On this page

What Albuterol Is and Why the Right Dose Matters for Kids
Albuterol is a quick-relief bronchodilator. It relaxes tight airway muscles so your child can breathe easier. In a nebulizer, the medicine turns into a fine mist your child inhales.
Getting the dose right matters. Too little can leave wheezing and tight breathing unchanged. Too much can cause side effects like a fast heartbeat or shakiness. Your child’s dose is measured in milligrams (mg), and it should always match what’s on their prescription label.
If you’re searching “albuterol nebulizer dose for child,” here’s how doctors set it and why the exact amount matters. Nebulizers are used when kids are too young to use an inhaler well. Use albuterol for doctor-diagnosed breathing problems like asthma or bronchospasm. Always follow the plan your pediatrician gives you.
This guide is informational and doesn’t replace your child’s prescription or doctor’s advice.
Takeaway: Albuterol opens airways fast, but kids need exact, doctor-set doses.
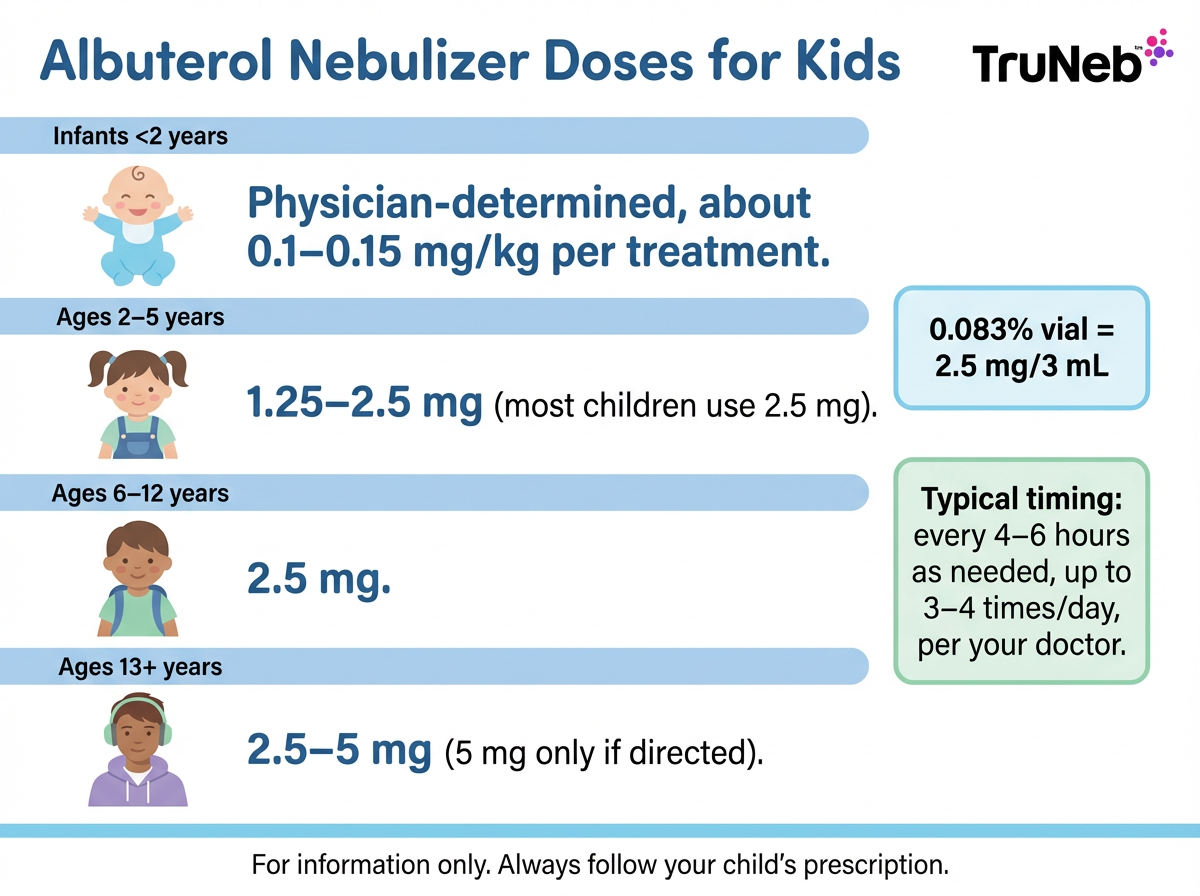
Recommended Albuterol Nebulizer Dosages by Age and Weight
These ranges explain what doctors commonly prescribe so you can understand your child’s label; they’re not meant for choosing a dose on your own.
Here are common doctor-prescribed doses families see at home. Your child’s prescription can differ based on weight and symptoms.
Infants under 2 years:
- For infants under 2, albuterol should only be used if prescribed, and the dose is always set by your child’s doctor because there isn’t a standard amount for this age.
- In select cases, doctors sometimes use weight-based dosing around 0.1–0.15 mg/kg per treatment. This weight-based dosing means the amount is matched to your child’s size, not their age alone.
Toddlers and young children 2–5 years:
- Common dose for each treatment: 2.5 mg (one premixed vial of 0.083% solution, which is 2.5 mg in 3 mL).
- Some smaller children are prescribed 1.25 mg instead. Follow the label on your child’s vial.
Children 6–12 years:
- Typical dose for each treatment: 2.5 mg (one 0.083% vial).
Teens 13+ years:
- Usually 2.5 mg per treatment. In some severe cases, up to 5 mg per treatment is used under medical supervision.
What the labels mean:
- 0.083% premixed vial = 2.5 mg/3 mL ready to use.
- 0.5% concentrate (5 mg/mL) is usually diluted by a clinician to a total of 3 mL before use.
Takeaway: Most kids 2 years and older use a 2.5 mg nebulized albuterol dose per treatment unless their doctor prescribes less.
How to Give an Albuterol Nebulizer Treatment the Right Way
Use the dose on your child’s prescription label, and don’t mix medications unless your doctor has told you to. Always follow the instructions on your nebulizer device and your child’s written treatment plan.
A typical treatment looks like this:
1) You’ll usually start by washing your hands, then pour the prescribed dose into the nebulizer cup.
2) Attach the cup to the mouthpiece or child mask.
3) Seat your child upright, calm, and comfortable (your lap works well).
4) Turn the device on and help your child take slow, normal breaths.
5) Let the treatment run until the mist stops (about 5–10 minutes).
6) When finished, remove the mask or mouthpiece. Rinse the cup and any parts that touched medicine, then let them air-dry.
If your child is upset or crying, pausing to calm them can help more medicine reach the lungs. Clean parts after each session to keep treatments effective.
Takeaway: A snug mask, calm breathing, and a clean cup make each treatment work better.
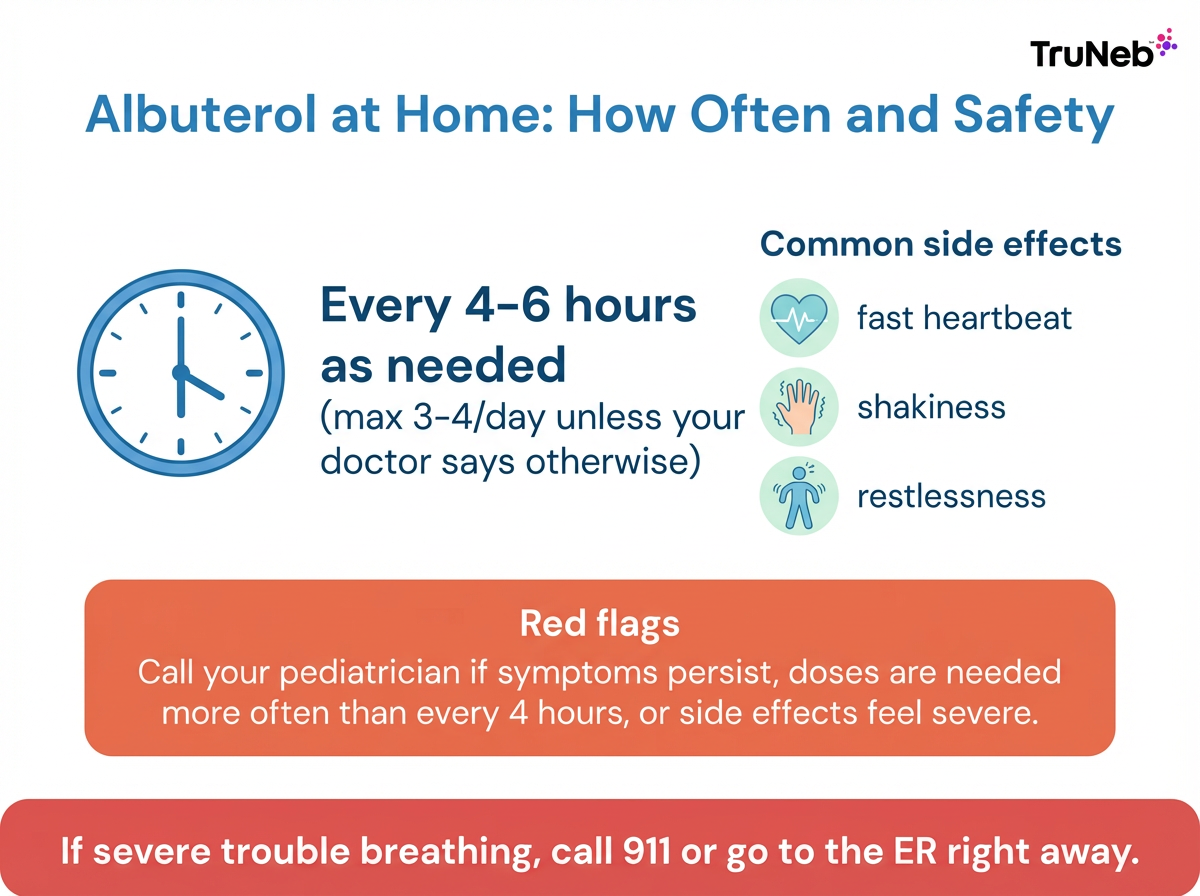
Frequency and Safety: How Often Kids Can Use an Albuterol Nebulizer
Most home asthma plans use a schedule like every 4–6 hours as needed, up to 3–4 treatments in 24 hours, as your doctor prescribed.
During a bad flare, some action plans allow back-to-back treatments (for example, every 20 minutes for 3 doses) before heading to urgent care. Only do this if it’s written in your child’s plan.
Common, short-lived side effects:
- Fast heartbeat
- Jitteriness or shakiness
- Feeling restless or “hyper”
- Mild headache or cough
Call your pediatrician if:
- Your child needs albuterol more often than every 4 hours
- Symptoms don’t improve after a treatment
- Side effects are severe or worrying
⚠️ If your child has severe trouble breathing (struggling to speak, ribs pulling in with each breath, bluish lips or face, or they seem very drowsy), call 911 or go to the emergency room right away.
Safety note: Follow your child’s written action plan for timing and doses. Never give extra or more frequent doses than prescribed.
Takeaway: Spacing albuterol nebulizer doses 4–6 hours apart and following your child’s written action plan helps keep treatments safe and effective.
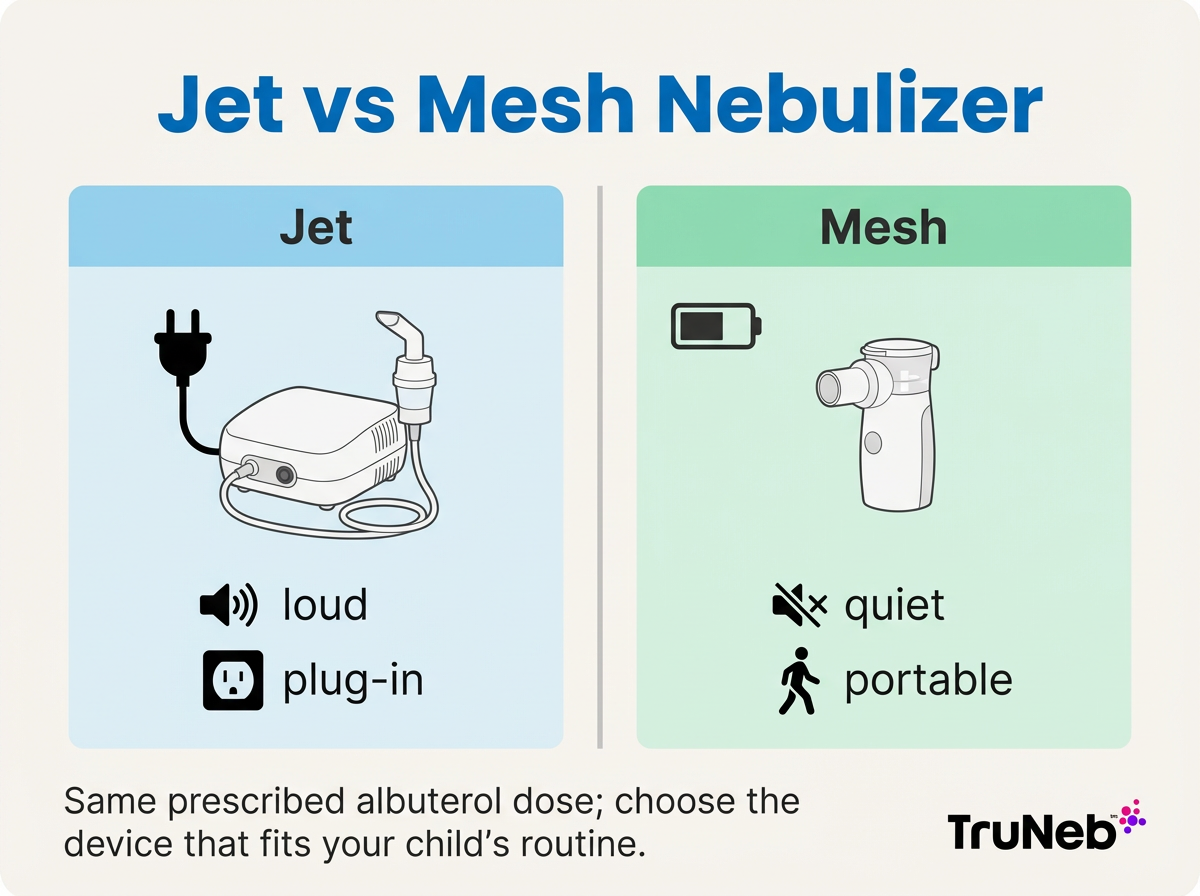
Choosing a Nebulizer for Kids: Jet vs Portable Mesh
All nebulizers turn liquid medicine into a mist. The differences are size, noise, and convenience.
- Plug-in, bulkier, and louder
- Reliable for home use
Portable mesh nebulizers:
- Handheld, very quiet, and battery-powered
- Easy to use on the go or at night without extra noise
You might also see boxes labeled “steam inhaler” near nebulizers. These devices are NOT for breathing prescription medications and shouldn’t be used in place of a nebulizer.
A portable mesh nebulizer like TruNeb™ is small and quiet, which can make treatments feel less stressful for some kids. Switching from a jet to a mesh nebulizer doesn’t change your child’s medication dose; you use the same prescription vials. If your child is old enough to use an inhaler well, an inhaler with a spacer can work just as effectively when used correctly.
Key takeaway: Mesh nebulizers are quiet and portable, while jet nebulizers are louder and plug-in; both deliver the same prescribed medicines.
| Feature | Jet (compressor) | Portable mesh |
|---|---|---|
| Power | Plug-in outlet | Battery-powered (some USB) |
| Noise | Louder | Very quiet |
| Portability | Bulky tabletop | Handheld, travel-friendly |
| Use at night | Noise can wake a child | Quiet for bedside use |
| Medication compatibility | Works with standard unit-dose vials | Works with standard unit-dose vials |
| Cleaning | Multiple parts; rinse after use | Fewer parts; rinse after use |
Note: Follow your device manual for setup and cleaning. Switching devices does not change your child’s prescription dose.
Takeaway: Mesh nebulizer models are quiet and kid‑friendly; jet nebulizers are louder and bulkier.
Beyond Albuterol: Nebulized Saline and Other Medications
Some children are prescribed sterile hypertonic saline (3% or 7%) to help loosen thick mucus. Sterile hypertonic saline ampules (such as TruNeb 3% or 7% saline) are made for nebulizer use, but should only be used if your child’s doctor prescribes them. Doctors sometimes use these saline treatments for conditions like bronchiolitis or thick mucus in lung diseases.
Other medications sometimes nebulized:
- Budesonide (an inhaled steroid) for long-term control
- Ipratropium as an add-on in severe flares, usually given in clinics or emergency settings
- Levalbuterol as an alternative bronchodilator in select cases
Important: Only place sterile, pharmacy-provided solutions in the nebulizer. Don’t add essential oils, homemade saline, or anything not prescribed.
Takeaway: Hypertonic saline loosens mucus and albuterol opens airways—use each nebulizer medicine only as your doctor directs.
Frequently Asked Questions
These quick answers cover the most common questions parents ask about pediatric albuterol nebulizer treatments. Tap or click a question below to see the answer:
Most home plans allow a treatment every 4–6 hours as needed, up to 3–4 times in 24 hours, as your doctor wrote (see the Frequency and Safety section above). If your child seems to need it more often than every 4 hours, call your pediatrician.
It isn’t used routinely unless a doctor specifically prescribes it. In young infants, albuterol doesn’t always help because their airways respond differently, so doctors are careful about when they use it. Dosing must be set by your child’s doctor.
A brief fast heartbeat, jitteriness, and restlessness are common and usually fade within 20–30 minutes. Call your doctor if side effects are severe or don’t improve.
Only if your child’s written action plan says so. Some plans allow a treatment every 20 minutes for up to 3 doses during a severe flare before seeking urgent care. If you don’t have a written plan and your child is still struggling to breathe, seek urgent care instead of adding extra doses.
They deliver the same medication. For young kids, a nebulizer with a mask is usually easier. Older children who can use an inhaler with a spacer correctly can get the same benefit.
No. Use the exact dose your doctor prescribed. Don’t split, mix, or change doses on your own. If symptoms aren’t improving, don’t keep repeating treatments outside your child’s written action plan—get medical help instead.
Takeaway: These FAQs give quick, plain-language answers about dosing, frequency, side effects, and device choices for kids’ albuterol nebulizer treatments.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk to your child’s doctor about their medications, doses, and any changes to their treatment plan.