On this page
Asthma Treatment Equipment Overview
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms, asthma action plan, and any treatments or equipment you use.
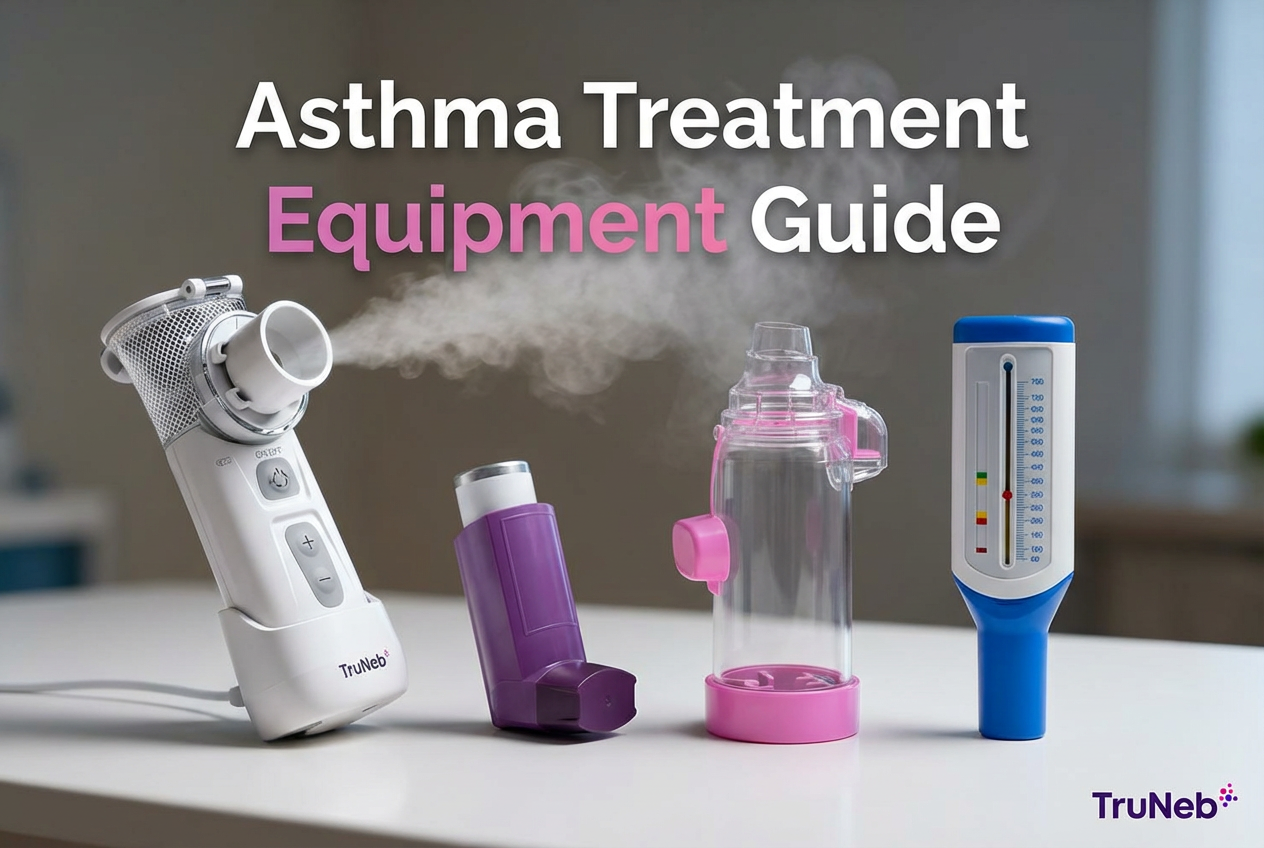
Asthma treatment equipment helps you get medicine straight into your lungs and track how well you’re breathing. These are the main types of asthma treatment equipment doctors use today. The main tools are:
- Inhalers: small handheld devices that deliver quick‑relief (rescue) or daily controller medicine.
- Nebulizers: machines that turn liquid medicine into a fine mist you breathe normally.
- Spacers: add‑ons for metered‑dose inhalers that make each puff easier to inhale.
- Peak flow meters: simple monitors that measure how fast you can blow air out.
That includes asthma spacers and peak flow meters alongside inhalers and nebulizers.
Inhaled treatments are typically first‑line because they act quickly in the airways and tend to cause fewer whole‑body side effects than pills. Your doctor’s asthma action plan tells you when to use each device and what dose to take.
A typical asthma plan might include carrying a rescue inhaler for sudden symptoms, using a controller inhaler daily, keeping a nebulizer at home for tough flare‑ups, and checking a morning peak flow to spot early changes—always based on your doctor’s plan.
⚠️ If you have severe trouble breathing, trouble speaking in full sentences, bluish lips or face, or your usual rescue medicine doesn’t help, seek emergency medical care right away.
In short: Inhalers, nebulizers, spacers, and peak flow meters are the core tools to treat and track asthma.
Types of Asthma Inhalers and How They Work
Here are the main types of asthma treatment devices and how they work.
Metered‑Dose Inhalers (MDIs)
MDIs are the classic “puffer” with a pressurized canister that delivers a measured puff. They work fast and are very portable. Good technique matters, so a lot of people use a spacer (valved holding chamber) to make each puff easier to inhale. MDIs can deliver quick‑relief bronchodilators like albuterol and some daily controller medicines.
Dry Powder Inhalers (DPIs)
DPIs deliver medicine as a powder you pull in with a quick, deep breath. There’s no spray to time, but you do need enough inhalation strength, so DPIs are best for older kids and adults. Some DPIs deliver inhaled corticosteroids such as budesonide.
Soft Mist and Breath‑Actuated Inhalers
These newer devices release a slow‑moving mist or automatically release a dose when you begin to inhale. They can make coordination easier for some people.
Inhaler Use Tips
- Using an MDI typically involves shaking it, breathing out first, then pressing and inhaling slowly and deeply, and holding your breath for about 10 seconds. Your doctor or nurse will show you the exact steps.
- People are usually advised to rinse their mouth after using steroid inhalers to lower the risk of thrush.
- Check dose counters and keep caps clean. For a lot of people, pairing an MDI with a spacer is the easiest way to get medicine into the lungs.
In short: Choose the inhaler type that fits how you breathe, and pair MDIs with a spacer to help more medicine reach your lungs.
Inhaler vs Nebulizer: Which One and When
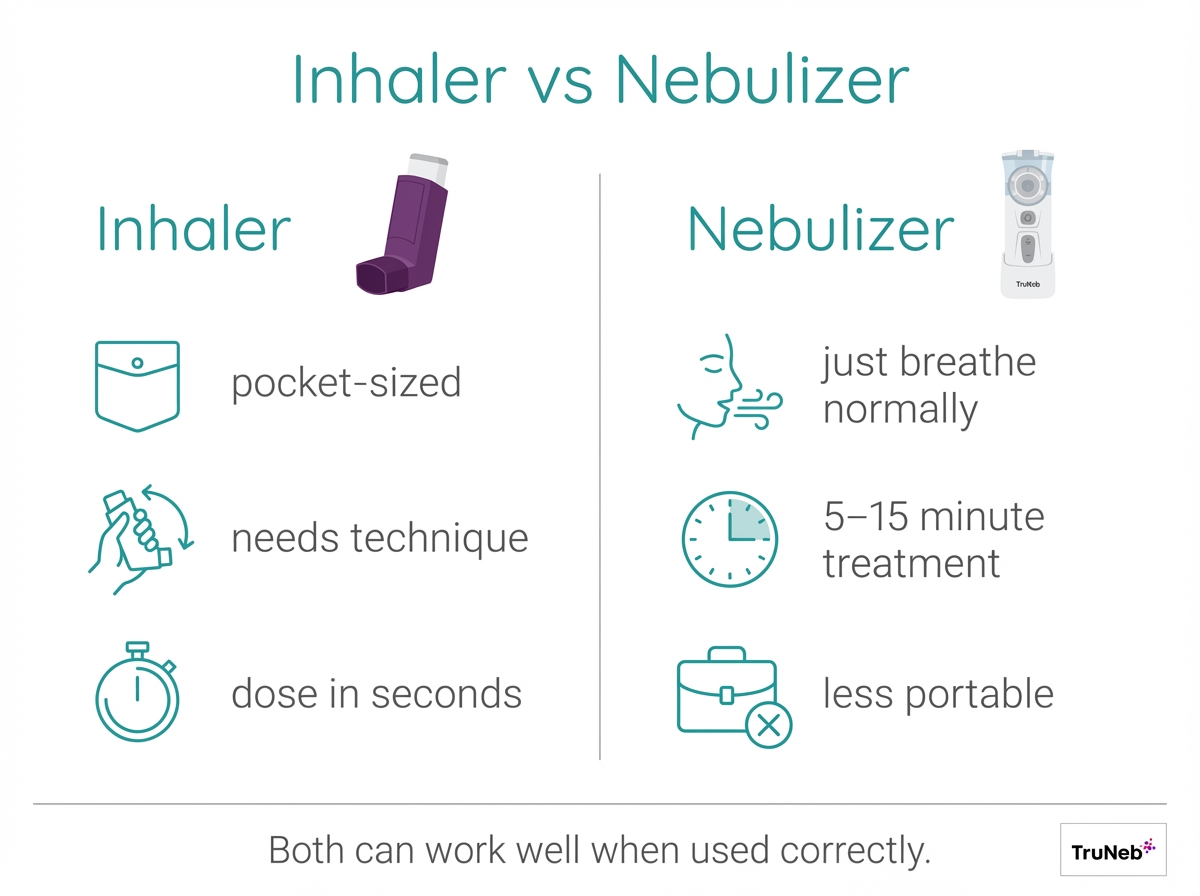
Both deliver the same kinds of asthma medicines; they differ in how you take them.
Here’s a quick asthma inhalers vs nebulizers comparison:
- Portability: Inhalers fit in a pocket. Nebulizers are usually tabletop units, though newer portable mesh models are small and travel‑friendly.
- Ease of use: Inhalers work in seconds but require timing and technique. Nebulizers are easy to use. You just breathe normally through a mouthpiece or mask.
- Speed: An inhaler dose takes seconds. A nebulizer treatment usually takes about 5–15 minutes.
- Effectiveness: When used correctly, an MDI with a spacer can work as well as a nebulizer for common bronchodilators. Technique is the key.
- When to use: Inhalers are first choice for most daily and on‑the‑go needs. Doctors typically recommend a nebulizer when someone can’t use an inhaler well (for example, infants or severe flare‑ups) or for specific medicines.
A nebulizer treatment isn’t automatically “stronger” than an inhaler dose; the difference is mostly how the medicine is delivered and how easy it is for you to use the device correctly.
Follow your asthma action plan to know which device to use in each situation.
In short: Inhalers are fast and portable; nebulizers are simple to breathe but take longer—both work when used correctly.
Nebulizer Machines for Asthma: Home and Portable
What a nebulizer does: It turns liquid medicine into a fine mist you breathe in through a mouthpiece or mask. People sometimes call this a “breathing treatment.” A typical treatment lasts about 5–15 minutes while you sit and breathe normally.
Who benefits: Nebulizers are helpful for young children, older adults, and anyone who struggles to use an inhaler during a flare. Some medicines are also designed for nebulizer use (for example, a bronchodilator like albuterol or an inhaled corticosteroid like budesonide). Portable asthma treatment devices for adults and kids, like mesh nebulizers, can help when a doctor prescribes one.
Types of nebulizers:
- Jet (compressor) nebulizer: Plug‑in, reliable, and affordable for home use, but larger and louder.
- Mesh nebulizer: Handheld, quiet, and battery‑powered for quick treatments on the go. For example, a modern portable mesh device is pocket‑sized and nearly silent, useful for on‑the‑go treatments.
- Ultrasonic nebulizer: Handheld units that use high‑frequency vibrations; less common for asthma medicines because they can warm solutions and aren’t compatible with every medication.
When you’re choosing the best home nebulizer for asthma treatment, think about:
- Portability: tabletop vs handheld.
- Power: outlet vs rechargeable.
- Noise and treatment time.
- Medication compatibility and ease of cleaning.
Basic use: A typical treatment involves using the exact dose your doctor prescribed, sitting upright while you breathe in the mist until it stops, then cleaning the cup and mouthpiece or mask as the device instructions describe. Don’t share nebulizer mouthpieces or masks with other people to reduce infection risk. ⚠️ Don’t use a steam inhaler to breathe in asthma medicine—steam devices are not the same as nebulizers and aren’t made for prescription nebulizer solutions.
In short: Mesh nebulizers are quiet and portable, while compressor models are sturdy home units—choose the one that fits how and where you do your treatments.
Using Spacers with Inhalers: Why and How
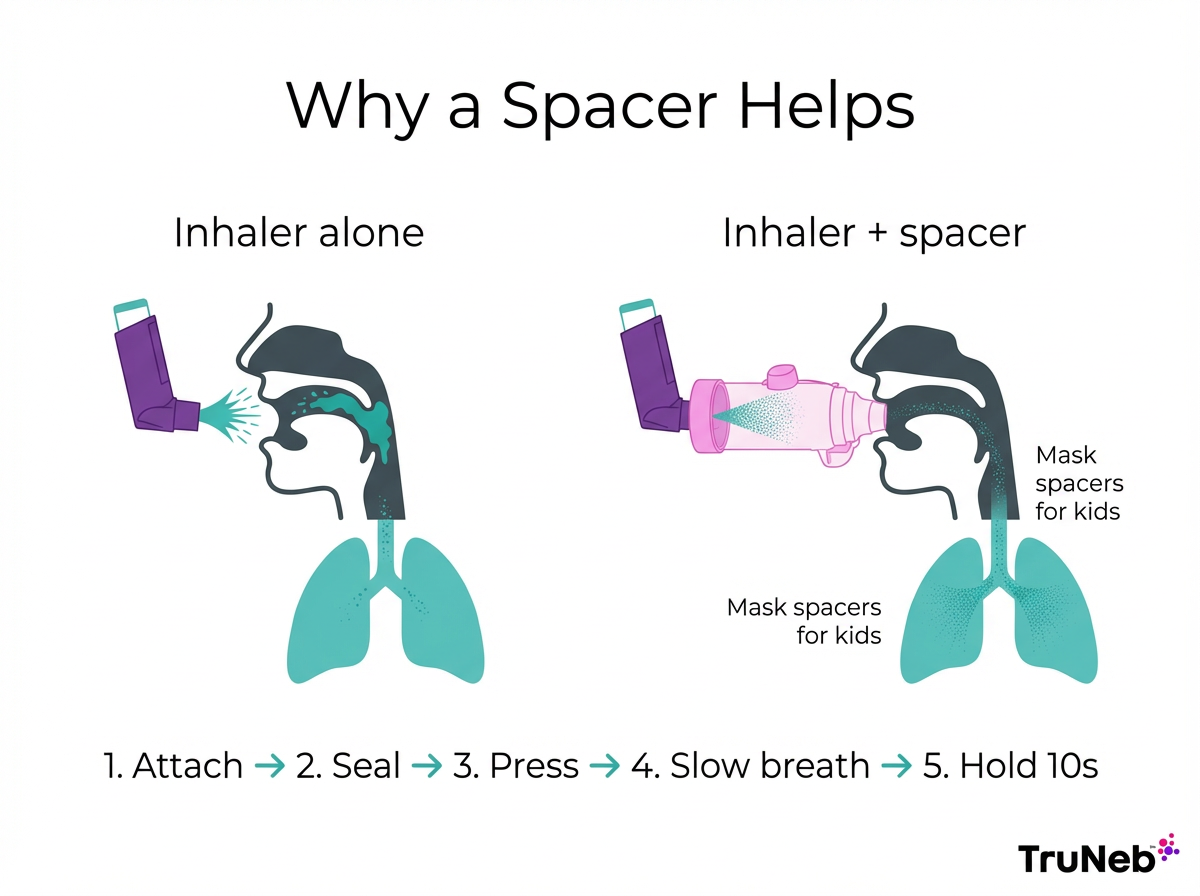
What a spacer is: A spacer (valved holding chamber) is a tube that holds the medicine cloud from an MDI for a moment so you can breathe it in slowly. Mask spacers are available for young children.
Why it helps:
- More medicine reaches the lungs and less sticks in the mouth and throat.
- Easier timing: press the inhaler, then inhale from the spacer without rushing.
- Using a spacer can significantly increase how much medicine actually reaches your lungs compared with using an inhaler alone.
- Fewer side effects with steroid inhalers (lower risk of thrush).
How to use it:
Using a spacer usually involves attaching the inhaler, making a tight seal with your lips (or fitting the mask snugly), pressing one puff into the spacer, and then taking a slow, deep breath and holding it for about 10 seconds. For small kids, a few normal breaths from the spacer is commonly taught. Your doctor or nurse will show you the exact steps.
Care: Wash the spacer with mild soap and water weekly and let it air‑dry to reduce static.
In short: A spacer guides more medicine into your lungs and makes inhaler timing easier.
Monitoring Asthma at Home: Peak Flow Meters
A peak flow meter measures how fast you can blow air out. Think of it like a thermometer for your lungs—it shows how open (or tight) your airways are right now.
Why it’s useful:
- Helps you and your doctor track daily control.
- Can reveal a drop in lung function before you feel symptoms.
- Guides action plan steps (green, yellow, red zones).
How to use it:
Your doctor will show you how to use it, but in general you set the marker to zero, stand up, take a deep breath, seal your lips around the mouthpiece, and blow out as hard and fast as you can. Do this three times and record the highest number. Try to test at the same time each day.
Peak flow meters are most useful for people with moderate to severe asthma or those who’ve had serious flare‑ups. Your doctor will help you set your “personal best” and zones.
In short: A peak flow meter is like a thermometer for your lungs—great for spotting changes early and following your plan.
Saline Nebulization and Mucus Clearance Options
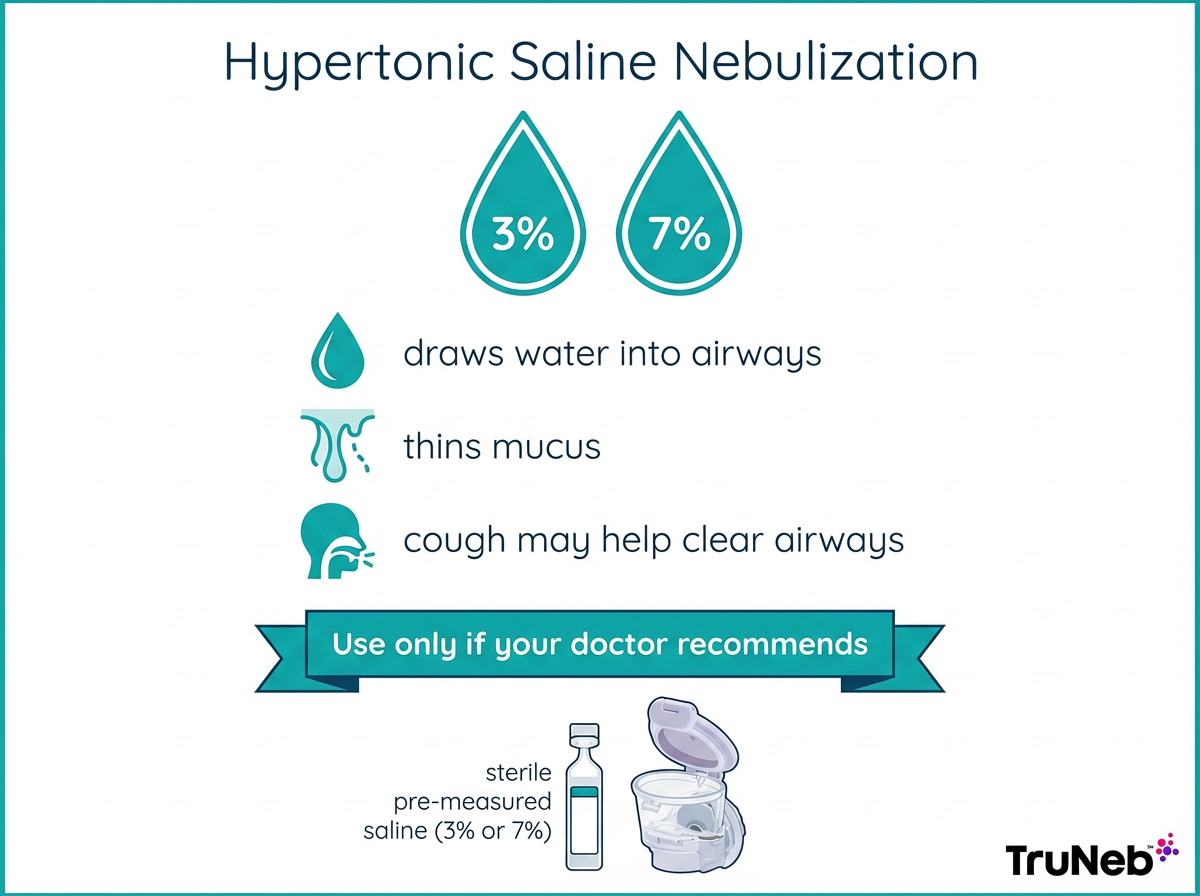
Hypertonic saline (3% or 7%) is a sterile saltwater solution you can nebulize to draw water into the airways and thin thick mucus. It is widely used in cystic fibrosis and bronchiectasis, and some adults with asthma and stubborn mucus can also benefit under specialist guidance. The mist can trigger coughing that helps move mucus up and out. This isn’t a standard treatment for every person with asthma and is usually reserved for certain cases with thick, hard‑to‑clear mucus. It’s not a replacement for your usual controller or rescue medicines.
If your doctor recommends saline therapy, use a sterile, pre‑measured product made for nebulizers. TruNeb™ 3% and 7% hypertonic saline ampules are sterile and pre‑measured, so you don’t have to mix solutions yourself.
Other airway clearance tools, like oscillatory PEP devices (handheld gadgets that vibrate and help loosen mucus) or chest physiotherapy, are sometimes added in certain cases.
⚠️ Never nebulize homemade saltwater or solutions not designed for nebulizers. Talk to your doctor before trying a new medication or saline treatment. Hypertonic saline can cause irritation or bronchospasm (sudden tightening of the airways).
In short: Hypertonic saline can thin sticky mucus, but only use it if your doctor recommends it.
Caring for Your Asthma Equipment and Final Tips
Keep your devices clean and ready:
- Bring your devices to check‑ups so your doctor can review your technique.
- Inhalers: Most instructions recommend wiping mouthpieces. If using an MDI, remove the canister and rinse the plastic actuator weekly, then let it air‑dry fully.
- Spacers: Wash with mild soap and water weekly and air‑dry to reduce static.
- Nebulizers: Device manuals generally advise washing the medicine cup and mouthpiece or mask with warm soapy water after each use, rinsing, and air‑drying. Replace compressor filters as directed.
- Storage: Keep devices dry and away from heat. Check dose counters and expiration dates.
- Spares: Keep backup parts, a spare inhaler, and extra batteries if you use a portable nebulizer.
If you’re using your equipment correctly and still have frequent symptoms, night‑time waking, or activity limits, talk to your doctor about updating your asthma action plan. With the right equipment and habits, plus modern options like portable mesh nebulizers and ready‑to‑use saline ampules (such as those by TruNeb), staying on plan gets simpler.
In short: Clean, store, and check your devices regularly, and review your technique with your doctor.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms, asthma action plan, and any treatments or equipment you use.
Frequently Asked Questions
Tap or click a question below to see the answer:
An inhaler is a small device that gives a quick puff of medicine you breathe in, while a nebulizer turns liquid medicine into a mist you breathe over several minutes. Inhalers are pocket-sized and fast but require good technique. Nebulizers are easier to breathe with during a flare but take longer and are less portable.
Doctors usually recommend a nebulizer when someone can’t use an inhaler well (for example, infants, severe shortness of breath, or limited coordination) or for certain medicines. Your asthma action plan should spell out when to use each device.
Not by default. If used correctly, a metered-dose inhaler with a spacer can deliver bronchodilators as effectively as a nebulizer. The real difference is technique and the situation you’re in, not the strength of the medicine.
In general, wipe inhaler mouthpieces, wash spacers weekly with mild soap and water, and wash and rinse nebulizer parts after each use, then air-dry. Replace compressor filters on the schedule in your manual. See the “Caring for Your Asthma Equipment and Final Tips” section above for the full checklist.
Possibly, but only if your doctor recommends it. Hypertonic saline (3% or 7%) can thin thick mucus but can cause irritation or coughing in some people. Always use sterile, pre-packaged saline made for nebulizers and follow your doctor’s plan.
Most children do well with a metered-dose inhaler plus a spacer and mask, since it makes timing easy and improves delivery. Very young children or kids during bad flares might use a nebulizer. Your pediatrician will guide the choice.







