On this page
How long does it take to recover from a pulmonary embolism?
Most people start to feel better within a few days of treatment. Full recovery from a pulmonary embolism (a blood clot in the lung) typically takes weeks to a few months, and sometimes up to 6–12 months if the clot was large or there are other health issues.
In the first days, chest pain and shortness of breath usually ease once blood thinners start working. Your body then slowly breaks down the clot over weeks to months. Recovery means getting back to your usual activities and energy.
Most people feel better in days, but full recovery from a pulmonary embolism typically takes weeks to a few months, and sometimes up to a year for severe cases.
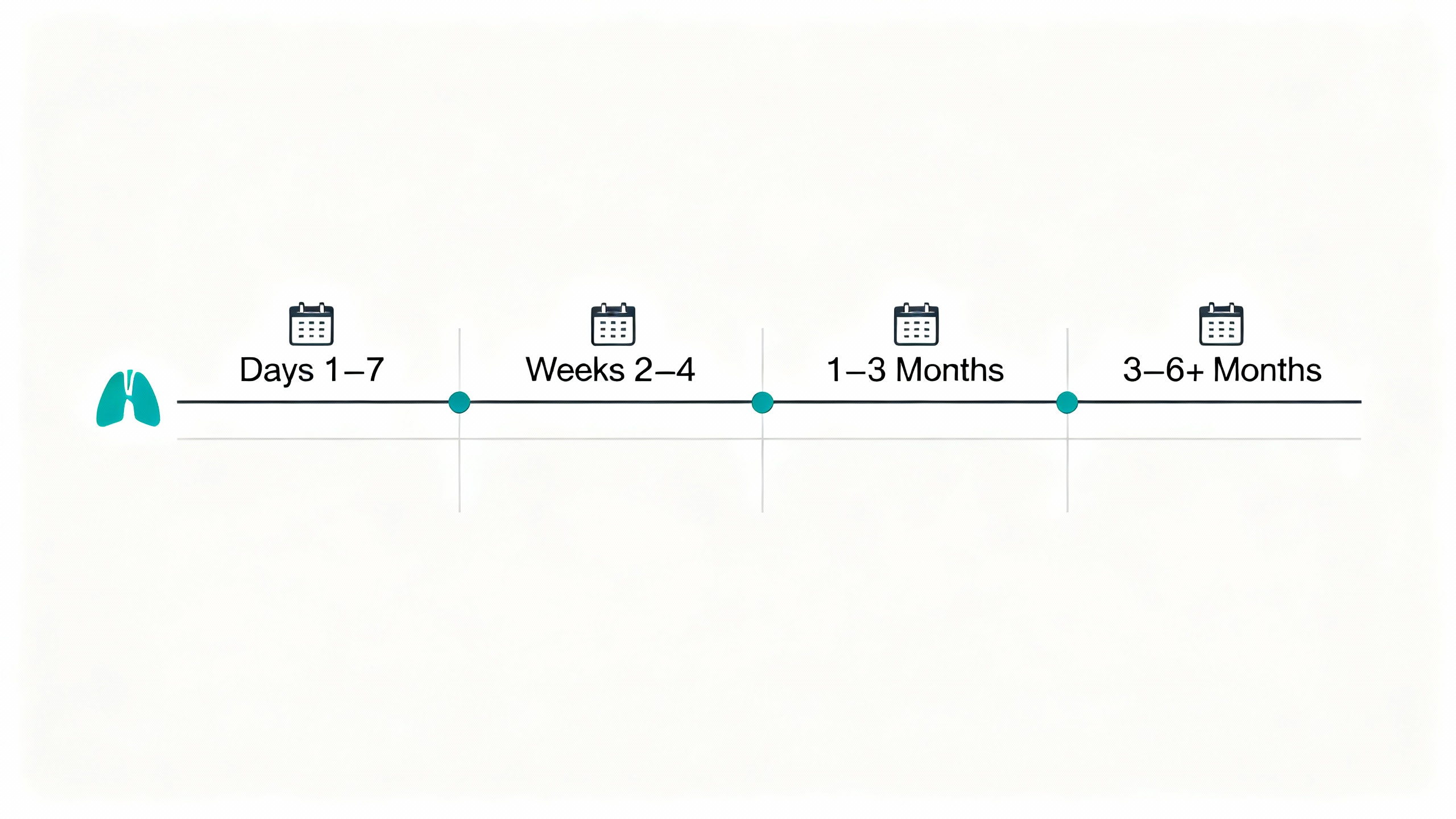
Stages of recovery from a blood clot in the lung
Days 1–7: The acute phase
Treatment starts in the hospital or at home if your case is low risk. Blood thinners begin protecting you. Most people notice easier breathing and less chest pain within a few days.
Weeks 2–4: Early recovery
You’re home on medication. Walking and simple tasks feel a bit easier each week. Fatigue is common. Gentle movement helps, but stop if symptoms spike. If stamina still lags at 6–8 weeks, your doctor can consider a referral to pulmonary rehab.
1–3 months: Subacute recovery
Most daily activities return. By about 3 months the clot is usually largely absorbed. Your doctor typically reviews your anticoagulation plan around this time.
Beyond 3 months: Extended recovery
Most people feel close to normal. If shortness of breath or low stamina linger, your doctor can check for uncommon issues like chronic lung vessel pressure.
Pulmonary embolism recovery improves in phases—from relief in the first week to near-normal activities by about three months for most people.
Anticoagulants prevent clot growth; your body dissolves the clot over weeks to months.Typical treatment duration is at least 3 months.Light activity is encouraged early unless your doctor advises otherwise. Sources: American Heart Association
| Phase | Timeframe | What you may feel | What to do |
|---|---|---|---|
| Acute | Days 1–7 | Chest pain and shortness of breath start to ease | Start/continue anticoagulants; oxygen/monitoring if needed; short, easy walks |
| Early recovery | Weeks 2–4 | Steady gains; fatigue common with exertion | Gentle walking; keep meds on schedule; rest as needed |
| Subacute | 1–3 months | Most daily tasks return; stamina builds | Follow-up visit(s); review anticoagulant plan |
| Extended | 3–6+ months | Near-normal for most; lingering symptoms may fade | Reassess meds; consider pulmonary rehab if symptoms persist |
Note: Timelines vary by clot size, overall health, and any complications.
Treatment and hospital care in the early days
Some low-risk pulmonary embolisms are treated at home with close follow-up. Others need a short hospital stay, typically a few days, to start anticoagulants and watch oxygen levels; length of stay varies by severity. Severe cases can need ICU care, clot-busting medicine, or a catheter procedure.
In rare situations where blood thinners aren’t an option, doctors sometimes place an inferior vena cava (IVC) filter to reduce the risk of a clot reaching the lungs.
Most people go home once they’re stable on pills and safe to recover outside the hospital.
Low-risk pulmonary embolisms can be treated at home, while higher-risk cases can need several days in the hospital for monitoring and treatment.
The role of medications: blood thinners and recovery
Anticoagulants (blood thinners) are the main treatment. They don’t dissolve the clot right away. They prevent growth and stop new clots so your body can safely absorb the clot over time.
Most people take blood thinners for at least 3 months. If your clot was unprovoked or you have ongoing risk, your doctor can advise a longer course.
Common options include warfarin (with INR blood tests) and newer direct oral anticoagulants like apixaban or rivaroxaban that usually don’t need routine lab checks.
Blood thinners don’t dissolve the clot but protect you while your body gradually breaks it down.
At-home recovery: rest, activity, and daily habits
Move a little, regularly. Short walks help blood flow and can lower clot risk. Rest when you’re tired. Build up slowly.
Building up exercise safely
Your doctor might suggest starting with short walks (for example, 5–10 minutes) and building up as you feel ready. If you notice chest pain, severe breathlessness, or dizziness during activity, stop and contact your doctor. Compression stockings can help if your leg had a DVT or swelling. If stamina or shortness of breath persists, ask your doctor about pulmonary rehab.
Diet and medication interactions
Eat a balanced diet. If you take warfarin, keep your vitamin K intake steady (leafy greens) rather than avoiding them. Limit alcohol. Check with your doctor before starting new supplements or over-the-counter meds.
5 tips for a safe recovery
- Take your medications exactly as prescribed.
- Move a little, regularly.
- Keep vitamin K intake steady if you’re on warfarin.
- Don’t smoke, and plan movement on long trips.
- Keep follow-up appointments and ask about any lingering symptoms.
Short, regular movement and steady routines help you rebuild stamina safely over time.
Preventing another blood clot
Your risk is higher right after a PE, so prevention matters.
- Keep moving: On flights or long drives, get up every 1–2 hours, stretch, and hydrate.
- Stay active: Regular walking or light exercise helps blood flow.
- Quit smoking: Smoking is linked to clot risk and blood vessel damage.
- Manage health conditions: Keep weight, blood pressure, and other conditions under control.
- Plan for high-risk times: Before surgery or bed rest, tell your doctor you’ve had a PE so a prevention plan is in place.
- Hormones: Talk with your doctor about estrogen-containing birth control or hormone therapy if that applies to you.
Regular movement and smart planning reduce your chances of another clot.
Long-term outlook and possible complications
Most people recover fully and do not have permanent lung damage. About 2–4% develop chronic thromboembolic pulmonary hypertension (CTEPH), which causes ongoing shortness of breath. If your breathing is not improving by about 6 months, ask your doctor about evaluation.
If your clot started in the leg (DVT), some people get post-thrombotic syndrome (long-term leg swelling or discomfort). Compression and activity can help.
Most people recover fully, but a small number develop chronic lung vessel pressure (CTEPH) that needs follow-up.
Caring for your mental and emotional recovery
Feeling anxious after a PE is common. You might worry about every ache or breath. Talk with your doctor about these feelings. Counseling, support groups, and simple breathing exercises can help you feel safer as you heal. National organizations like the National Blood Clot Alliance offer education and support.
As your body recovers and time passes, confidence usually returns.
Feeling anxious after a pulmonary embolism is common, and support and time help your confidence return.
When to call the doctor during recovery
- ⚠️ Call 911: Sudden shortness of breath, sharp chest pain, coughing up blood, fainting, or a racing heartbeat with dizziness.
- ⚠️ Call your doctor promptly: New one-sided leg swelling, warmth, redness, or pain (possible DVT); unusual bleeding (black stools, blood in urine, big bruises); headaches after a fall while on blood thinners.
- Follow up if symptoms persist: If breathing or stamina isn’t improving over months, ask about further evaluation.
If you’re worried, get help—better safe than sorry.
⚠️ Sudden shortness of breath, chest pain, coughing blood, or fainting are emergencies—call 911.
Safety note and tools that can help
- Medication safety: Take blood thinners exactly as prescribed and ask before adding new meds or supplements. Talk to your doctor before trying a new medication.
- Breathing support: If you also manage asthma or COPD, using your inhaled medicines on schedule can help you stay active while you recover. A portable nebulizer can make at-home treatments easier when your routine is off. Use only if your doctor recommends inhaled therapy.
- Travel timing: Ask your doctor when it’s safe to fly; doctors typically advise waiting 2–4 weeks, then take movement and hydration steps during trips.
Your care plan comes first. These tools support, not replace, your doctor’s advice.
Use supportive tools—like a portable nebulizer for other lung conditions—only as part of your doctor’s plan.
Frequently Asked Questions
Tap or click a question below to see the answer:
The body usually absorbs the clot over several weeks to a few months, even though you can feel better much sooner.
Yes. Most people recover fully in weeks to months with proper treatment. A small group needs extra follow-up for lingering issues like CTEPH.
Doctors typically advise waiting 2–4 weeks once you’re stable on medication. When you do fly, wear compression socks, move regularly, and stay hydrated.
No. Blood thinners prevent growth and stop new clots while your body breaks the clot down.
Desk work is sometimes possible within 1–2 weeks once you’re stable on medication. Physically demanding jobs usually take longer; your doctor will tailor timing to your condition.
Keep vitamin K intake steady (leafy greens). Avoid binge alcohol and check with your doctor before new supplements.
Mild soreness can happen during healing, but new or severe chest pain isn’t normal—get urgent medical care.