On this page
ACBT uses relaxed breathing, deep breaths, and huff coughing to move and clear lung mucus.
ACBT is an airway clearance technique used by people with conditions like cystic fibrosis, bronchiectasis, and COPD with chronic bronchitis to help loosen and clear mucus.
What Is the Active Cycle of Breathing Technique (ACBT)?
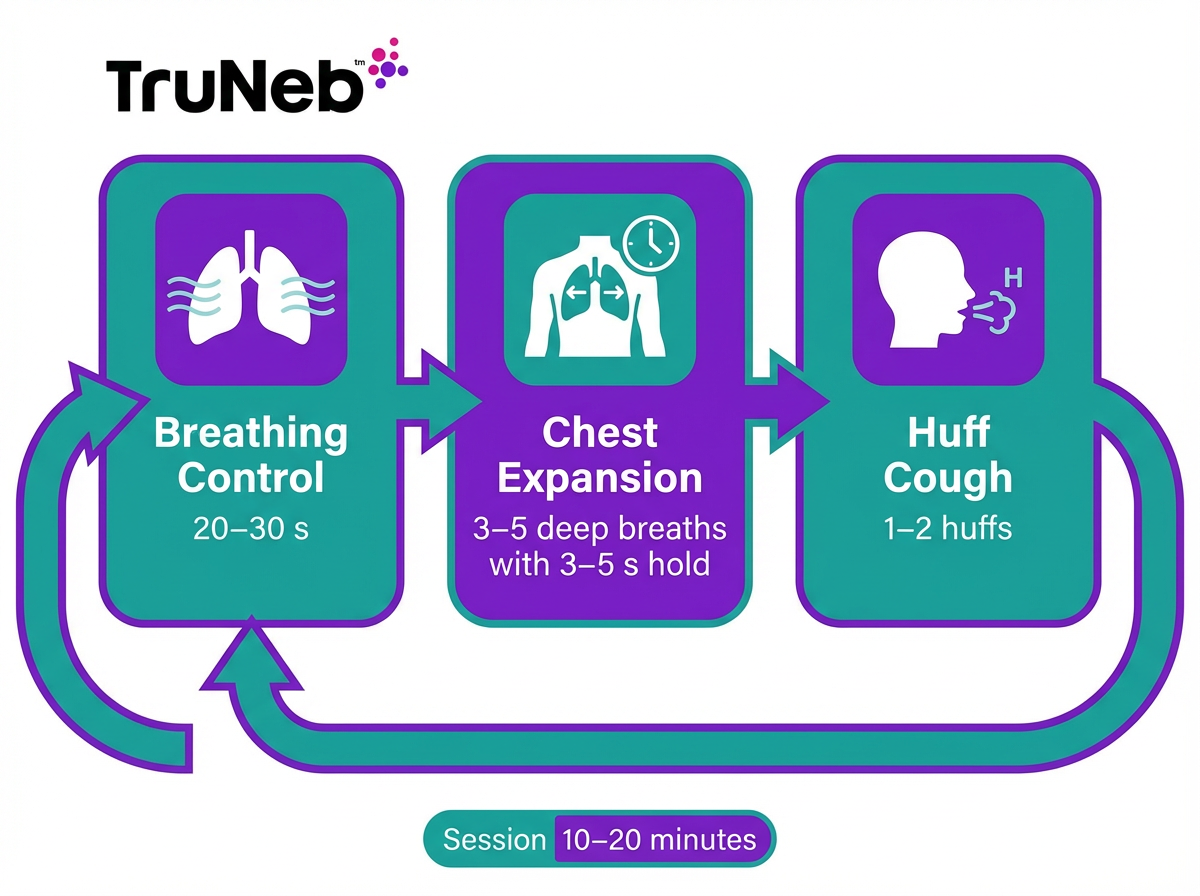
Active Cycle of Breathing Technique (ACBT) is a simple airway clearance technique that uses three repeating phases to loosen and clear mucus from your lungs without equipment. You repeat breathing control, chest expansion breaths, and huff coughing in order. The sequence relaxes tight airways, gets air behind sticky mucus in smaller airways, and then uses controlled huffs to move it upward so you can clear it. By improving airflow and helping the cilia clear mucus, ACBT can make breathing feel easier. It's usually taught by a physiotherapist or respiratory therapist. ACBT should be taught and checked by your doctor or physiotherapist—don't change your treatment routine without their guidance.
Who Should Use ACBT and When
ACBT is mainly used by people who have ongoing mucus in their lungs, such as those with cystic fibrosis, bronchiectasis, or chronic bronchitis, and during recovery from chest infections.
ACBT helps if mucus lingers and doesn't clear easily. It's widely used in cystic fibrosis, bronchiectasis, and chronic bronchitis. People also add short sessions during or after chest infections when mucus is thicker. A physiotherapist or respiratory therapist can tailor timing and pacing for you, and ACBT is usually taught in person so you can practice safely at home.
ACBT in Cystic Fibrosis
ACBT is a core part of cystic fibrosis care. Thick, sticky mucus can trap germs and lead to infections. Daily ACBT helps move mucus and keep airways open, commonly as morning and evening sessions.
ACBT in Bronchiectasis
Bronchiectasis widens airways and makes sputum pool. ACBT gives you a routine to shift that sputum and breathe easier at home. It can be done sitting or in positions your therapist suggests.
ACBT in COPD and Chronic Bronchitis
Not everyone with COPD needs airway clearance. If chronic bronchitis causes frequent phlegm, gentle ACBT can help. Breathing control calms your breathing, and huff coughs move mucus with less strain.
After Infections or Other Situations
After pneumonia, bronchitis, or a bad cold, mucus can hang around. Short runs of ACBT can help clear your chest as you heal. Ask your doctor how frequently to practice during recovery.
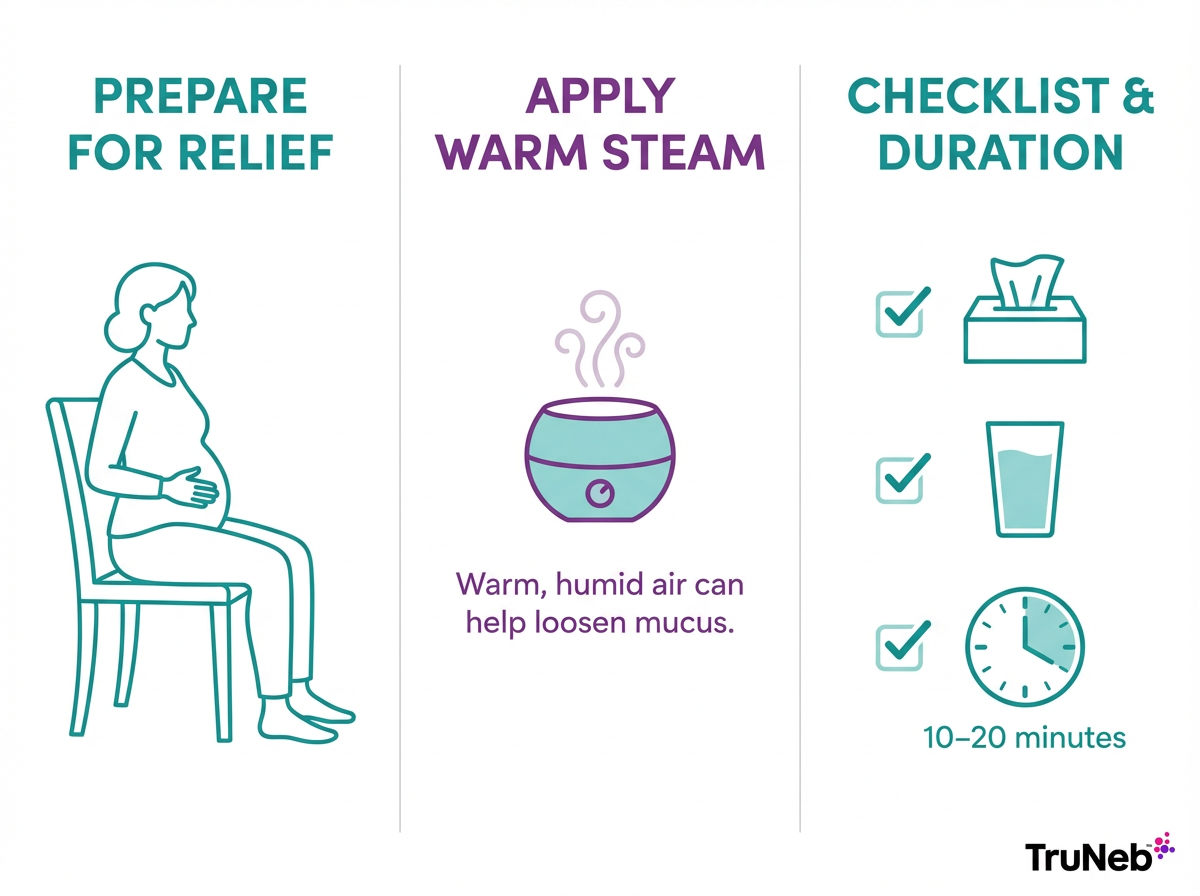
Preparing for Your ACBT Session
Good posture, a calm setting, and simple supplies like tissues make ACBT more comfortable and effective.
Sit upright with your back supported and shoulders relaxed. Place a hand on your belly to feel it rise and fall. A quiet space helps you focus. Warm, humid air, like in a steamy bathroom, can loosen mucus.
You don't need equipment, but keep tissues and water nearby. If your doctor advised an inhaler or nebulizer around ACBT, have it ready before you start. Steam inhalers aren't the same as nebulizers and shouldn't be used to breathe in prescription medications.
Step-by-Step: How to Perform the Active Cycle of Breathing Technique
ACBT is usually taught to you by your physiotherapist or doctor. The steps below describe the typical pattern they might use so you can remember what you've already been shown. Key point: In ACBT, you move from gentle relaxed breaths, to deeper chest-expanding breaths, then to controlled huff coughs to clear mucus. Don't force your breaths.
- Breathing control to relax your airways.
- Chest expansion breaths to get air behind mucus.
- Huff coughing to move mucus up and out.
Repeat in order. Rest with breathing control between parts.
Step 1: Breathing Control
Start with easy, relaxed breaths, as your therapist showed you. Breathe in gently through your nose and let your belly rise as your diaphragm moves down. Breathe out slowly through your mouth, like a soft sigh. Keep your shoulders down and your upper chest quiet. Use pursed lips if it helps control the flow. Do this for about 20 to 30 seconds, or about five to six calm breaths, until you feel settled.
If you feel light‑headed at any time, pause here and keep breathing gently until you feel steady again.
Step 2: Chest Expansion Exercises (thoracic expansion exercises)
Take a deep, slow breath in and feel your ribs widen, as your therapist showed you. Hold for about three to five seconds if that feels comfortable. Breathe out gently without forcing it. Do three to five deep breaths, then return to relaxed breathing control before the next set. These bigger breaths help air reach behind mucus so it loosens.
Step 3: Huff Cough
Huff cough (also called the Forced Expiratory Technique, or FET) starts with a medium breath in. Open your mouth and exhale firmly but steadily, like you're steaming up a mirror. Aim for a smooth "haaah" sound with a relaxed throat. One or two good huffs are usually enough before you rest with breathing control again. If you hear wheezing, you're pushing too hard. Slow down and try a gentler, longer huff. When mucus reaches your throat, a small cough can finish the job. If you keep getting very wheezy or dizzy while huffing, stop the session and follow the safety advice below or contact your doctor.
Repeating the Cycle
A full session is several rounds of breathing control, deep breaths, and huffs. Keep going until your huffs feel dry or you reach your planned time. Most sessions take about 10 to 20 minutes. End with a final gentle huff or cough if mucus is still moving.
Pro Tips for Success
Simple routine tweaks—like timing, posture, and pacing—help ACBT fit into daily life and work better for you.
Your doctor will tell you how often to fit sessions into your routine (see the FAQ below for more detail). Morning sessions can clear overnight mucus. Evening sessions can make it easier to sleep. Sit upright unless your therapist gave you a special position. Aim for steady, focused work rather than long, tiring sessions. During a flare or infection, your doctor can recommend more frequent sessions for a short time.
Combining ACBT with Nebulizers and Inhaled Medications
Key point: Many care teams ask people to use a reliever inhaler before airway clearance and to take inhaled antibiotics afterward, if those medicines are prescribed.
Short‑acting bronchodilators, such as albuterol, are commonly taken shortly before ACBT when your care team recommends it. Some people use prescribed nebulized saline (often hypertonic saline) just before or during ACBT to help thin mucus so it moves more easily.
A portable mesh nebulizer like TruNeb™ can make it easier to take prescribed treatments when you're away from home. Because it's small and quiet, it's easier to use at school, work, or while traveling.
If you use a nebulized antibiotic, clear with ACBT first so the medicine can reach deeper into cleaner airways, as your doctor directs.
Safety note: Only use medicines your doctor prescribed. Talk to your doctor before trying a new medication.
Avoiding Common Mistakes and Staying Safe
Using ACBT gently and listening for warning signs protects your airways while you clear mucus.
- Go gentle. Fast, shallow breathing can make you light‑headed. Slow down and return to breathing control if you feel dizzy.
- Don't lift your shoulders or puff your cheeks during huffs; keep your throat open and your body relaxed.
- Don't huff too hard. If you hear a wheeze, ease up and try a longer, steadier huff.
- Limit huffs to one or two before resting to avoid coughing fits.
- If you've had recent chest surgery, a pneumothorax, or other complex lung problems, ask your doctor before doing ACBT or any strong breathing exercises.
- Stay hydrated to help keep mucus thinner.
⚠️ Stop and seek urgent medical help if you have chest pain, severe shortness of breath that doesn't settle, or you cough up more than small streaks of blood. Call emergency services (911 or your local number) for sudden severe symptoms.
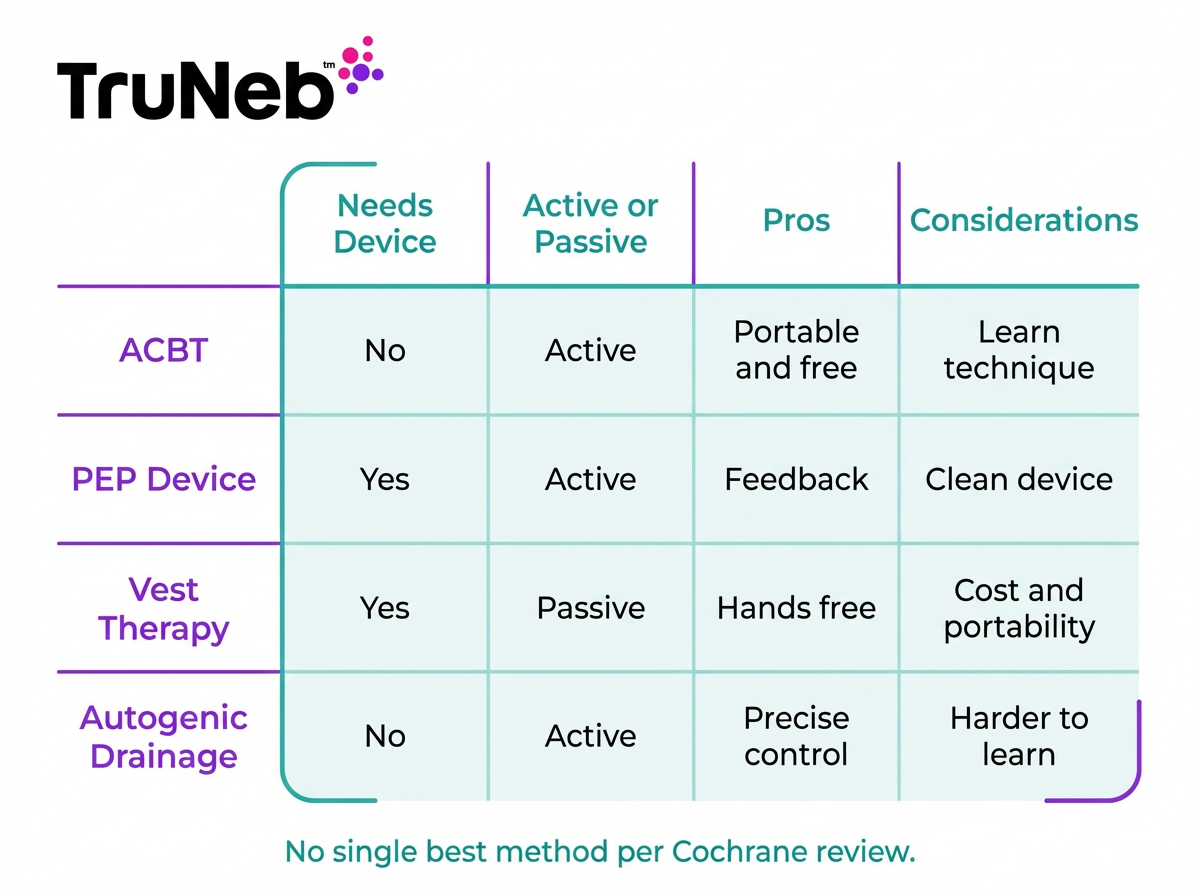
ACBT vs. Other Airway Clearance Techniques
ACBT is one of several airway clearance techniques (ACTs). Research reviews haven't found one method clearly superior for most people, so the best choice is usually the one you can do regularly with your care team's guidance.
| Technique | Needs device | How it works | Active/passive | Pros | Considerations |
|---|---|---|---|---|---|
| ACBT | No | Breathing control, deep chest/thoracic expansion, and huff coughs move mucus | Active | Portable, free, flexible, no equipment | Requires learning proper technique and pacing |
| PEP devices (Flutter, Acapella) | Yes | Exhale against resistance (sometimes with oscillation) to help keep airways open | Active | Tactile feedback, can combine with nebulizers | Device needs cleaning, carry and maintain |
| Vest therapy (HFCWO) | Yes | Inflatable vest gently vibrates chest to loosen mucus | Passive | Hands-free, useful if huffing is difficult | Bulky, costly, power needed |
| Autogenic drainage | No | Controlled breathing at low to high lung volumes to mobilize mucus | Active | Precise control without devices | Harder to learn, concentration required |
Key takeaway: No single airway clearance method is clearly best; choose the one you can do consistently and that fits your routine.
HFCWO = high-frequency chest wall oscillation.
Frequently Asked Questions About ACBT
Tap or click a question below to see the answer:
Breathing control, chest expansion breaths (thoracic expansion), and huff coughing (FET). You repeat them in a cycle until your chest feels clear.
People commonly practice once or twice daily. During flare-ups or infections, your doctor sometimes increases the number of sessions for a short time. Each session is usually 10–20 minutes. Your exact plan comes from your doctor or physiotherapist.
No. ACBT uses only your breathing and controlled huffs. Some people use inhalers or nebulized medicines around ACBT if prescribed, but the technique itself needs no device.
Yes, with guidance. Children should only do ACBT under guidance from their doctor or pediatric physiotherapist, and an adult should supervise each session. Pediatric teams routinely teach ACBT to kids with cystic fibrosis or other lung conditions.
Studies show ACBT performs about as well as PEP devices, vest therapy (high-frequency chest wall oscillation), and autogenic drainage. The best method is the one you can do consistently.
Check your technique, slow your breathing, and try gentler huffs. Make sure you're drinking enough fluids. Ask your doctor about using bronchodilators or nebulized saline around sessions if appropriate. Safety note: Talk to your doctor before trying a new medication.
Disclaimer: This article is for informational purposes only and doesn't replace professional medical advice. Always talk with your doctor about your symptoms, treatments, and how to use techniques like ACBT.