On this page
Why Is My Throat Mucus Black? Top Causes of Black Phlegm
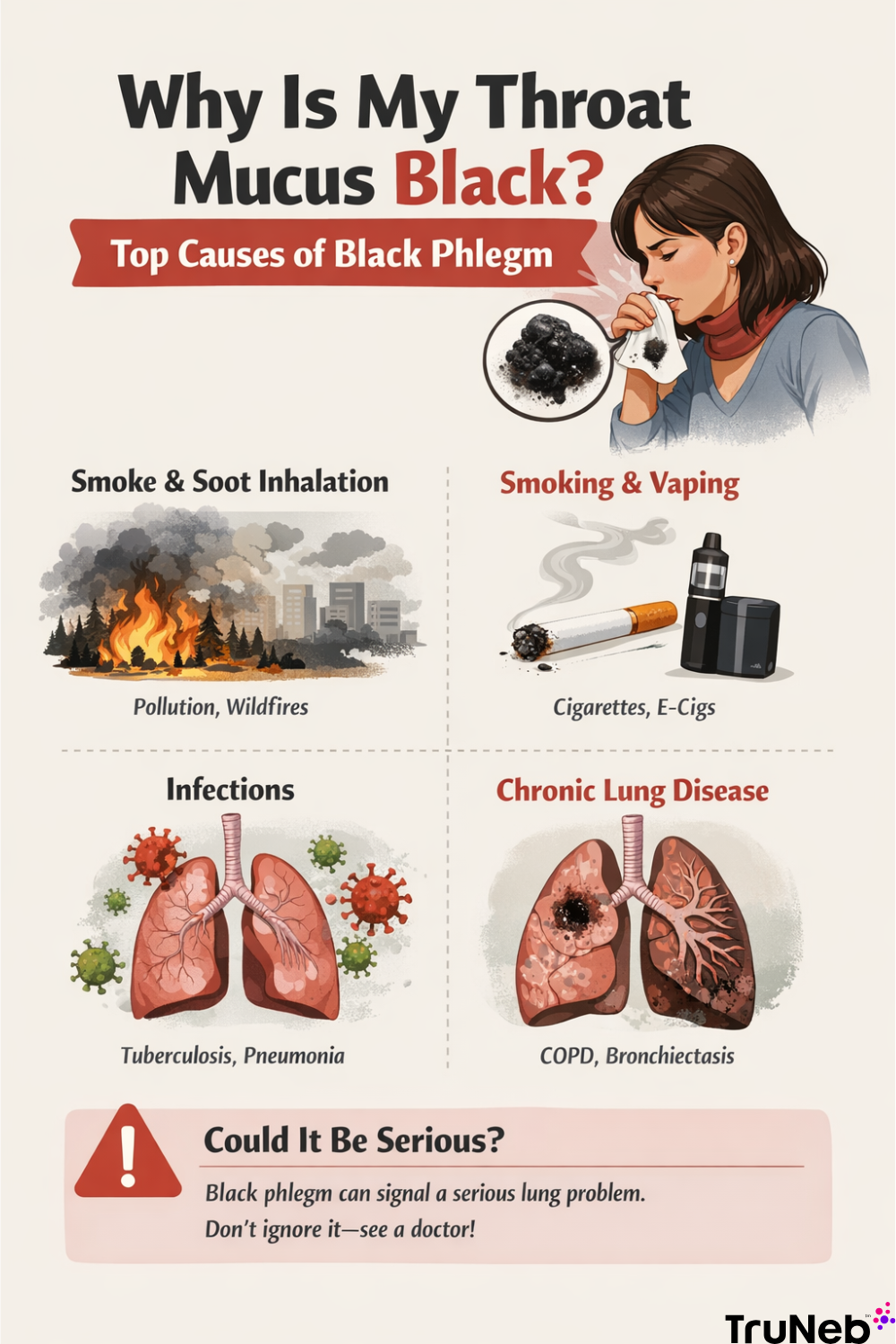
Black mucus from your throat is not normal. The dark color usually means something extra has mixed into your mucus - often soot from smoke, tar from cigarettes, or old blood. In medical terms, coughing up black mucus is sometimes called melanoptysis.
Quick overview of common causes:
- Inhaling smoke or soot (wildfires, heavy pollution, dusty jobs)
- Smoking or vaping (tar and carbon particles)
- Infections (tuberculosis, pneumonia) and some fungal illnesses
- Chronic lung disease with old blood or debris (for example, COPD or bronchiectasis)
- Less often, lung cancer that causes bleeding into the airways
Think of your lungs like air filters. When the air is dirty, the “filter” (your mucus) traps that dirt, and it can look gray or black. Because some causes are serious, black phlegm is something you shouldn’t ignore.
Phlegm vs. mucus: mucus lines your nose and throat; phlegm is the thicker mucus you cough up from your lungs. You might also see black mucus when blowing your nose after smoke or dust exposure, but this article focuses mainly on mucus you cough up from your chest.
Key point: Black phlegm means particles like soot or old blood have stained your mucus - and it deserves a doctor’s look.
Inhaling Smoke or Soot: Environmental Causes of Black Mucus
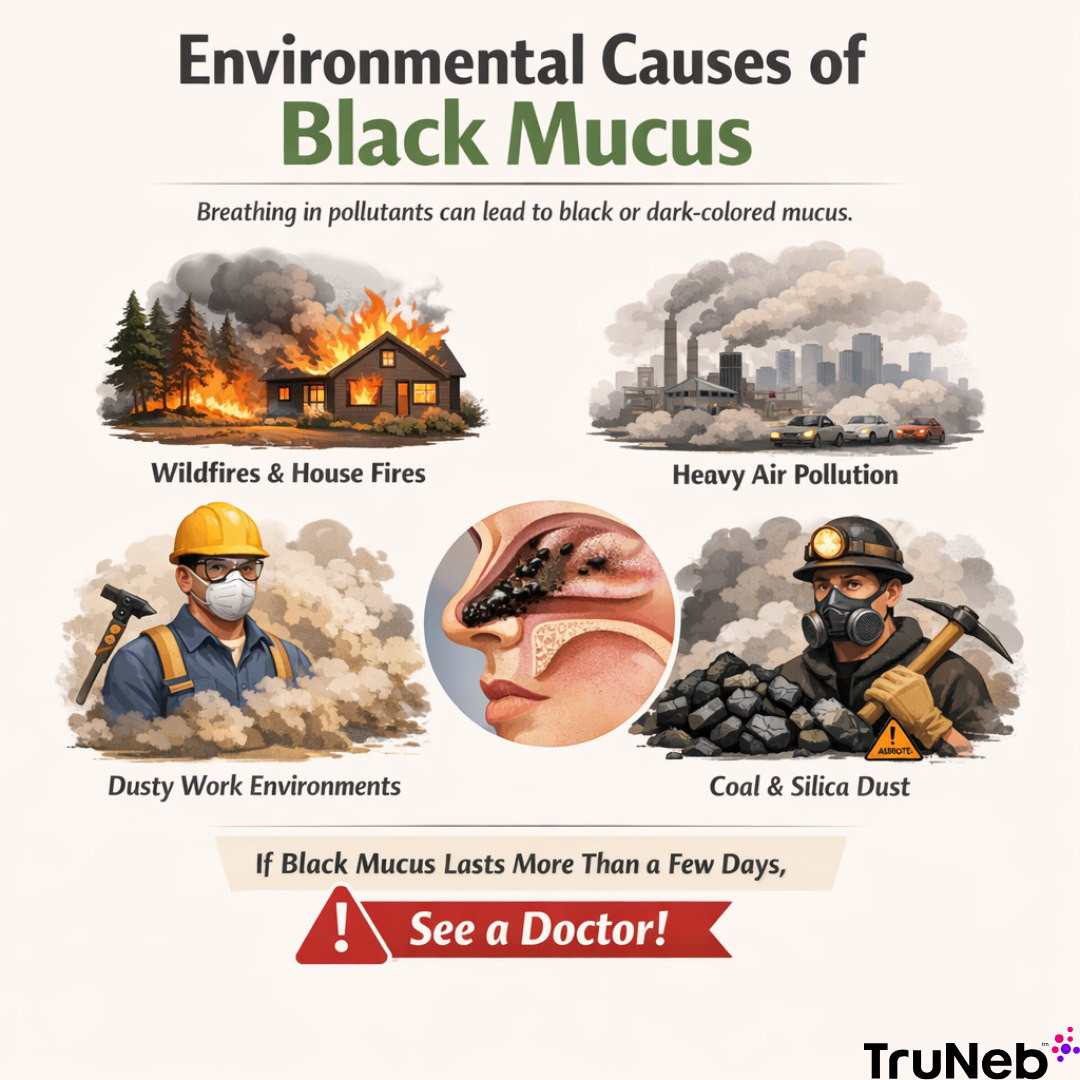
Breathing a lot of smoke or dust can turn your mucus black. Your airways trap soot, ash, and tiny particles and move them out in phlegm. After wildfires, a house fire, or a week of thick smog, it’s common to see gray or black streaks for a short time. If black mucus continues for more than a couple of days after you’re back in clean air, that’s not just a temporary soot effect and needs a doctor’s evaluation.
Common exposures:
- Wildfire smoke, campfire smoke, or indoor fires
- Heavy air pollution or dust storms
- Workplace dust (construction, mining, cutting stone)
- Coal, silica, or asbestos dust
“Black Lung” and Heavy Workplace Dust
“Black lung” (coal worker’s pneumoconiosis) is an extreme example after years of coal dust exposure. It shows how long-term dust can darken lung tissue and mucus over time. Even if you’re not a miner, a dusty day can leave visible black specks in your phlegm.
If symptoms don’t settle after you leave the exposure - or you have chest pain, fever, or trouble breathing - see a doctor.
Key point: Breathing smoke or dust can temporarily turn mucus black as your airways trap soot.
Smoking or Vaping: How Tar Turns Phlegm Dark
Cigarette smoke carries tar and tiny carbon particles. Those particles stick to airway mucus and can stain it brown or black. Long-term smokers can notice a “smoker’s cough” with dark phlegm, especially in the morning. Even secondhand smoke can leave residue your lungs try to clear in mucus.
Smoke also harms the cilia - tiny hairs that sweep mucus out of your lungs. When cilia slow down, mucus builds up and can look darker and thicker.
What about vaping? E‑cig aerosols don’t contain tar like cigarettes, but inhaling heated oils or additives can still leave residue. And smoking anything that burns (including marijuana or hookah) introduces sooty particles that can darken mucus. Dark or black phlegm from smoking typically builds up over months or years of exposure, not just one cigarette.
If you’re seeing black phlegm and you smoke, talk with your doctor about a quit plan and lung check. Many people notice mucus color improves over time after quitting.
Key point: Tar and carbon from smoke collect in mucus, making it brown or black.
Infections That Can Cause Dark or Black Phlegm
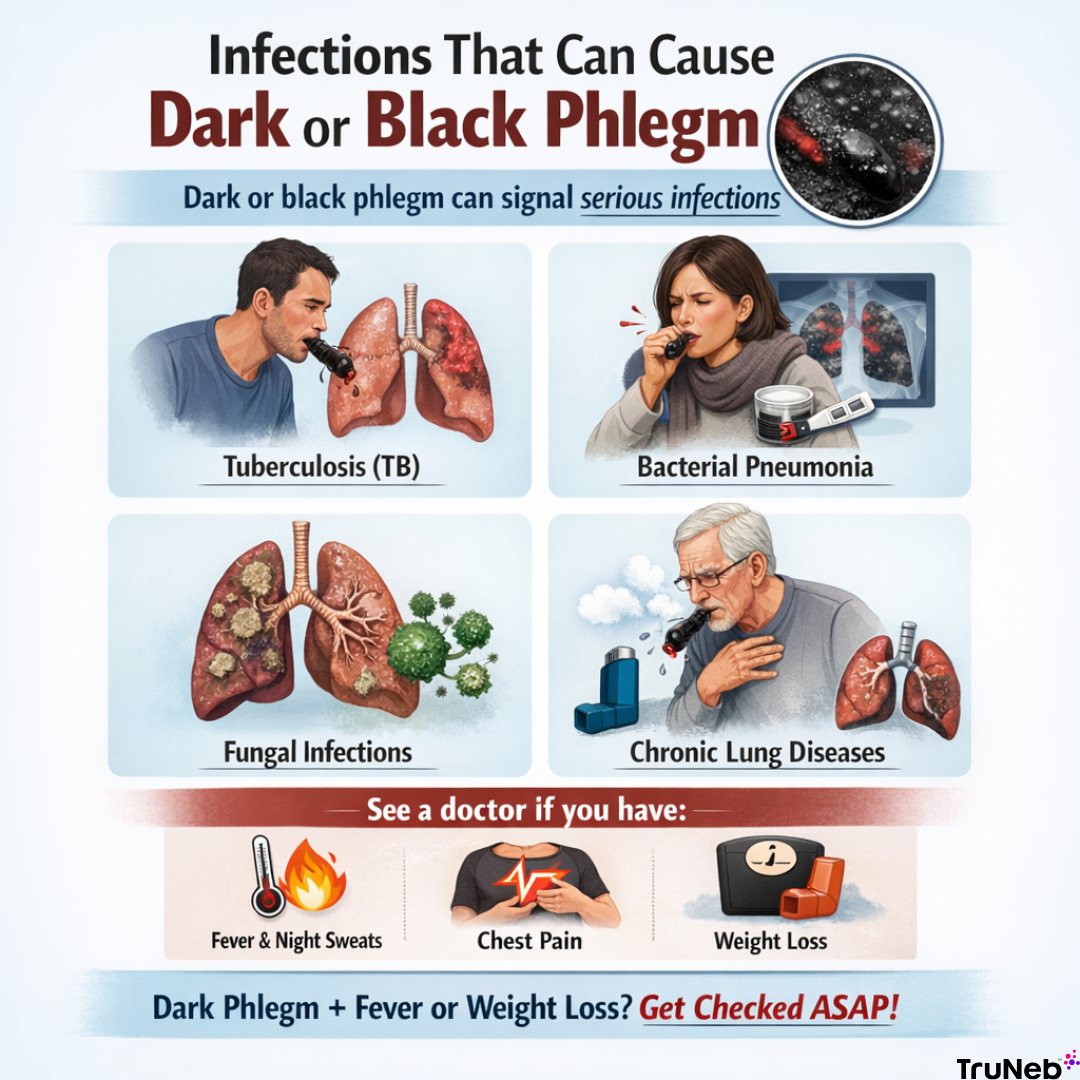
Some infections can make phlegm look dark - usually from bleeding or dead tissue mixing into mucus. Most chest infections cause yellow or green mucus; truly black phlegm is less common and suggests more severe disease or blood and debris mixing into mucus.
Tuberculosis (TB): A serious lung infection that can cause a chronic cough, night sweats, weight loss, and dark or blood-streaked sputum. TB needs prompt testing and treatment.
Bacterial pneumonia: Most pneumonia causes yellow or green phlegm. In tougher cases, old blood can tint sputum brown or very dark.
Fungal infections (like aspergillosis): More common in people with weak immune systems, these can create thick, sometimes brown‑black mucus.
Chronic lung problems (such as bronchiectasis, COPD, chronic bronchitis, or a lung abscess): Trapped mucus and recurring infection can lead to foul-smelling, discolored sputum that can look very dark.
If dark phlegm appears with fever, chest pain, night sweats, or weight loss, seek care quickly.
Key point: Dark phlegm with fever, night sweats, or weight loss needs prompt medical evaluation for serious infections.
Could It Be Cancer? What Black Phlegm Can Mean
Lung cancer itself doesn’t usually make pigment. But it can cause bleeding inside the airways. That blood can dry, turn brown or nearly black, and show up in sputum. This is more concerning if you have risk factors like a long smoking history or a known tumor.
Only a medical exam can tell for sure. Your doctor can order imaging (chest X‑ray or CT) and check the sputum to look for cancer cells. Early detection matters. Black or bloody phlegm alone doesn’t prove you have cancer, but it’s a strong reason to get checked.
If the thought of cancer is on your mind, don’t wait - get checked and get answers.
Key point: Black or bloody phlegm, especially if you smoke or have other risk factors, can be a warning sign of lung cancer and should be checked by a doctor.
Black Specks in Mucus: What Those Tiny Dots Usually Are
Not all black mucus is solid black. Sometimes you’ll see tiny black specks or streaks.
Common explanations:
- Soot or dust you breathed in (after wildfires, a campfire, a dusty attic)
- Small bits of dried blood from irritated airways or a recent nosebleed
Specks that look like grains of dirt are usually soot. Stringy dark streaks can be old blood. You might also see the same black specks when you blow your nose after smoke or dust exposure - this is usually soot, not disease. If black specks keep showing up and there’s no clear exposure, have a doctor take a look.
Key point: Tiny black dots are usually soot or dried blood caught in mucus.
When to Worry and When to See a Doctor
Because black phlegm can signal serious problems, know the next steps.
Call your doctor soon if:
- You have black mucus without a clear smoke or dust exposure
- It lasts more than a day or two, or keeps coming back
- You have a weakened immune system or a known lung condition
⚠️ Go to urgent care, the ER, or call emergency services right away if you have:
- Severe chest pain or trouble breathing
- Coughing up a lot of blood
- High fever, chills, or confusion
- Dark phlegm with night sweats or weight loss (possible TB)
Your doctor can help find the cause and start the right treatment.
⚠️ If you suddenly feel like you can’t catch your breath or you’re coughing up large amounts of blood, don’t wait - seek emergency care immediately.
Key point: If you have black mucus without smoke exposure, see your doctor, and if you also have trouble breathing or cough up a lot of blood, go to the ER.
How to Clear Black Mucus from Your Throat Safely
Relief starts with simple, gentle steps. These help move mucus while you and your doctor sort out the cause.
- Hydrate: Sipping water through the day helps keep mucus thinner. Warm tea or broth can soothe your throat.
- Humidify: A steamy shower or a clean humidifier helps loosen thick mucus.
- Controlled breathing and coughing: Controlled breathing and coughing techniques, such as slow deep breaths followed by a firm cough, can help bring mucus up without straining.
- Fresh air and protection: Leave smoky or dusty areas when you can. Wear a quality mask if you must be in dust or smoke.
- Nebulizer therapy (if your doctor recommends it): A nebulizer turns liquid solution into a fine mist you breathe in. For stubborn, thick mucus, doctors sometimes use saline (including hypertonic saline like 3% or 7%) to draw water into secretions and help clear them, typically in people with ongoing lung conditions like COPD or bronchiectasis. These treatments should only be used with a doctor’s prescription and guidance. A portable mesh nebulizer like TruNeb™ can deliver these saline treatments at home or while you’re out, under your doctor’s guidance.
Always let a doctor figure out why your mucus is black - home steps can help, but they don’t replace a diagnosis.
Simple measures help thin and move mucus; doctor‑directed therapies are for diagnosed lung conditions and don’t replace treatment.
| Option | What it does | Best for | Doctor needed? |
|---|---|---|---|
| Hydration | Thins mucus so it moves more easily | Most people with thick phlegm | No |
| Humidified air | Moistens airways to loosen secretions | Dry environments, irritated throat | No |
| Breathing & coughing techniques | Helps bring mucus up without straining | Chest congestion | No (ask your doctor if you have heart/lung disease) |
| Nebulized normal saline | Adds moisture to airways | Thick secretions | Yes, if prescribed |
| Nebulized hypertonic saline (3% or 7%) | Draws water into secretions to aid clearance | Chronic lung disease (e.g., COPD, bronchiectasis) | Yes, prescription and supervision |
Note: Nebulized saline, especially hypertonic solutions, should only be used if prescribed and supervised by your doctor.
These steps support your lungs but don’t replace treating the root cause.
Safety note: Talk to your doctor before trying a new medication or saline strength.
Key point: Moist air, fluids, and doctor‑guided therapies help your lungs move out dark mucus.
Frequently Asked Questions
Tap or click a question below to see the answer:
Not always. Antibiotics only help when a bacterial infection is causing the dark phlegm. If the color comes from smoke, soot, or old blood, antibiotics won’t fix it. See your doctor to find the cause first.
Pneumonia phlegm is usually yellow or green. In some severe cases it can be brown or blood‑streaked, which can look dark. Pure black mucus is more often linked to smoke or soot exposure or certain fungal infections.
Allergies usually cause clear or white mucus. Black mucus almost always means inhaled particles like soot or blood are mixing into your mucus and should be checked by a doctor.
Key point: Antibiotics only help black phlegm if a bacterial infection is the cause.
Takeaways: Don’t Ignore Black Mucus
- Black mucus is uncommon and usually means soot, smoke, or blood has mixed into your phlegm.
- It can signal serious problems like infection or, less commonly, cancer - so it always deserves a doctor’s attention.
- Simple steps like fluids, humid air, and doctor‑guided therapies (including nebulized saline) support your lungs but don’t replace treatment. If your doctor recommends inhaled saline, a portable nebulizer such as TruNeb can make treatments easier to fit into your day.
Key point: Black mucus is uncommon and is a warning sign - usually from smoke or serious lung problems - so it always needs a doctor’s attention.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms and before starting or changing any treatment.