On this page
Why Croup Is Worse at Night: Explained for Parents
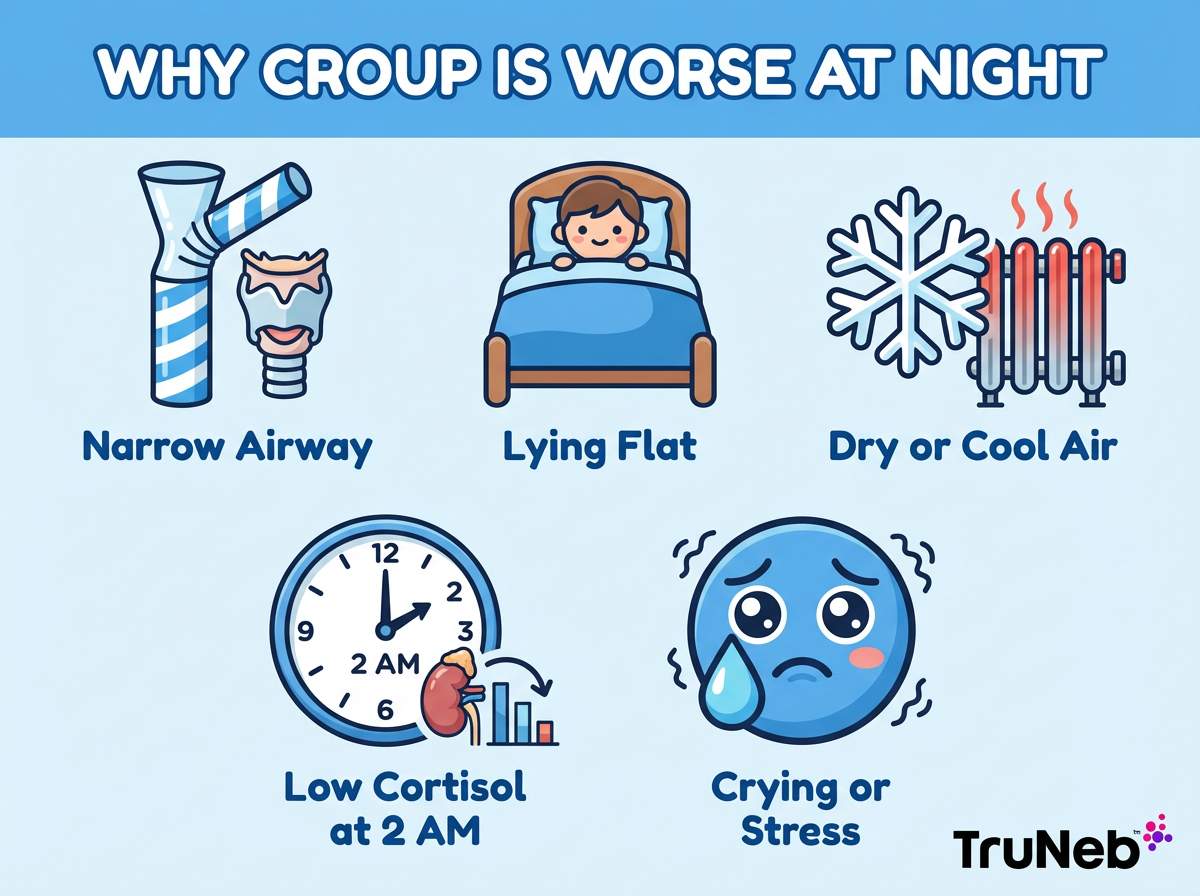
Croup can get louder after bedtime because several things stack up at once. This is most common in babies and toddlers, usually between about 6 months and 3 years. Young children have small airways. A little swelling from a virus can narrow that space a lot. Lying flat lets tissues press inward. Night air is cooler, and home heaters can dry the air, which irritates the throat. Your child's body clock also matters: natural steroids like cortisol are lowest late at night, so swelling can flare. If your child gets scared and cries, breathing speeds up and the noisy sound called stridor can get worse.
One-liner: Nighttime croup happens because small airways, lying flat, dry cool air, and lower nighttime cortisol all combine to make the barky cough sound worse.
Key point: It often sounds worse at night and eases by morning; watch how hard your child is working to breathe.
The 2 AM Barking Cough: Why Symptoms Intensify at Night
Smaller airways and swelling: Toddlers have narrow windpipes (trachea) and voice boxes (larynx). A little swelling crowds the space and creates that harsh, barky cough. During sleep, muscle tone drops, so the airway can flutter and make stridor, a high-pitched sound when breathing in.
Lying flat: On the back, mucus can pool and swollen tissues press inward. Gravity isn’t helping. Kids usually settle when held upright on your lap.
Dry and cool air: Winter nights and indoor heat dry the air. Dry air irritates an inflamed airway. Cool outside air can also trigger narrowing in sensitive airways.
Body clock: Cortisol, the body's natural steroid hormone, follows a circadian rhythm. Levels are lowest around midnight to early morning, so swelling can feel worse then.
Stress cycle: The quiet of night makes each cough sound dramatic. Fear and crying speed up breathing and can tighten the airway more, which makes the bark and stridor escalate.
A lot of kids seem fairly okay in the daytime with a hoarse cough, then flare again overnight.
One-liner: Nights make croup louder because airways are tighter, the air is drier, and natural steroid levels like cortisol are at their lowest.
How To Soothe Your Child's Croup at Night
Use these options to calm a croupy spell and ease breathing:
- Stay calm and cuddle your child. Staying calm can help slow their breathing.
- You can steam up the bathroom for about 10 minutes and sit together in the moist air.
- You can also try cool air by stepping outside for a few minutes or standing briefly in front of the freezer.
- Keep them upright. Hold them on your lap or slightly elevate the head of the bed.
- Offer warm fluids if age-appropriate. Warm water or broth can soothe; honey is okay for children over 1 year.
- Run a cool-mist humidifier by the bed for the rest of the night.
Keep the air smoke-free; cigarette or vape smoke can make breathing harder.
Safety note: Keep your child away from very hot water or steam to avoid burns, and keep any cold-air or freezer time brief and supervised.
If you’re thinking about cough or cold medicine, talk with your child’s doctor first—over-the-counter cough medicines don’t help croup and can be unsafe in young children. Stay close and listen for stridor while your child is resting.
One-liner: Calm, moist or cool air and an upright position can quickly ease a typical night croup spell for a lot of children.

Red Flags: When Croup Needs Emergency Care
Most kids can stay home, but get urgent help if you see any of these:
⚠️ Call emergency services right away if you see any of the signs below.
- Stridor at rest: You hear the harsh, high-pitched breath sound even when your child is calm or sleeping. Go to the emergency room now or call your doctor’s after-hours line for guidance.
- Working hard to breathe: Chest pulls in between ribs or at the neck (retractions), fast breathing, or they can’t speak or cry. Go to the emergency room now.
- Blue or gray lips or face: Call 911 right away.
- Drooling or trouble swallowing: Call 911 right away; this can signal severe swelling.
- Very sleepy, floppy, or very agitated and can’t be consoled: Go to the emergency room now or call your local emergency number.
- If your child is under 6 months old or has other health problems, have them seen sooner.
- If your gut says something isn’t right, or nothing helps within minutes, get medical care.
One-liner: Stridor at rest, blue lips, drooling, or severe work of breathing in a child with croup means you should get emergency care right away.
Key point: If breathing looks hard while your child is calm, it’s time to go in.
Viral Croup vs Spasmodic Croup
Viral croup comes with a cold—runny nose, hoarse voice, and sometimes fever—and is contagious like a cold. Most cases are caused by parainfluenza viruses. The barky cough usually peaks the first one to two nights, then eases.
Spasmodic croup can start suddenly at night with little or no fever and usually improves by morning. Some children have repeat night-only episodes tied to airway sensitivity, allergies, or reflux. Talk with your pediatrician about frequent episodes to look for triggers and an action plan.
Key takeaway: Viral croup is contagious and tends to peak on nights 1–2; spasmodic croup tends to recur and is linked to triggers. Comfort steps are similar.
| Feature | Viral Croup | Spasmodic Croup |
|---|---|---|
| Onset | Builds over a day or two with cold symptoms | Sudden at night, usually without prior cold |
| Fever | Low to moderate fever is common | Little or no fever |
| Cold symptoms | Runny/stuffy nose, hoarse voice | Minimal or none |
| Contagious | Yes, like a cold | No, episodes aren’t contagious |
| Worst nights | Nights 1–2 are usually the hardest | Can recur on separate nights |
| Daytime pattern | Usually seems better by day, hoarse cough lingers | Usually normal by day |
| Triggers | Viral infection (commonly parainfluenza) | Airway sensitivity, allergies, reflux |
| What to do | Comfort steps at home; call doctor for breathing trouble | Same comfort steps; discuss an action plan if episodes repeat |
One-liner: Spasmodic croup is a sudden night-only barky cough without much fever that tends to come back but responds to the same calming steps.
Doctor's Treatments for Croup and When a Nebulizer Like TruNeb™ Helps
In clinic or the ER, doctors usually give a single dose of a corticosteroid, usually dexamethasone, to reduce airway swelling. It starts working within a few hours and helps over the next day or so. For more serious cases, they can give a nebulized epinephrine treatment that works within minutes but can wear off, so monitoring is needed. Bronchodilators for asthma (like albuterol) usually don’t help typical croup, which affects the upper airway.
If your child also has reactive airway disease or wheezing with colds, your pediatrician might add specific nebulizer steps to your plan. A portable mesh nebulizer like TruNeb™ can make prescribed treatments easier at night because it’s quiet and handheld. ⚠️ Don’t confuse a steam inhaler or humidifier with a medication nebulizer like TruNeb™; steam devices aren’t designed to deliver prescription medicines and shouldn’t be used as a substitute for a nebulizer.
Medical disclaimer: Talk to your doctor before trying a new medication.
One-liner: Steroids shrink swelling over hours; epinephrine works fast but needs monitoring in medical care.
Frequently Asked Questions
Tap or click a question below to see the answer:
Stay calm and hold your child upright, then try 10 minutes in a steamy bathroom followed by a few minutes of cool night air or brief freezer breaths. Run a cool-mist humidifier and offer warm fluids if age-appropriate. If you’re considering medicine, talk with your child’s doctor first.
Go now for stridor at rest or hard work of breathing. Call 911 for blue or gray lips/face or for drooling with trouble swallowing.
Most cases improve in 3 to 5 days. Nights 1 and 2 are usually the hardest; the hoarse, barky cough can linger a bit longer.
A night-only croup pattern with little or no fever that tends to recur. Use the same calming steps, and ask your pediatrician about possible triggers (such as reflux or allergies) if episodes repeat.
Not unless your doctor tells you to. Typical croup is an upper-airway problem, so asthma inhalers don’t usually help. If your child has a plan that includes nebulized medicine or saline, follow it. A quiet portable device like TruNeb can help deliver prescribed treatments.
Viral croup is contagious, especially in the first few days. Use good handwashing and keep your child home if they have a fever or new cough.
One-liner: Nights 1 and 2 are usually the hardest; if your child is working hard to breathe while resting, seek urgent medical care.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your child’s symptoms and before starting, stopping, or changing any treatment. If you think your child is having a medical emergency, call 911 or your local emergency number right away.