On this page
Key Differences Between an Asthma Cough and a Cold Cough
Asthma coughs and cold coughs don’t act the same. Here’s how to tell, fast:
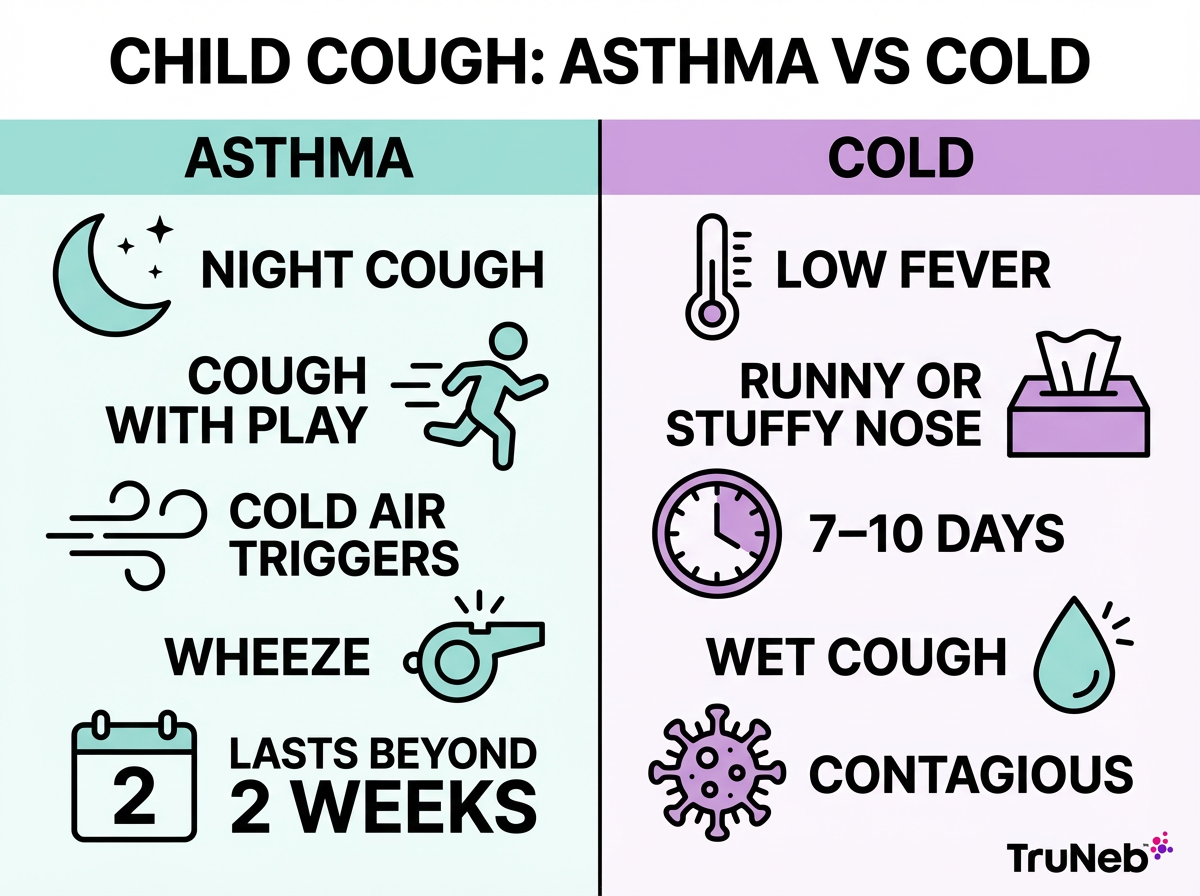
- Duration: An asthma cough usually lingers or keeps coming back. A cold cough fades in about 1–2 weeks.
- Timing: Asthma coughs flare at night, early morning, or with triggers like exercise or cold air. A cold cough is tied to the infection and improves as you recover.
- Cough quality: Asthma is commonly a dry, tickly cough. Colds usually sound wet or phlegmy.
- Other symptoms: Asthma pairs with wheezing, chest tightness, and shortness of breath. Colds usually include runny or stuffy nose, sore throat, sneezing, and sometimes a mild fever—fever and body aches don’t come from asthma itself.
- Triggers vs cause: Asthma is trigger‑based (allergens, smoke, cold air, exercise, viral infections). A cold is a viral infection of the upper airways.
- What brings relief: Asthma coughs usually improve after quick‑relief asthma medicine. Cold coughs ease as the virus runs its course; inhalers don’t usually help if you don’t have asthma.
Asthma isn’t contagious; colds are caused by contagious viruses.
Bottom line: Dry, persistent, trigger‑based cough usually points to asthma; wet, short‑term cough with nasal symptoms usually points to a cold.
Side‑By‑Side Comparison
Asthma cough vs cold or flu cough: quick comparison
| Feature | Asthma cough | Cold or flu cough |
|---|---|---|
| Cause | Reactive, inflamed lower airways | Viral infection of upper airways |
| Duration | Persistent or recurrent | Usually 7–10 days, then resolves |
| Timing | Worse at night, early morning, with exercise or cold air | Follows the illness; improves as the cold fades |
| Cough quality | Usually dry or scant, sticky mucus | Usually wet/productive with phlegm |
| Other symptoms | Wheeze, chest tightness, shortness of breath; typically no fever | Runny/stuffy nose, sore throat, sneezing, mild fever/aches |
| Triggers | Allergens, smoke, cold air, exercise, viruses | Contact with contagious viruses |
| Response to treatment | Improves with inhaled bronchodilators and controller medicines (as prescribed) | Gets better with time and supportive care; inhalers don’t help if no asthma |
| Contagious | No | Yes |
In short, asthma coughs tend to be dry, long‑lasting, and trigger‑based, while cold or flu coughs are usually wet, contagious, and clear up in about a week.
Everyone is different, so a doctor can confirm what’s causing your cough.
Signs It’s Asthma and Not Just a Cold in Adults
Look for patterns, not just one rough day.
- Night signals: Coughing that wakes you or hits early morning.
- Effort triggers: Cough or chest tightness on stairs, during workouts, or when laughing.
- Cold air or strong smells: Symptoms kick up in winter air or around fumes and perfumes.
- The lingering cough: Still coughing 2–3 weeks after a “cold” is a red flag that something more than a simple cold is going on, including asthma.
- Relief clue: If a quick‑relief inhaler eases coughing or tightness, asthma can be involved.
Next step: book an asthma check with your doctor. Simple breathing tests can confirm what’s going on and help you and your doctor build a plan.
Cough‑Variant Asthma and Lingering Coughs
Some people have a form of asthma where the main symptom is a persistent dry cough, with little or no wheeze—especially after a cold or at night. It’s easy to mistake this for “just a cough.” If this sounds like you, talk to your doctor; other causes like reflux or post‑nasal drip can also cause chronic cough, and a proper evaluation can sort it out.
Bottom line: A cough that lingers, worsens at night, and improves with an inhaler strongly suggests asthma and should be checked by a doctor.
Is It Just a Cough or Childhood Asthma
Kids can’t always explain how they feel. Patterns tell the story.
- Nighttime cough: Waking to cough or wheeze is a classic asthma sign.
- During play: Coughing, wheezing, or quick fatigue when running or playing.
- Early morning: Symptoms flare on waking.
- Triggers: Cold air, pets, pollen, or dust make symptoms worse.
- The repeat cold: “Every cold goes to the chest” or coughs that linger after each illness.
- Family history: Asthma, eczema, or allergies raise the odds.
If these patterns show up or the cough lasts more than two weeks, see your pediatrician for an asthma check. Younger children can’t always do formal breathing tests, so doctors rely on patterns and sometimes a trial of asthma medicine to see if symptoms improve. Asthma doesn’t just go away with each cold—look for patterns across illnesses.
Bottom line: Night and playtime coughs usually point to asthma; fever and runny nose are more likely from a cold, but only a doctor can diagnose asthma.
When to Worry: Red Flags and When to See a Doctor
⚠️ Call for urgent help if any of these happen:
- Severe trouble breathing, fast‑worsening wheeze, or can’t speak in full sentences (call 911 or your local emergency number).
- Blue lips or skin, ribs pulling in with each breath, or a hunched posture to breathe.
- High fever, chills, chest pain, or coughing up colored mucus with feeling very unwell.
Schedule a visit soon if:
- Your cough lasts longer than 2–3 weeks.
- Your cough lasts more than 8 weeks, even without fever or obvious cold symptoms.
- You have frequent night coughs or repeated “chest colds.”
- Over‑the‑counter cough medicine does nothing.
Quick action can help keep mild issues from turning into emergencies.
Bottom line: Severe breathing trouble or a high‑fever cough is an emergency sign that needs urgent care right away.
Managing Colds When You Have Asthma
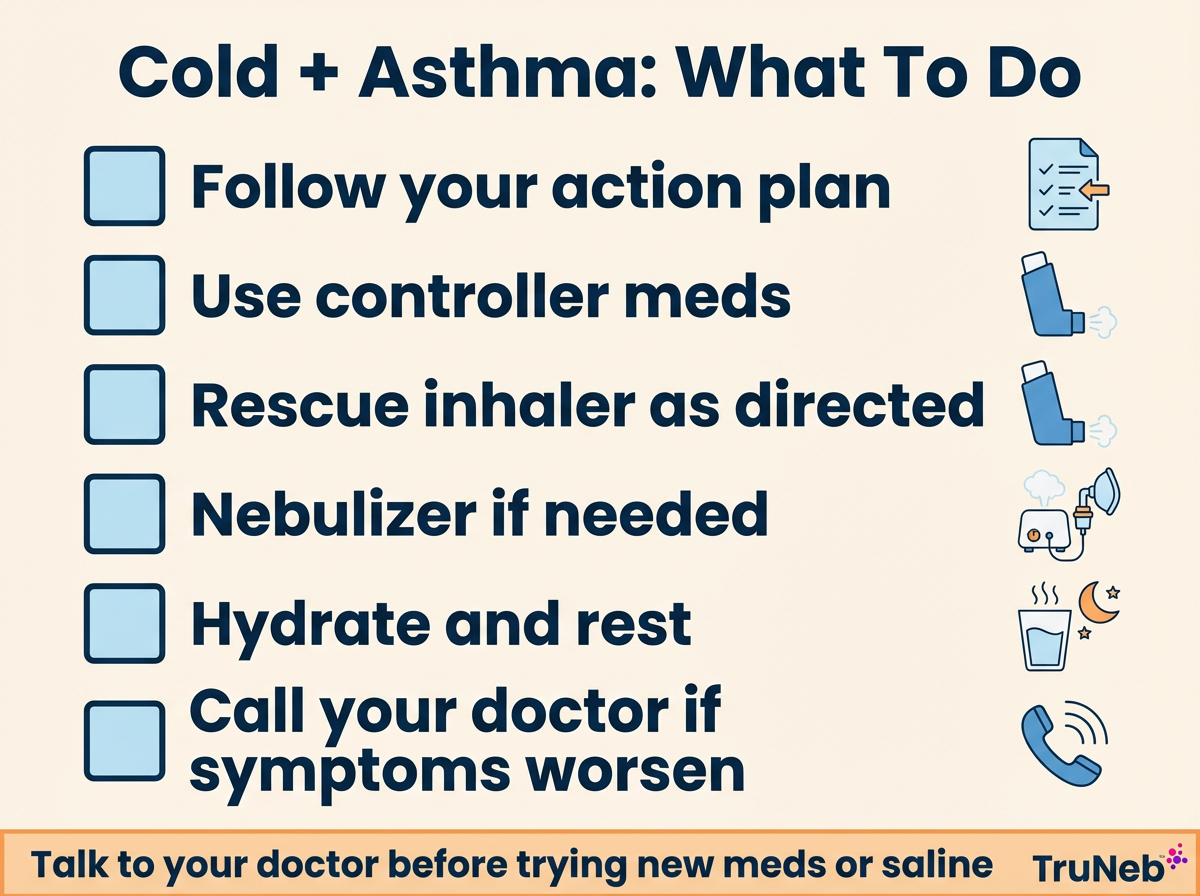
Colds can trigger asthma. A simple plan helps you stay in control.
- Follow your action plan: At the first sign of a cold, follow the steps your doctor gave you. Keep taking your controller medicine as prescribed.
- Use quick relief as your action plan describes: If you feel chest tightness or wheeze, follow the rescue inhaler steps your doctor has given you.
- Consider nebulizer therapy: When symptoms spike or for young children, a home nebulizer your doctor has recommended can make treatments easier.
- Clear the mucus: Your doctor can recommend saline by nebulizer to help loosen thick mucus. TruNeb sells 3% and 7% hypertonic saline vials that a doctor can prescribe if they’re right for you.
- ⚠️ Steam inhalers are not the same as nebulizers. Steam devices aren’t for breathing prescription asthma medicine—only use the nebulizer and medications your doctor has prescribed.
- Track and rest: If you use a peak flow meter, check daily. Rest, drink fluids, and avoid smoke and strong odors.
- Prevent the next one: Get your yearly flu shot if recommended, wash hands regularly, and don’t share inhalers or breathing equipment.
Safety note: Talk to your doctor before trying a new medication or saline strength.
Bottom line: Act early, follow your plan from your doctor, and use the tools that help you breathe easier.
Frequently Asked Questions
Tap or click a question below to see the answer:
Yes. Asthma coughs tend to last longer, flare at night or with exercise, and usually don’t cause fever or body aches. Colds are contagious and usually clear in about a week. If you’re unsure, your doctor can help sort it out.
Usually dry and tickly, sometimes ending with a wheeze or whistling sound. It can come in spasms and is worse at night or with exercise.
Yes. That’s called cough‑variant asthma. The main symptom is a chronic dry cough, usually worse at night or after a cold.
People usually manage nighttime asthma coughs by taking controller medicine as prescribed, keeping triggers out of the bedroom, and using their quick‑relief inhaler as directed in their action plan. Some people benefit from a bedtime nebulizer treatment as part of their plan. If nights stay rough, ask your doctor to adjust your plan.
Asthma coughs are usually dry or bring up small amounts of sticky mucus. If you’re bringing up a lot of phlegm with runny nose or fever, a cold is more likely.
Yes. Colds are a common trigger. Have your action plan ready and act early.
⚠️ Medical disclaimer: This article is for informational purposes only and isn’t a substitute for professional medical advice. Always talk to your doctor before changing medications or treatments.







