and small frequent feeds for bronchiolitis.
When to See a Doctor or Go to the ER
Here’s when you need to go in right away. These red flags apply to both croup and bronchiolitis; drooling or trouble swallowing can signal an upper-airway emergency.
⚠️ If your child has any of the signs below, seek emergency medical care right away.
- Noisy breathing at rest (stridor when calm) or pauses in breathing.
- Blue or gray lips or face, or your child looks very pale or limp.
- Strong pulling-in of the skin between the ribs or at the collarbone with each breath.
- Very fast breathing (about 60 breaths per minute or more in an infant) or severe effort to breathe.
- Drooling or trouble swallowing, or your child cannot speak or cry due to breathing trouble.
- Poor feeding with signs of dehydration (very few wet diapers, very sleepy, or hard to wake).
If none of these are present but you’re worried, call your pediatrician for advice. If you’re ever unsure, it’s always safest to call your doctor or local emergency number.
In one line: With croup or bronchiolitis, go to the ER for noisy breathing at rest, blue lips, severe work of breathing, or poor feeding in a baby.
Treatment by Doctors: Croup vs Bronchiolitis
Croup usually improves with medicine that reduces swelling. In clinics and ERs, doctors usually give a single dose of dexamethasone, a steroid that opens the upper airway. If a child has severe croup with stridor at rest, nebulized epinephrine can be used in the ER for quick, short-term relief while the steroid takes effect.
Bronchiolitis has no quick cure. Care focuses on oxygen if levels are low and fluids if a baby is dehydrated. Some clinicians try a bronchodilator such as albuterol, but most infants do not improve with it. Current guidelines don’t recommend routine bronchodilators for bronchiolitis; at most, a brief trial may be used and stopped if there’s no clear benefit. Supportive care and time are the main treatments, and most babies recover without hospital admission.
In one line: Doctors use steroids for croup swelling, while bronchiolitis care is mostly oxygen, fluids, and time.
Nebulizer Use: Do They Help With Croup or Bronchiolitis?
Parents often ask if a home nebulizer will help. For croup, the main problem is swelling above the lungs. Albuterol, a lower-airway bronchodilator, usually does not help that. In severe croup, ER teams use nebulized epinephrine for short-term relief while the steroid takes effect.
Bronchiolitis is a lower-airway problem. Some doctors try a short trial of albuterol for wheezing and stop if there is no clear benefit. In certain cases, a clinician might recommend nebulized saline, especially hypertonic saline (3% or 7%), but this is mainly used in clinical settings and should only be used if prescribed. If your child is prescribed a breathing treatment, a quiet, portable mesh nebulizer like the TruNeb™ portable nebulizer can make sessions easier for little ones at home. Your pediatrician can also recommend medical-grade saline when appropriate.
Key point: Home albuterol usually does not help croup because the swelling sits above the lungs.
Safety note: Talk to your doctor before trying a new medication or nebulized saline. Hypertonic saline should only be used if your child’s doctor recommends it. A nebulizer is a way to deliver prescribed medicines, not a cure by itself.
In one line: Home nebulizers do not treat croup swelling but may be used for wheezy bronchiolitis if your doctor advises.
Frequently Asked Questions
Tap or click a question below to see the answer:
Croup affects the upper airway and causes a barky cough and stridor. Bronchiolitis affects the small airways in the lungs and causes wheezing and fast breathing. They tend to affect different ages too, with croup in toddlers and bronchiolitis in infants.
No. RSV is a virus, while bronchiolitis is the illness RSV commonly causes in babies. Older kids usually just have a cold, but infants can wheeze.
Yes. Croup is viral and spreads like a cold through coughs, sneezes, and touch. Good hand hygiene helps reduce spread.
It’s uncommon, but viruses can cause mixed symptoms. Doctors focus on the dominant pattern to guide care.
No. Both are usually viral, so antibiotics don’t help. Doctors treat swelling in croup and give supportive care for bronchiolitis.
Keep your child calm. A steamy bathroom (keep your child away from hot water), a brief step into cool night air, a cool mist humidifier, and fluids as tolerated can help. Seek urgent care if breathing sounds bad when your child is calm, or if they seem to be working hard to breathe.
Blue or gray lips, noisy breathing at rest, or severe work of breathing are top warning signs. See the “When to See a Doctor or Go to the ER” section above for the full list of warning signs.
Not unless your pediatrician suggests it for wheezing or saline treatments. Most croup and bronchiolitis cases don’t need a home nebulizer.
Asthma causes recurrent wheezing (usually in older children) and typically responds to albuterol. Whooping cough (pertussis) causes weeks of coughing fits with a “whoop” and sometimes vomiting. If you’re unsure, talk to your doctor.
In one line: Use the sound and your child’s breathing effort to guide next steps with suspected croup or bronchiolitis, and call your pediatrician if unsure.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about any questions or concerns you have about your child’s health.