On this page
Is bronchiectasis the same as COPD?
Bronchiectasis and COPD are two different chronic lung diseases that can share symptoms but develop for different reasons and are managed in different ways.
When people search for "bronchiectasis vs COPD," they’re really asking whether these are the same disease or two different problems.
No. Bronchiectasis is a separate disease—it isn't a type of COPD.
Bronchiectasis means the bronchial tubes are permanently widened and scarred after damage, usually from past infections. Thick mucus builds up, and lung infections tend to come back.
COPD (chronic obstructive pulmonary disease) is an umbrella term, mainly emphysema and chronic bronchitis. It usually comes from years of smoke or irritant exposure. Air sacs and small airways are damaged, so it becomes hard to push air out.
The key difference between bronchiectasis and COPD is where the lung damage occurs and what originally caused it.
A simple way to picture it: bronchiectasis is like widened, damaged pipes that collect gunk; COPD is like narrowed pipes and worn-out filters from long-term irritation.
They can share symptoms like cough and shortness of breath, which causes confusion. But their causes, tests, and daily care are not the same. This distinction matters because the tests and treatments differ, and mislabeling can delay the right care.
Causes and Risk Factors: Bronchiectasis vs COPD
Bronchiectasis Causes
- Repeated or severe lung infections such as pneumonia or tuberculosis
- Immune system problems (such as immune deficiency conditions) or cilia disorders
- Genetic conditions like cystic fibrosis
- Sometimes no clear cause is found, but long-standing airway inflammation is common
COPD Causes
- Long-term exposure to irritants, especially cigarette smoking
- Secondhand smoke, workplace dust or chemicals, and heavy air pollution
- Biomass smoke from wood or coal stoves
- Rarely, alpha‑1 antitrypsin deficiency
In simple terms, COPD usually comes from years of breathing in irritants like cigarette smoke, while bronchiectasis usually follows infections or other damage that permanently widens the airways. You can never smoke and still develop bronchiectasis.
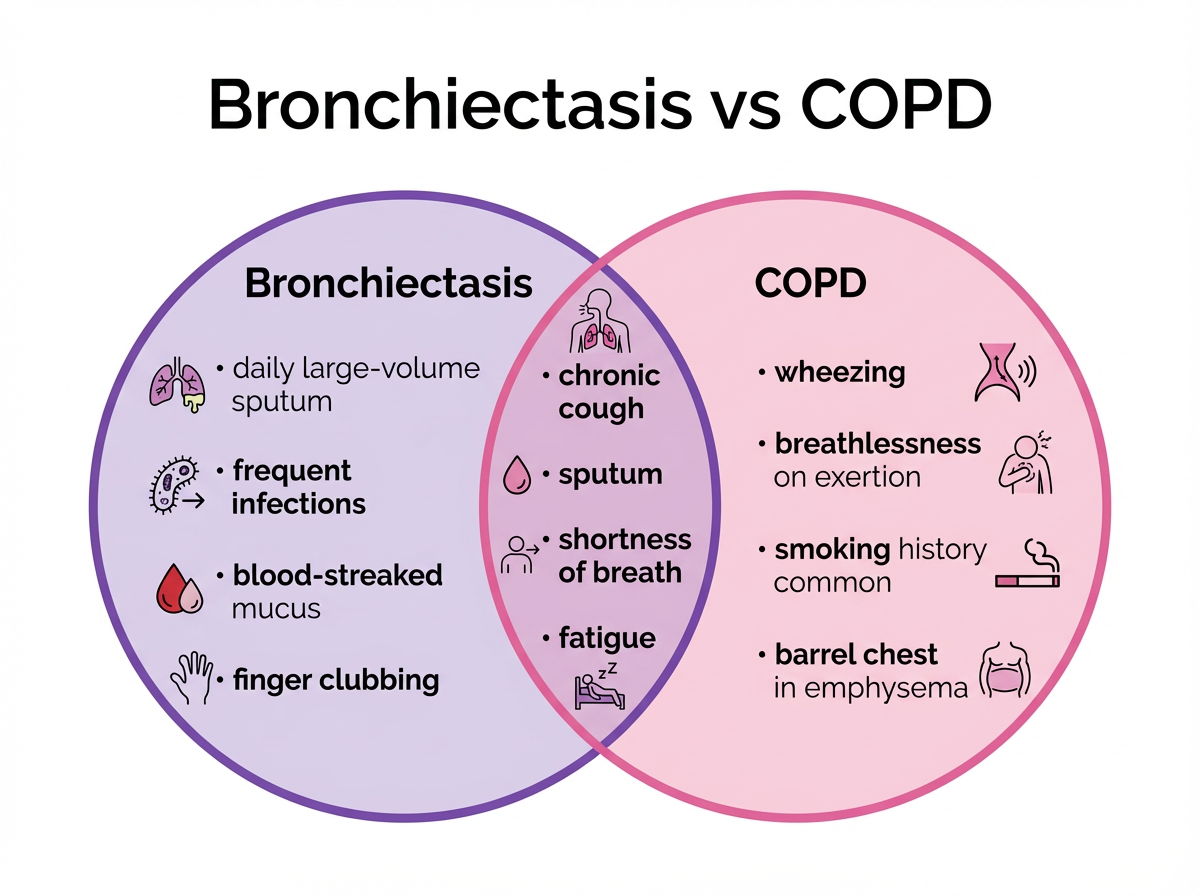
Symptoms and Signs: Bronchiectasis vs COPD
If you have either condition, you might notice a daily cough and shortness of breath; the pattern of your symptoms tells your doctor more.
Bronchiectasis Symptoms
- Daily, heavy mucus that is yellow or green
- Frequent chest infections and flare-ups
- Possible blood-streaked mucus during infections
- Fever and feeling generally unwell during flares
- Crackles on exam and sometimes finger clubbing over time
COPD Symptoms
- Breathlessness on exertion, especially early in emphysema
- Wheezing and chest tightness from narrowed airways
- Cough with mucus in chronic bronchitis, usually with less day to day volume than bronchiectasis
- Fatigue and exercise intolerance that slowly worsen
- Symptoms usually appear gradually over years, especially in people who smoke
As a rule of thumb, lots of thick, colored mucus and repeated infections point more to bronchiectasis, while wheeze and trouble exhaling point more to COPD—especially if there’s a smoking history.
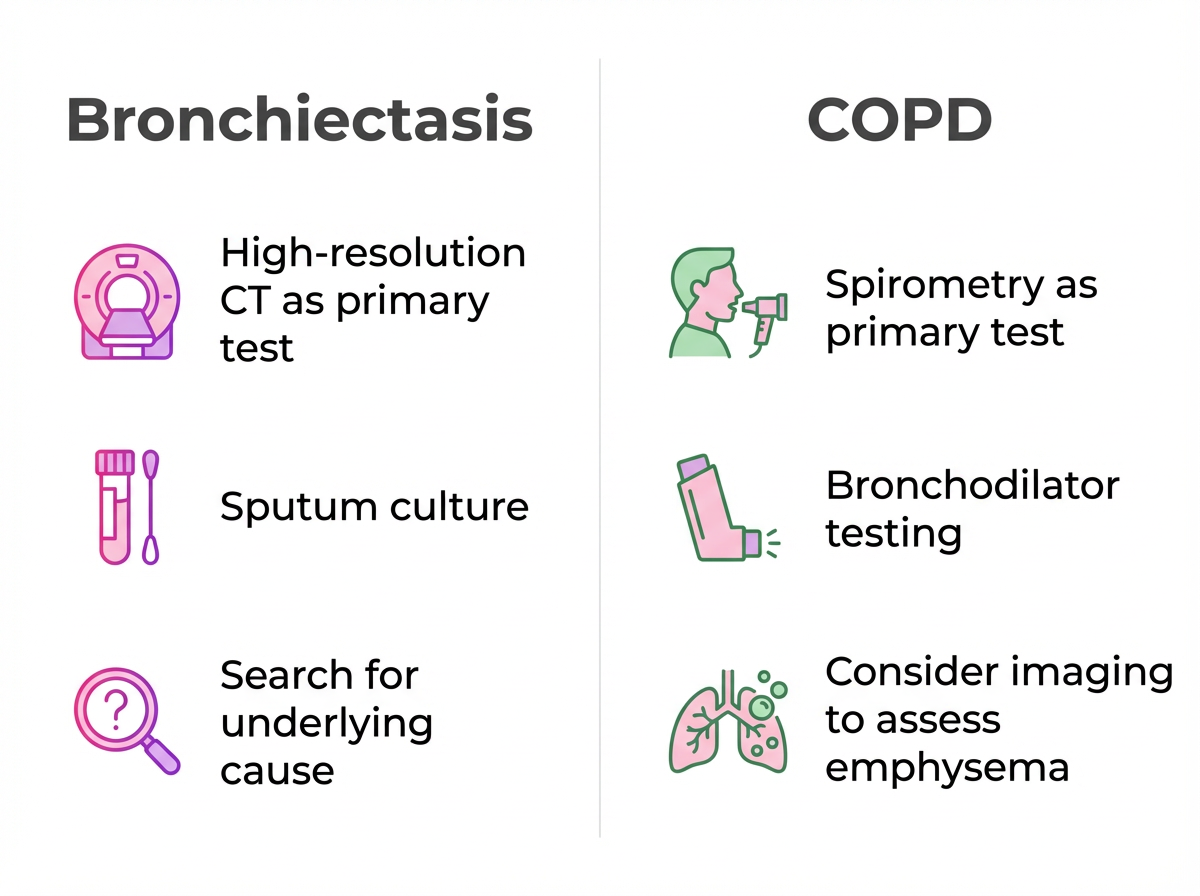
Diagnosis: Bronchiectasis vs COPD
How Doctors Confirm COPD
- Spirometry breathing test is key
- A low post‑bronchodilator FEV1/FVC ratio shows airflow blockage
- Imaging can help assess emphysema, but spirometry plus history usually make the diagnosis
How Doctors Confirm Bronchiectasis
- High‑resolution CT scan shows widened, thick-walled airways and mucus plugging
- Spirometry may also show obstruction, so imaging is essential for bronchiectasis
- Sputum cultures and blood tests can help find causes and guide antibiotics
Spirometry can show obstruction in both COPD and bronchiectasis; the CT scan is what confirms bronchiectasis.
COPD is mainly confirmed with spirometry breathing tests, while bronchiectasis is confirmed with a high‑resolution CT scan that shows widened, mucus‑filled airways.
If you were told you have COPD but you make a lot of mucus or keep getting chest infections, ask if a CT scan is needed to check for bronchiectasis. Consider seeing a lung specialist (pulmonologist) if infections are frequent or the diagnosis isn't clear.
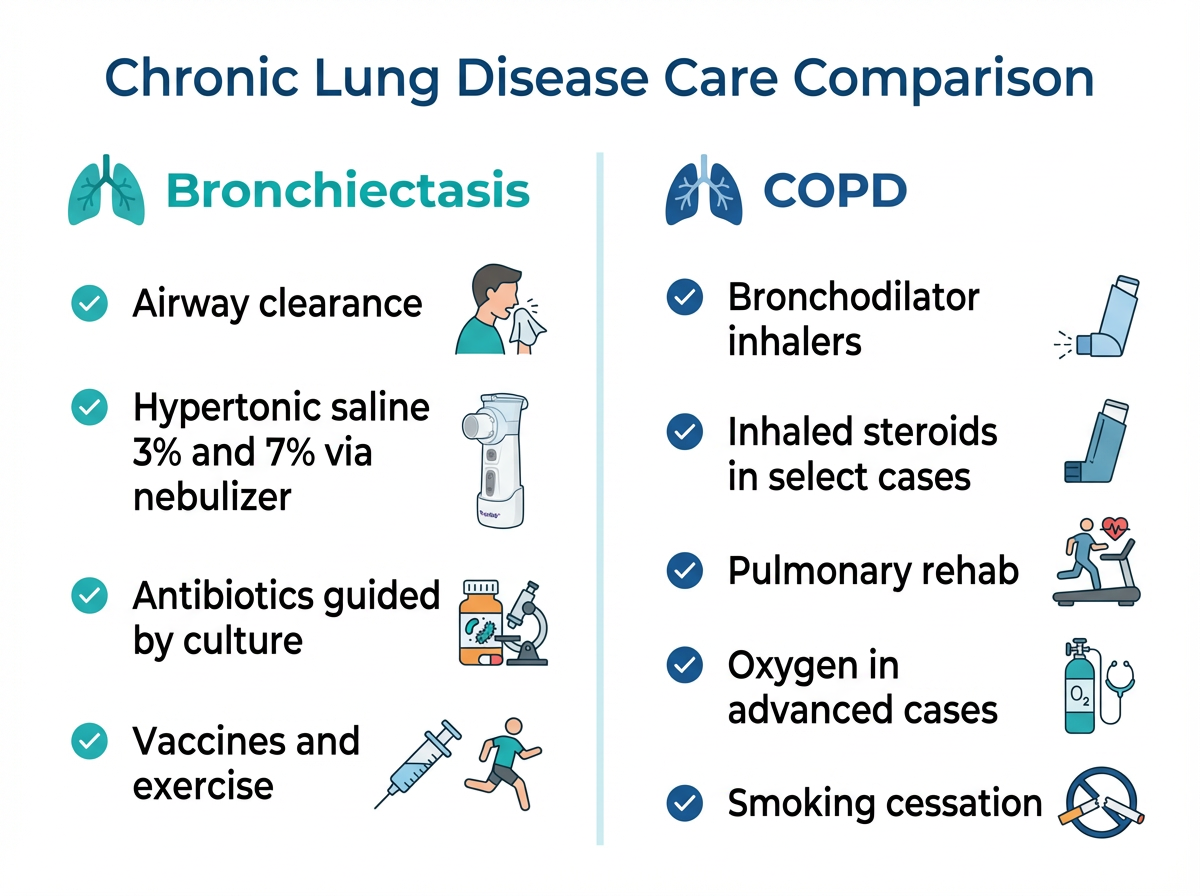
Treatment and Management: Bronchiectasis vs COPD
When you look at bronchiectasis vs COPD treatment options, the focus of care is different for each condition.
Treating bronchiectasis focuses on clearing mucus and preventing infections, while COPD treatment centers on opening narrowed airways and easing breathlessness.
⚠️ If you have sudden severe shortness of breath, chest pain, confusion, or blue lips or face, seek emergency medical care right away.
Talk to your doctor if your cough, mucus, or breathlessness suddenly worsens, you’re needing antibiotics more often, or your usual treatments aren’t working as well.
Bronchiectasis Treatment Focus
- Daily airway clearance routines to help move mucus
- Nebulized hypertonic saline to thin mucus (prescription therapy)
- Antibiotics for flare-ups and sometimes long-term plans based on sputum cultures
- Bronchodilators if airway narrowing is present, plus exercise, hydration, and vaccines
Airway clearance can include breathing techniques, chest physiotherapy, or devices that help move mucus out of the lungs.
COPD Treatment Focus
- Inhaled bronchodilators for relief and daily control; inhaled steroids in select cases
- Pulmonary rehabilitation to build strength and ease breathlessness
- Oxygen therapy in more advanced disease
- Quitting smoking and avoiding irritants to slow decline
For people who smoke, quitting is the most powerful step to slow COPD progression. Treatment plans are individualized; not everyone needs oxygen or steroids.
TruNeb™ nebulizers can deliver bronchodilators or saline as a fine mist at home or on the go. If your doctor recommends hypertonic saline, 3% is gentler while 7% is stronger; your care team will help you choose what you tolerate best. Hypertonic saline is a prescription therapy your doctor might add to your plan to help thin mucus.
⚠️ Don’t use a steam inhaler for prescription breathing medications—these devices aren’t designed to deliver nebulized drugs safely.
Safety note: Talk to your doctor before trying a new medication or hypertonic saline. Do not start, stop, or change prescriptions or doses on your own.
Similarities and Overlap of Bronchiectasis and COPD
These are both chronic, obstructive lung diseases. They share cough, sputum, and shortness of breath. They also flare, especially with infections, and benefit from vaccines, regular activity, and pulmonary rehab.
Takeaway: Both bronchiectasis and COPD are long-term lung diseases that cause cough, sputum, and shortness of breath and tend to flare up when infections or irritants trigger them.
At a glance: Bronchiectasis vs COPD — different root causes and tests lead to different care.
| Feature | Bronchiectasis | COPD |
|---|---|---|
| Main cause | Usually follows lung infections, immune or cilia problems, or other airway injury | Years of irritant exposure (most commonly cigarette smoke); rare genetic causes |
| Where damage occurs | Widened, scarred bronchial tubes with mucus build-up | Damaged air sacs and narrowed small airways |
| Hallmark symptoms | Daily large-volume, colored sputum; frequent chest infections | Wheeze, breathlessness on exertion; chronic cough (usually less sputum) |
| Key test | High-resolution chest CT | Spirometry (post-bronchodilator FEV1/FVC) |
| Core treatment focus | Airway clearance and infection prevention | Bronchodilators, rehab, and symptom relief |
Note: Some people have features of both conditions.
Sometimes, they occur together. In moderate to severe COPD (more advanced stages), studies report a large share of people have bronchiectasis visible on CT scans; in one study, nearly half did. Doctors sometimes call this pattern bronchiectasis–COPD overlap syndrome (BCOS). Overlap is linked with more infections, more flare-ups, and higher risk of hospital visits.
Care must cover both sides of the problem: bronchodilators and rehab for COPD, plus airway clearance and infection control for bronchiectasis. If you’re living with COPD and find you’re bringing up a lot of mucus or keep getting chest infections, it’s reasonable to ask whether bronchiectasis could also be present.
A note on related conditions: asthma is another chronic airway disease that can overlap with these, but it’s distinct and not the focus here. Researchers are exploring clearer ways—such as the ROSE criteria—to spot overlap earlier so treatment can be tailored.
Frequently Asked Questions
Tap or click a question below to see the answer:
No. Bronchiectasis is a separate disease—it isn’t a type of COPD. It involves damaged, widened airways, usually after infections, while COPD describes long-term lung damage from irritants like smoking, including emphysema and chronic bronchitis.
Yes. Some people with moderate to severe COPD also have bronchiectasis on CT scans. When both are present, people tend to have more mucus and flare-ups, so doctors usually treat both together.
Thick, colored mucus every day and frequent chest infections point to bronchiectasis. Wheeze and breathlessness on exertion fit COPD more, especially with a smoking history. Blood-streaked mucus during flares is a red flag for bronchiectasis.
COPD is diagnosed with spirometry, a simple breathing test. Bronchiectasis is confirmed by a high-resolution CT scan that shows widened, mucus-filled airways. Spirometry can look obstructed in both, so CT is crucial for bronchiectasis.
Bronchiectasis does not literally turn into COPD, but the two conditions can develop in the same person over time. People with bronchiectasis who smoke can develop COPD, and years of COPD damage and infections can contribute to bronchiectasis.
Both are serious and can limit daily life. COPD is common and can be life‑threatening if not managed. Bronchiectasis ranges from mild to severe, but symptoms can usually be managed with the right combination of treatments. When both are present, illness tends to be more severe.
No. The airway damage is permanent, but symptoms can be managed with airway clearance, medicines, exercise, and infection control. COPD is also treatable but not curable. Talk to your doctor before trying new therapies.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk to your doctor about your symptoms, test results, and treatment options.