On this page
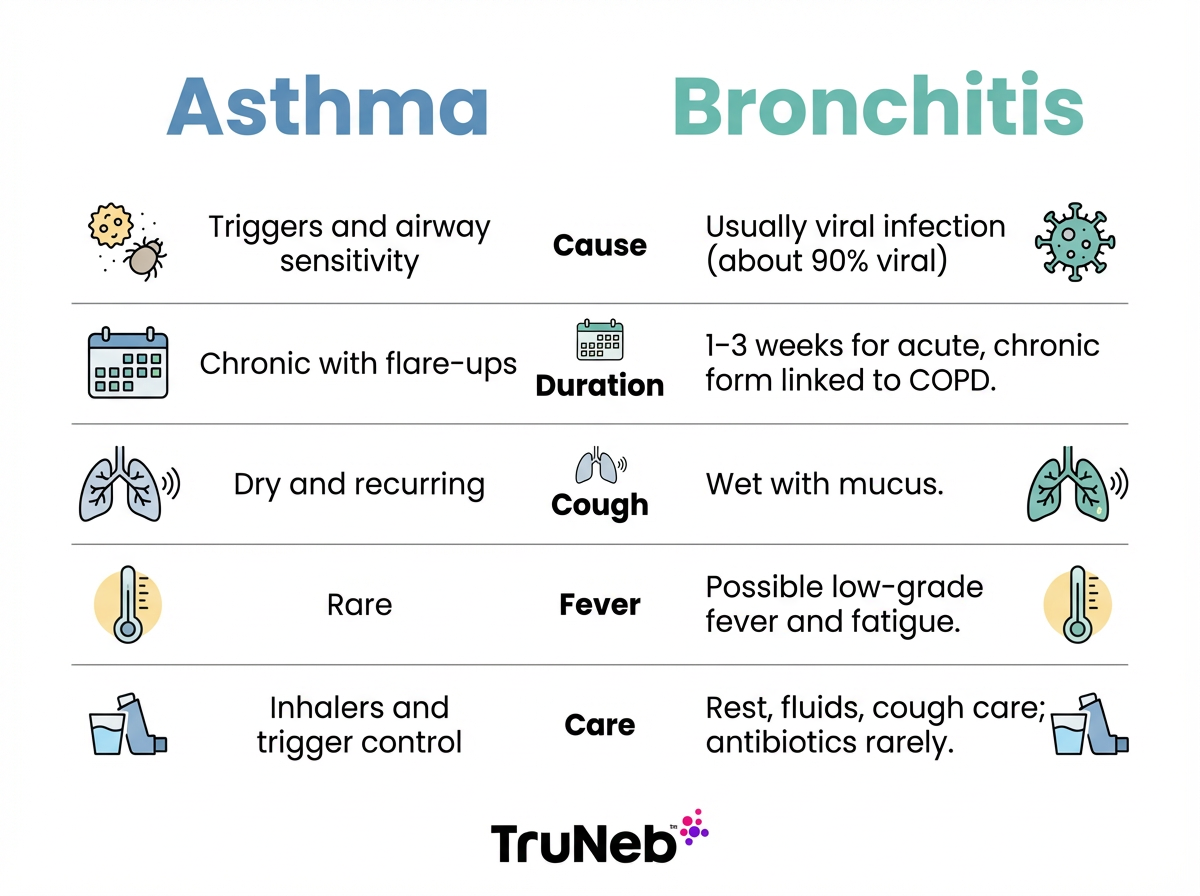
Asthma vs Bronchitis: Key Differences at a Glance
Here’s the main difference between asthma and bronchitis in everyday terms: Asthma is a long-term airway condition that flares with triggers. Acute bronchitis is usually a short-term airway infection that brings a heavy, wet cough.
Quick differences:
- Cause: Asthma is driven by airway sensitivity and triggers. Bronchitis is usually caused by a virus.
- Duration: Asthma is chronic with flare-ups. Acute bronchitis usually clears in 1–3 weeks. Chronic bronchitis is long-term and tied to COPD.
- Cough: Asthma typically causes a dry, recurring cough. Bronchitis usually causes a wet, mucus-filled cough.
- Triggers vs infection: Asthma flares with allergens, smoke, cold air, or exercise. Bronchitis often starts after a cold or the flu.
- Infection vs non-infection: Asthma isn’t an infection; acute bronchitis usually is.
- Fever: Asthma doesn’t typically cause fever. Bronchitis can bring mild fever and fatigue.
Key takeaway: Asthma is a chronic, noninfectious airway disease; acute bronchitis is usually a short-term viral infection with mucus.
| What to compare | Asthma | Acute bronchitis | Chronic bronchitis |
|---|---|---|---|
| Cause | Airway sensitivity and inflammation triggered by allergens, smoke, cold air, exercise | Usually viral infection after a cold or flu | Long-term airway damage, mainly from smoking; part of COPD |
| Cough | Dry or scant clear mucus, comes and goes | Wet, thick mucus (clear/yellow/green) | Daily wet cough for months |
| Duration | Lifelong, with flares | 1–3 weeks | Long-term, recurring |
| Fever | Uncommon | Low-grade fever and fatigue possible | No fever unless another illness |
| Contagious | No | Yes, while sick if viral | No |
| Main care | Controller + rescue inhalers, trigger control | Rest, fluids, cough support; bronchodilator only if wheezy | Smoking cessation, inhaler therapy, regular follow-up |
Takeaway: Asthma is chronic and noncontagious; acute bronchitis is usually a short-term viral airway infection with mucus.
Symptoms: How Asthma and Bronchitis Feel
It’s easy to mix these up because they share a lot of symptoms: cough, wheeze, chest tightness, and shortness of breath.
Asthma patterns
- Cough is usually dry and comes in episodes.
- It’s typically only a small amount of clear mucus, unlike the thick mucus of bronchitis.
- Wheeze is common, especially on exhale.
- Symptoms often worsen at night, early morning, with exercise, cold air, smoke, or allergens.
- You can feel normal between flares.
Bronchitis signs
- Cough is usually wet with thick mucus (clear, yellow, or green).
- Bronchitis can cause wheezing that sounds like asthma, which is one reason they’re easy to confuse.
- Low fever, fatigue, and chest discomfort are common during the illness.
- In chronic bronchitis, a daily mucus cough lasts for months and can bring wheeze and breathlessness on exertion.
Only a doctor can tell for sure, but these patterns give you a sense of what they’ll look for.
Takeaway: A dry, trigger-based cough points to asthma; a wet, post-cold cough with mucus points to bronchitis.
Causes and Triggers: What Starts Each Condition
Asthma causes and triggers
- Asthma develops from a mix of genetics and environment.
- Common triggers: pollen, dust mites, pet dander, mold, smoke, pollution, cold air, and exercise.
- Asthma is not contagious.
Bronchitis causes
- Acute bronchitis is usually viral. About 90% of cases are linked to viruses from colds or flu.
- Because viruses cause most acute bronchitis, it’s contagious while you’re sick.
- Chronic bronchitis is mainly due to long-term smoking and is part of COPD. Air pollution and job-related fumes or dust also raise risk.
Can one turn into the other? No. Asthma doesn’t turn into bronchitis, and bronchitis doesn’t turn into asthma. They can happen in the same person, and an infection can trigger an asthma flare. When someone with asthma gets bronchitis, some doctors call it “asthmatic bronchitis” (you’re dealing with both asthma and an infection at once, not a new disease).
Takeaway: Asthma stems from airway sensitivity and triggers; acute bronchitis is usually a short-term viral infection.
Diagnosis: How Doctors Tell Them Apart
Your doctor starts with your story and a lung exam.
What doctors use:
- Spirometry: you blow into a device to measure airflow. In asthma, airflow usually improves after a bronchodilator.
- Pattern matters: a cough that goes away but keeps returning points toward asthma.
- Chest X-ray: sometimes ordered to rule out pneumonia if bronchitis is suspected.
- Acute bronchitis is usually diagnosed by recent illness, a wet cough, and exam findings.
Clues doctors use:
- Recurring, trigger-based symptoms over time point to asthma.
- Clear improvement after a bronchodilator supports asthma.
- A one-time wet cough after a cold points to acute bronchitis.
Takeaway: Reversible airflow limits and recurring episodes suggest asthma; a one-time wet cough after a cold suggests bronchitis.
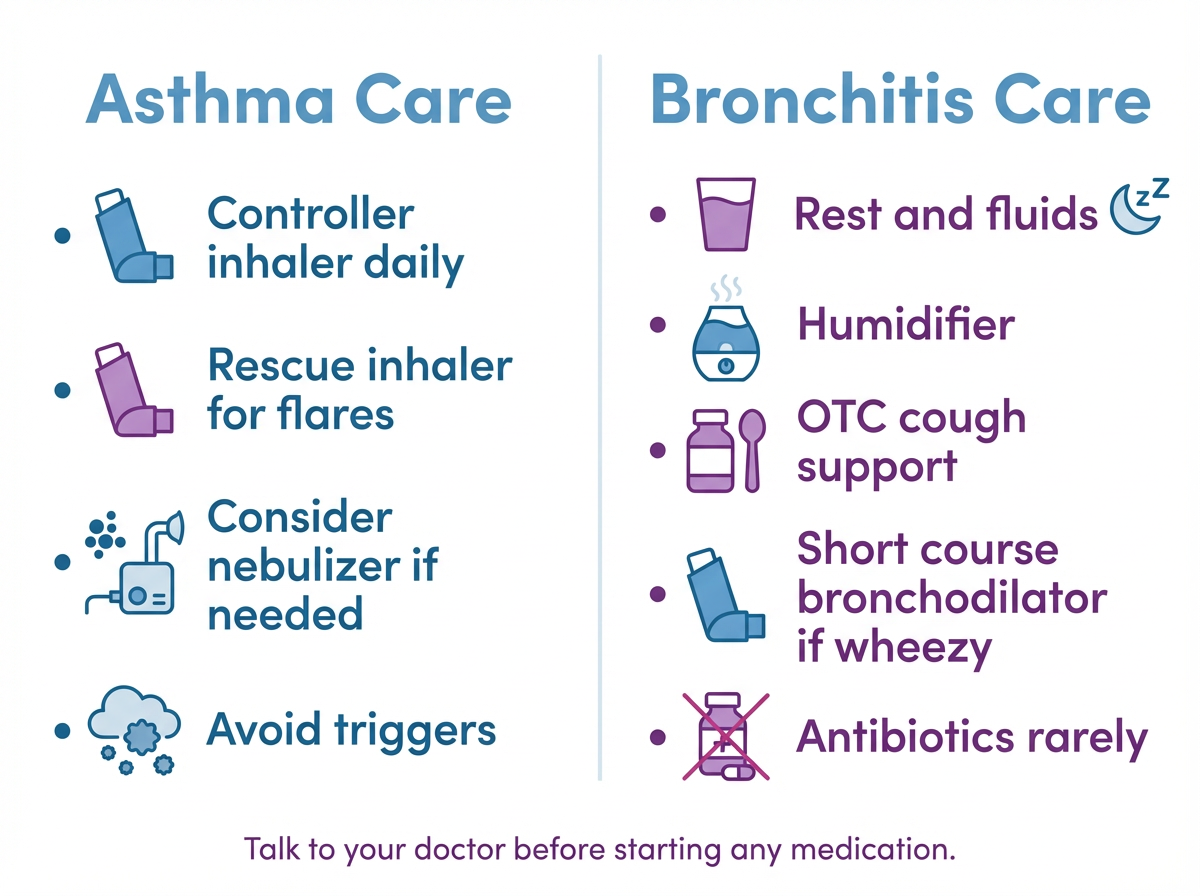
Treatment and Management: What Helps and When
Asthma care
- Daily control: many people use inhaled corticosteroids or combination inhalers to calm airway swelling.
- Quick relief: a rescue bronchodilator helps during flares.
- Delivery: inhalers are standard. A portable nebulizer can help if you struggle with inhalers during a flare or for young children. The TruNeb™ Portable Mesh Nebulizer is a quiet, travel friendly option some patients use under a doctor’s guidance.
- Trigger control: avoid smoke, allergens, and cold-air exposures when possible.
Bronchitis care
- Acute bronchitis typically follows a cold or flu. Most people do best with rest, fluids, humidified air, and over-the-counter cough support.
- If you have wheeze or tightness, your doctor may prescribe a bronchodilator by inhaler or nebulizer for short-term relief.
- Because most acute bronchitis is caused by viruses, antibiotics usually don’t help and aren’t prescribed unless your doctor thinks a bacterial infection is likely.
- Some doctors use nebulized saline to help loosen thick mucus. Ask what’s right for you.
- Ask your doctor which cough medicines or inhalers are safe for you, especially if you have other health conditions.
- ⚠️ If you see products labeled “steam inhaler,” don’t use them to take prescription nebulizer medicines because they’re not designed to deliver medication into your lungs.
Safety note: Talk to your doctor before trying a new medication, changing doses, or using hypertonic saline.
Asthma doesn’t have a cure, but treatment keeps it controlled; acute bronchitis usually clears on its own.
Takeaway: Asthma needs long-term control plus rescue medicine; acute bronchitis is usually supportive care, with bronchodilators only if breathing is tight.
Prevention and Outlook: What to Expect Long Term
Preventing asthma flares
- Avoid cigarette smoke and known triggers.
- Keep indoor allergens down and follow your written action plan.
Preventing bronchitis
- Wash hands, avoid sick contacts, and don’t smoke.
- Use masks or ventilation if you work around fumes or dust.
- Ask your doctor about flu and pneumonia vaccines if you have asthma or chronic lung disease, since infections can hit your lungs harder.
Outlook
- Asthma is lifelong but very manageable. With the right plan, most people stay active and well.
- Acute bronchitis is temporary and usually resolves in 1–3 weeks. Chronic bronchitis needs ongoing care with your doctor and is tied to COPD, but quitting smoking helps.
Takeaway: Asthma is controlled with good daily management; acute bronchitis usually clears with time and rest.
When to Seek Medical Help Right Away
⚠️ Call for emergency help if:
- Breathing is very hard, you can’t speak in full sentences, or lips look blue.
- Your rescue inhaler isn’t helping.
- You feel confused or too exhausted to breathe well.
See a doctor soon if:
- You have a high fever or a fever that lasts more than 3 days.
- You’re short of breath at rest or wheezing a lot.
- You have chest pain or cough up blood.
- Your cough hasn’t improved after 2–3 weeks.
These more severe symptoms can sometimes point to pneumonia or another serious lung problem, not just simple bronchitis.
If you’re unsure and breathing is difficult, it’s safer to get care now.
Takeaway: If breathing is hard and not improving, seek medical care immediately.
Frequently Asked Questions
These quick answers clear up common questions about how asthma and bronchitis differ, overlap, and when to get help.
Asthma cough is usually dry, comes and goes with triggers like allergens, exercise, or cold air, and you can feel normal between flares. Bronchitis cough is wet with thick mucus and typically follows a cold or flu. A doctor can confirm with an exam and tests like spirometry.
Yes. Asthma and bronchitis are different conditions, and you can have both — especially if a respiratory infection triggers an asthma flare. Treatment then targets the infection and your asthma control at the same time. See your doctor if your breathing is getting worse.
It’s a practical label some doctors use when a person with asthma also has bronchitis. It means you’re dealing with an infection plus asthma symptoms, not a new disease. Care focuses on both: asthma medicines for airflow and supportive care while the infection clears.
Asthma isn’t contagious. Acute bronchitis is usually caused by viruses that can spread to others while you’re sick. Chronic bronchitis from smoking isn’t contagious.
Not usually. Most acute bronchitis care is rest, fluids, and cough support. If you’re wheezing or very tight, a doctor may prescribe a short course of a bronchodilator by inhaler or nebulizer.
Both can be serious. Uncontrolled asthma can cause dangerous attacks and needs ongoing management. Acute bronchitis is usually mild in healthy people and clears in 1–3 weeks, while chronic bronchitis is a long-term COPD condition that needs regular follow-up with a doctor.
In kids, both can show as cough and wheeze after colds. Asthma typically shows up as nighttime or exercise-related cough and wheeze, while acute bronchitis brings a wet, mucus cough for 1–3 weeks. Because the signs overlap, a pediatrician should make the diagnosis and guide treatment.
Disclaimer: This article is for informational purposes only and isn’t a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms and any questions about medications or devices.