On this page
Lung nodules, those small spots or growths in the lungs, are often found by chance during imaging tests for other health issues. While most nodules are harmless and non-cancerous, it's completely natural to feel anxious if one is found on your x-ray. Understanding when to worry about lung nodules can be helpful in managing your health. We'll walk you through the important factors to consider, how to interpret medical advice, and when it might be time to explore further testing or treatment.
Understanding Lung Nodules
What are lung nodules?
Lung nodules are small, round or oval-shaped growths that can show up in your lungs, usually less than 3 centimeters in size. They appear as a spot or shadow on an X-ray or CT scan. These nodules can be from past infections, benign tumors, or in some cases, they can be an early sign of lung cancer.
The main difference between benign (non-cancerous) and malignant (cancerous) nodules lies in their growth patterns and structure. Benign nodules typically stay the same size over time and don’t spread, whereas malignant nodules can grow and spread, which is a sign of cancer. Knowing this difference helps guide the next steps in your care.
How common are lung nodules?
Lung nodules are actually quite common, especially as more people undergo imaging tests for various reasons. Up to half of adults who get chest imaging will have at least one lung nodule. The good news is that around 95% of these nodules are benign.
Several factors can lead to the development of lung nodules:
- Infections: Past infections, like tuberculosis or fungal infections, can leave behind scar tissue that forms a nodule.
- Inflammation: Conditions like rheumatoid arthritis or sarcoidosis can cause inflammatory nodules to form.
- Environmental Exposure: Long-term exposure to harmful substances like dust, asbestos, or pollutants can also result in lung nodules.
Understanding these causes can help you feel more confident in knowing when to worry about lung nodules.
Symptoms associated with lung nodules
One reason lung nodules go unnoticed is that they usually don’t cause any symptoms. Most nodules are too small to cause noticeable issues, so they’re sometimes discovered accidentally during imaging for something else.
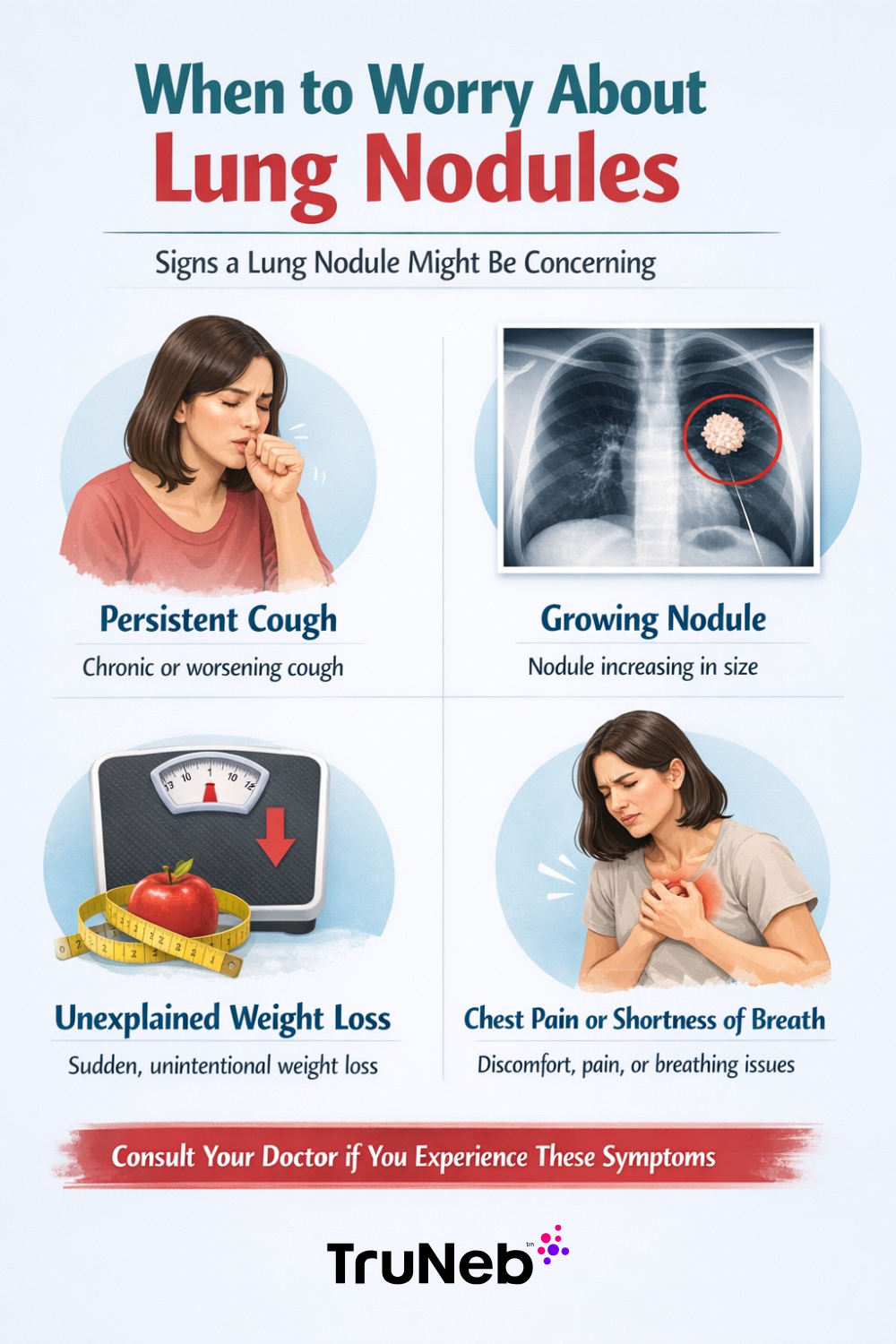
However, there are certain symptoms that mean a lung nodule needs closer attention:
- Cough That Won't Go Away: A cough that lingers, especially one that includes blood, could be a warning sign.
- Shortness of Breath: Any new or worsening shortness of breath is worth discussing with your doctor.
- Unexplained Weight Loss: Losing weight without trying can be a signal of a more serious condition, like cancer.
If you’re experiencing any of these symptoms, check in with your healthcare provider. Addressing potential issues early on can make a big difference in how they’re managed.
Risk Factors and Causes
What increases the risk of lung nodules?
Several factors can increase your chances of developing lung nodules, and knowing these can help you understand your own risk level.
Smoking History and Its Impact
One of the biggest risk factors for lung nodules is a history of smoking. Whether you’re a current smoker or you quit years ago, smoking has lasting effects on your lungs. Smokers and former smokers are more likely to develop lung nodules, and unfortunately, these nodules are also more likely to be cancerous. The longer and more heavily you’ve smoked, the greater your risk.
Age, Family History, and Exposure to Environmental Toxins
As we age, our risk of developing lung nodules naturally increases. This is because our lungs have been exposed to more over the years—whether that’s pollution, infections, or irritants. If lung cancer or other lung diseases run in your family, this can also raise your risk.
Environmental exposure is another risk. Long-term exposure to harmful substances like asbestos, radon, or certain chemicals can cause lung nodules. Even if you’ve never smoked, living in areas with high air pollution or being around secondhand smoke can still put you at risk. Being aware of these factors can help you make informed decisions about your health, like avoiding further exposure and keeping up with regular check-ups.
Non-cancerous causes of lung nodules
When you hear about lung nodules, it’s easy to jump to the worst-case scenario, but know that most nodules are actually benign and harmless.
Infections, Inflammations, and Scar Tissue
Previous infections are a common cause of lung nodules. If you’ve had illnesses like tuberculosis, pneumonia, or fungal infections including histoplasmosis, they can leave behind scar tissue that shows up as a nodule on a scan. These types of nodules usually don’t grow over time, which is a reassuring sign that they are noncancerous.
Inflammation in the lungs can also lead to nodule formation. This might happen if you’ve had chronic conditions like bronchitis or if you’ve been exposed to lung irritants like dust or smoke over a long period. In these cases, the nodules are part of your body’s natural response to ongoing irritation or injury in the lungs.
Autoimmune Diseases and Other Benign Conditions
Certain autoimmune diseases, like rheumatoid arthritis or sarcoidosis, can also cause lung nodules. These conditions cause your immune system to mistakenly attack your own tissues, leading to inflammation that can result in nodules. While these nodules can look concerning, they’re usually not cancerous.
Other noncancerous conditions, like hamartomas (a type of benign tumor) or pulmonary fibrosis, can also cause nodules to develop. These nodules typically stay stable over time and are managed through regular check-ups to make sure they don’t change.
Understanding that many lung nodules are caused by noncancerous conditions can help ease some of the anxiety that comes with their discovery. Remember, having a lung nodule doesn’t automatically mean something serious is wrong. Many people have lung nodules that never cause problems and require nothing more than routine monitoring.
Diagnosing and Monitoring Lung Nodules
How are lung nodules detected?
Lung nodules are often detected through imaging tests, which might sound a bit technical, but it’s actually pretty straightforward.
Common Imaging Techniques (X-ray, CT Scan)
The most common ways to spot a lung nodule are through chest X-rays or CT scans. A chest X-ray is usually the first step and can show if there’s something unusual in your lungs. However, because X-rays only provide a basic image, CT scans are often used to get a more detailed look. A CT scan takes multiple X-ray images from different angles to create a comprehensive picture of your lungs, allowing doctors to see nodules more clearly and assess them better.
Incidental Findings in Diagnosis
Interestingly, many lung nodules are discovered by accident—what doctors call “incidental findings.” For example, if you go to the hospital for something unrelated, like a car accident or a check-up for another condition, and you get a chest X-ray or CT scan, a lung nodule might show up unexpectedly. While it can be a surprise to hear you have a nodule, it’s a good thing that it was found early, giving you and your doctor more options for monitoring or treatment if needed.

Understanding your imaging results
Once a lung nodule is detected, your doctor will closely examine the imaging results to understand more about it.
Size, Shape, and Location of Nodules
The size, shape, and location of a nodule help doctors know whether it’s something to worry about. Generally, smaller nodules (less than 6 millimeters) are less likely to be cancerous, while larger ones may require closer monitoring. The shape also matters—nodules with smooth, round edges are typically less concerning than those with irregular or spiculated (spiked) edges.
Where the nodule is located in your lungs can also provide clues. For example, nodules found in the upper lobes of the lungs are often more suspicious than those in the lower lobes. These characteristics alone don’t tell the whole story, which is why your doctor will consider them along with other factors like your age, smoking history, and any symptoms you might have.
What Characteristics Might Be Concerning
Certain characteristics of a nodule can raise red flags. If the nodule is growing over time, has irregular borders, or is solid and dense, your doctor might be more concerned about the possibility of cancer. The nodule causing symptoms like coughing or shortness of breath could be concerning too.
When to get a biopsy
If there’s enough concern about a nodule, your doctor might recommend a biopsy to get a closer look.
Criteria for Recommending a Biopsy
A biopsy is usually recommended if the nodule has certain characteristics that suggest it could be cancerous, like being larger, having irregular edges, or showing signs of growth over time. Your personal and family medical history and risk factors like smoking will also be considered.
Different Biopsy Techniques and What to Expect
There are a few different ways to perform a biopsy, and the method used will depend on the size and location of the nodule, as well as your overall health.
- Needle Biopsy: This is the most common type and involves using a thin needle to remove a small sample of the nodule. It’s usually done with the help of a CT scan to guide the needle to the right spot. You’ll be awake during the procedure, but a local anesthetic will numb the area so you don’t feel pain.
- Bronchoscopy: In this procedure, a thin, flexible tube called a bronchoscope is passed through your mouth or nose and down into your lungs. The doctor can then collect a tissue sample from the nodule. You’ll likely receive sedation to keep you comfortable during the procedure.
- Surgical Biopsy: If the nodule is in a hard-to-reach area or if more tissue is needed for an accurate diagnosis, a surgical biopsy might be recommended. This involves a small incision in your chest to access the nodule and is done under general anesthesia.
Your doctor will discuss which option is best for you, based on your situation. A biopsy might sound intimidating, but it’s an important step in figuring out how to treat it.
Treatment Options and Next Steps
When a lung nodule is found, one of the first decisions you and your doctor will make is whether to just monitor it or take action now. The choice depends on a few things, including the characteristics of the nodule, your overall health, and any potential risk factors you may have.
Keeping an Eye on Low-Risk Nodules
If your nodule is small, has smooth edges, and isn’t showing signs of growth, your doctor might suggest a "watchful waiting" approach. This involves regular check-ups and imaging tests, usually with CT scans, to keep an eye on the nodule over time. The goal is to see if the nodule changes in size, shape, or appearance. If it stays the same, it’s likely benign and may not require any further action.
Surveillance might sound passive, but it’s actually a proactive strategy that allows your doctor to catch any changes early on. You might have follow-up scans every six months to a year, depending on your individual situation. This approach helps avoid unnecessary procedures while making sure any potential issues are caught quickly.
When More Aggressive Treatment Is Necessary
A nodule may show signs that make your doctor recommend a more aggressive approach. This could include nodules that are larger, have irregular or spiculated edges, or have shown growth in a short period. If there’s a higher suspicion that the nodule could be cancerous, your doctor may suggest moving beyond monitoring to more definitive treatments.
The decision to move to a more aggressive treatment plan is based on imaging results, your risk factors (like smoking history), and your overall health. Your doctor will discuss the options with you, taking into account the big picture.
Treatment approaches for concerning nodules
If your doctor determines that a nodule is concerning and could be cancerous, there are several treatment options available. The choice of treatment will depend on the nodule’s characteristics, its location in the lung, and your overall health.
Surgical Options
Surgery is often the first line of treatment for nodules that are suspected to be cancerous. There are a few different surgical options, depending on the size and location of the nodule:
- Wedge Resection: This is a minimally invasive surgery where only the nodule and a small margin of surrounding tissue are removed. It’s often used for smaller nodules that are easy to access. Recovery time is generally shorter with this procedure, and it can be a good option if the nodule is small and located near the edge of the lung.
- Lobectomy: If the nodule is larger or located deeper within the lung, a lobectomy might be recommended. This surgery involves removing an entire lobe of the lung (the lung is divided into sections called lobes). While it’s a more extensive procedure, a lobectomy can be very effective in removing cancerous tissue and reducing the risk of recurrence.
Your surgeon will talk about the risks and benefits of each option, so you can make an informed choice.
Non-Surgical Treatments and Clinical Trials
Surgery may not be the best option if the nodule is in a difficult location, if surgery poses too many risks from other health issues, or if you want a less invasive approach. There are several non-surgical treatments available:
- Radiation Therapy: This treatment uses high-energy rays to target and kill cancer cells. It’s often used when surgery isn’t an option, or in combination with surgery to ensure all cancer cells are eliminated.
- Chemotherapy: While less common for early-stage lung nodules, chemotherapy might be recommended if there’s a concern that cancer cells have spread beyond the nodule. Chemotherapy uses powerful drugs to kill cancer cells throughout the body.
- Targeted Therapy and Immunotherapy: These are newer treatments that focus on specific aspects of cancer cells or boost the body’s immune system to fight the cancer. They’re often used in more advanced cases or when traditional treatments aren’t possible.
- Clinical Trials: If standard treatments aren’t an option, or if you’re interested in exploring cutting-edge therapies, your doctor might suggest participating in a clinical trial. Clinical trials test new treatments that aren’t yet widely available and can offer access to innovative therapies. Your doctor can help you understand whether a clinical trial is a good fit for you and what the potential benefits and risks might be.
Each of these treatments has its own set of considerations, and your healthcare team will work with you to figure out the best way to go. The most important thing is that you feel informed and supported in knowing when to worry about lung nodules and what to do.
Staying Informed and Proactive
Advances in lung nodule research
Staying informed about the latest developments in lung nodule research can help you feel more empowered and confident in your healthcare journey. There’s always something new on the horizon, and understanding these advances can make a big difference in how lung nodules are detected and managed.
Emerging Technologies in Lung Nodule Detection
Technology in healthcare is constantly evolving, and that’s great news for anyone dealing with lung nodules. One of the most exciting areas of advancement is in imaging technology. Newer, more sophisticated CT scanners are able to detect even the tiniest nodules with greater accuracy than ever before. These scanners produce clearer, more detailed images, allowing doctors to spot potential issues earlier than ever.
Artificial intelligence (AI) is starting to play a role in lung nodule detection. AI algorithms can analyze scans more quickly and accurately than ever before, highlighting areas of concern that might be missed by the human eye. This technology is still in the early stages, but it’s showing a lot of promise for improving early detection and reducing unnecessary biopsies.
Current Research and What It Means for Patients
Ongoing research is also shedding light on how to better predict which lung nodules are likely to be cancerous and which are not. For example, researchers are studying genetic markers and other biological signals that could indicate a nodule’s potential to become malignant. This research is leading to the development of blood tests and other non-invasive methods that could help doctors determine the best course of action without needing to perform a biopsy.
For patients, this means that in the near future, lung nodule management could become even more personalized and less invasive.
Ongoing Studies
The Mayo Clinic currently has a dozen lung nodule studies in process to advance technology, diagnosis, and treatment of lung nodules. We’re excited to see how this field advances in the coming years!
Additional Resources: When to Worry About Lung Nodules
Check out the additional resources for lung nodule research, treatment, and support below: The Society of Thoracic Surgeons - Lung Nodule Resources
Lung Nodules - Patient Information Leaflets
Hopefully you have a better idea of when to worry about lung nodules and when to not! Ultimately, proper diagnosis and monitoring will help your doctor decide the best course of action.
*Article reviewed by a licensed Registered Respiratory Therapist