On this page
What Does Green Phlegm Mean?
Green phlegm usually means your immune system is fighting an infection in your airways. The green tint comes from white blood cells building up in your mucus as they trap and clear germs. Both viruses and bacteria can cause this change.
Phlegm is the mucus you cough up from your chest.
Color is just one clue, not a full diagnosis. How you feel, how long it’s lasted, and signs like fever or shortness of breath matter more than color alone.
Key takeaway: Green phlegm usually means your immune system is actively fighting an infection, but the color alone doesn’t mean you automatically need antibiotics.
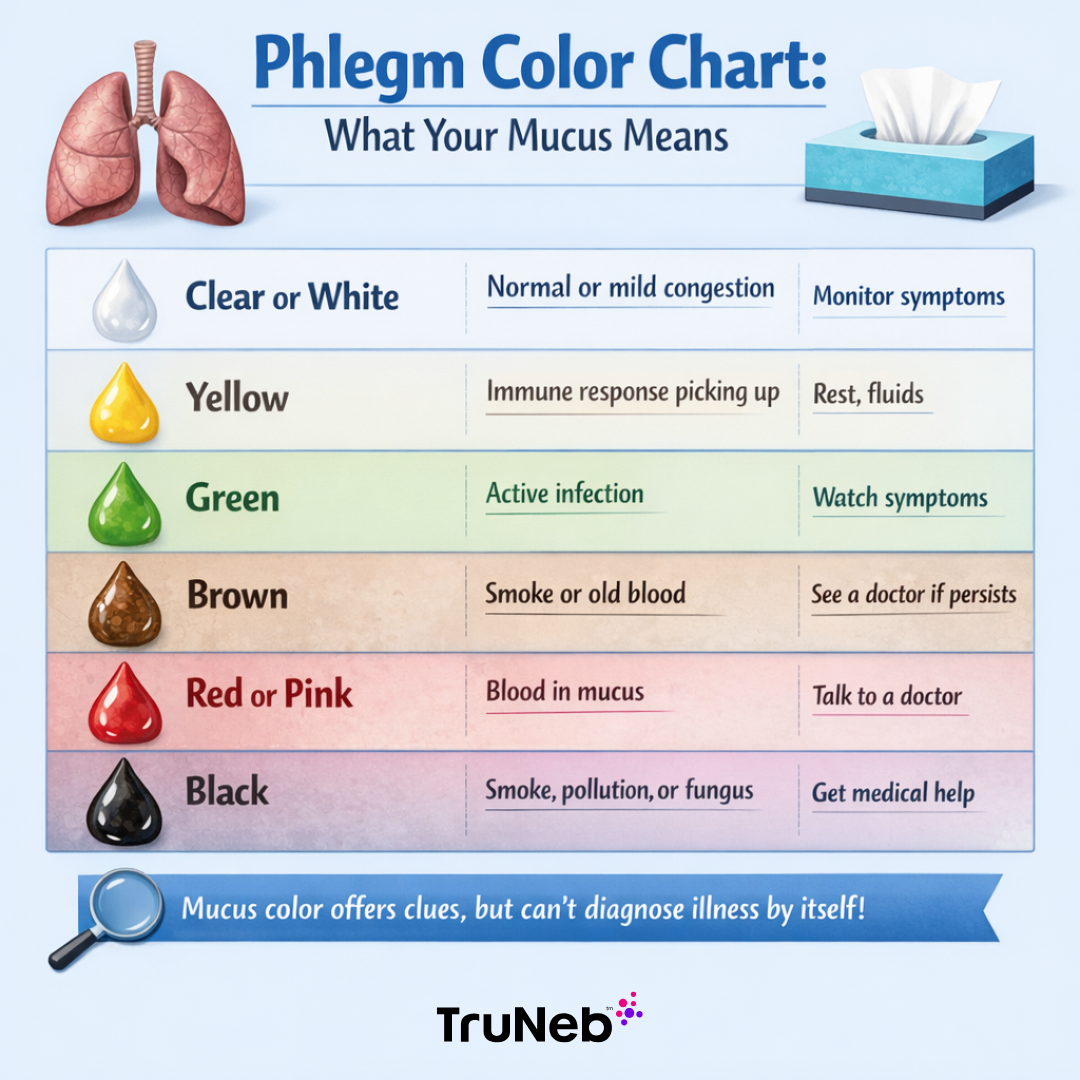
Phlegm Color Chart: What Different Mucus Colors Signal
Mucus usually starts yellow and can turn green as your immune response ramps up.
| Color | What it can signal | Check / action |
|---|---|---|
| Clear or white | Usually normal or mild congestion from allergies or an early cold | Monitor symptoms |
| Yellow | Immune response is picking up | Rest, fluids |
| Green | High number of immune cells during an active fight | Watch overall symptoms and timeline |
| Brown | Old blood or irritation from smoke or pollution | If persistent, talk to a doctor |
| Red or pink | Fresh blood | If more than a few streaks, talk to a doctor |
| Black | Smoke, heavy pollutants, or rarely fungal issues | Get medical advice promptly |
Mucus color can give you clues about what’s going on, but it can’t diagnose a specific illness by itself.
Key takeaway: Mucus color can give you clues about what’s going on, but it can’t diagnose a specific illness by itself.
Why Phlegm Turns Green
When you get sick, your body sends white blood cells called neutrophils to your airways. These cells carry a green-tinted enzyme. When a large number of these cells gather and break down in mucus, the mucus can look green.
This immune response happens in both viral and bacterial infections, so color alone can’t tell you what kind of germ is causing it. People usually notice mucus move from clear to yellow to green as an illness peaks, then lighten again as they recover.
Key takeaway: Phlegm turns green because infection-fighting white blood cells break down in your mucus during an active immune response.
Causes of Green Phlegm
- Common cold or flu: Usually starts clear or yellow and can turn green as your immune response peaks.
- Acute bronchitis: Usually viral. Deep cough with yellow or green mucus.
- Sinus infection: Thick green nasal mucus can drip into the throat and be coughed up, typically with facial pressure.
- Pneumonia: More serious. Green, yellow, or rusty mucus with high fever, chest pain, and shortness of breath.
- Chronic bronchitis or COPD: Daily mucus is common. A change to green can signal a flare or infection.
- Bronchiectasis or cystic fibrosis: Recurrent infections with thick, sometimes foul-smelling green sputum.
- COVID-19: Some cases develop phlegm. Green mucus can appear with severe illness or a secondary infection.
Bronchitis and pneumonia are examples of chest infections that can cause green phlegm.
Key takeaway: Green phlegm can come from a range of infections, from colds and sinusitis to bronchitis and pneumonia.
Green Phlegm with Other Symptoms
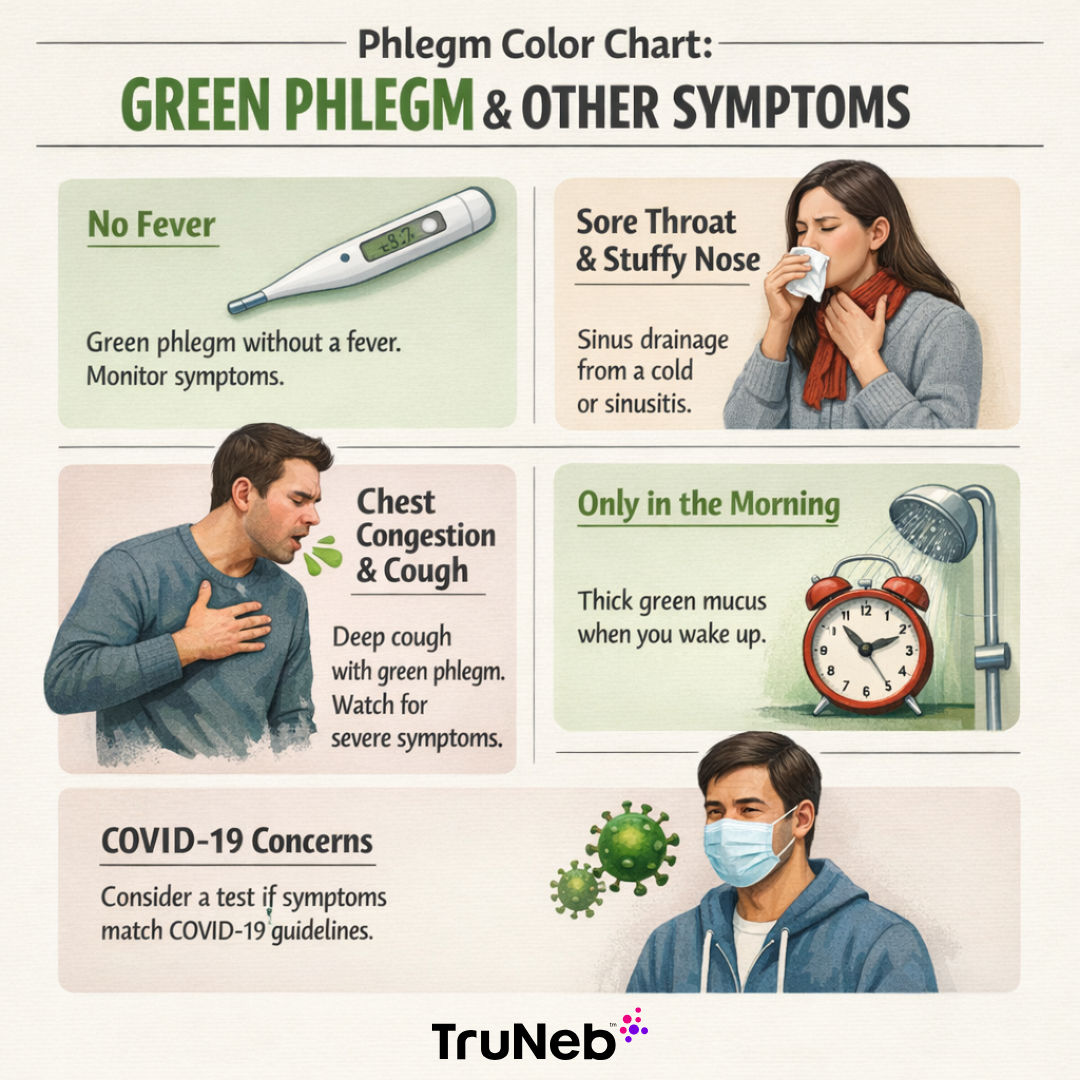
No Fever
You can have green mucus without a fever, especially with mild viral infections or while recovering. Lack of fever doesn’t rule out infection. Keep an eye on how you feel and how your cough changes.
Sore Throat and Stuffy Nose
Thick green snot plus a scratchy throat usually points to sinus drainage from a bad cold or sinusitis.
Chest Congestion or Deep Cough
A deep, chesty cough with green phlegm points to a lower airway issue like bronchitis. High fever, chest pain, or trouble breathing raises concern for pneumonia.
Only in the Morning
Mucus pools and thickens overnight. Some people notice dark green phlegm in the morning that clears after you hydrate and shower.
COVID-19 Context
Some COVID-19 cases develop phlegm; green mucus can show up with severe illness or a secondary infection. If you’re not sure and your symptoms match current COVID-19 guidance, consider taking a test.
Key takeaway: To understand green phlegm, always look at your other symptoms and how long you’ve been sick, not the color alone.
Am I Contagious If I Have Green Phlegm?
If you’re actively coughing up phlegm and have other symptoms like fever, sore throat, or body aches, it’s safest to assume you can spread germs and stay home. Coughing sends droplets into the air.
Many doctors use a rule of thumb: wait until you’ve been fever-free for 24 hours without medicine and your symptoms are improving before going back to work or school.
When green phlegm is your only symptom and you feel well otherwise, you’re less likely to be very contagious. Still use good hygiene: cover coughs, wash hands, and consider a mask in close spaces.
Key takeaway: If you’re coughing up green phlegm and feel sick, it’s safest to stay home and rest until your fever is gone and symptoms are improving.
Does Green Phlegm Mean I Need Antibiotics?
Not by itself. Green phlegm by itself doesn’t prove you need antibiotics. Most cases are caused by viruses, and antibiotics don’t help viruses.
Doctors don’t prescribe antibiotics based on color alone. They look at how long you’ve been sick, whether you have a high fever, chest findings, or signs of pneumonia or bacterial sinusitis.
Watch the timeline: viral bronchitis and colds usually improve within 1–3 weeks. If symptoms last beyond about 10–14 days, get worse after a brief improvement, or you develop high fever or shortness of breath, a doctor might check for a bacterial infection. Unneeded antibiotics can cause side effects and contribute to antibiotic resistance.
Key takeaway: Doctors base antibiotic decisions on how long you’ve been ill and how sick you are, not on phlegm color alone.
How to Get Rid of Green Phlegm at Home
- Stay hydrated: Water, warm tea, and broths thin mucus and make coughing it out easier.
- Inhale steam and add humidity: Steamy showers or a humidifier loosen chest and sinus congestion.
- Use saline: A saline nasal spray or rinse clears thick nasal mucus. Some people benefit from nebulized saline to moisten the airways.
- Practice controlled coughing: Gentle, purposeful coughs help bring phlegm up without exhausting you.
- Ask your doctor about an expectorant: An option like guaifenesin can help thin mucus. Always follow the label instructions.
- Try a portable mesh nebulizer: a device like the TruNeb™ portable mesh nebulizer can be used with sterile normal saline, or with hypertonic saline if your doctor prescribes it. The fine mist can help moisten and thin stubborn mucus so you can clear it more easily. It doesn’t replace medical treatment but can make thick mucus easier to clear. Clean the device after each use.
- Rest and elevate your head: Give your body time to recover and sleep propped up to reduce nighttime coughing.
Safety note: Talk to your doctor before trying a new medication or hypertonic saline.
Key takeaway: The best home care focuses on thinning, loosening, and clearing mucus with fluids, humidity, saline, gentle coughing, and rest.

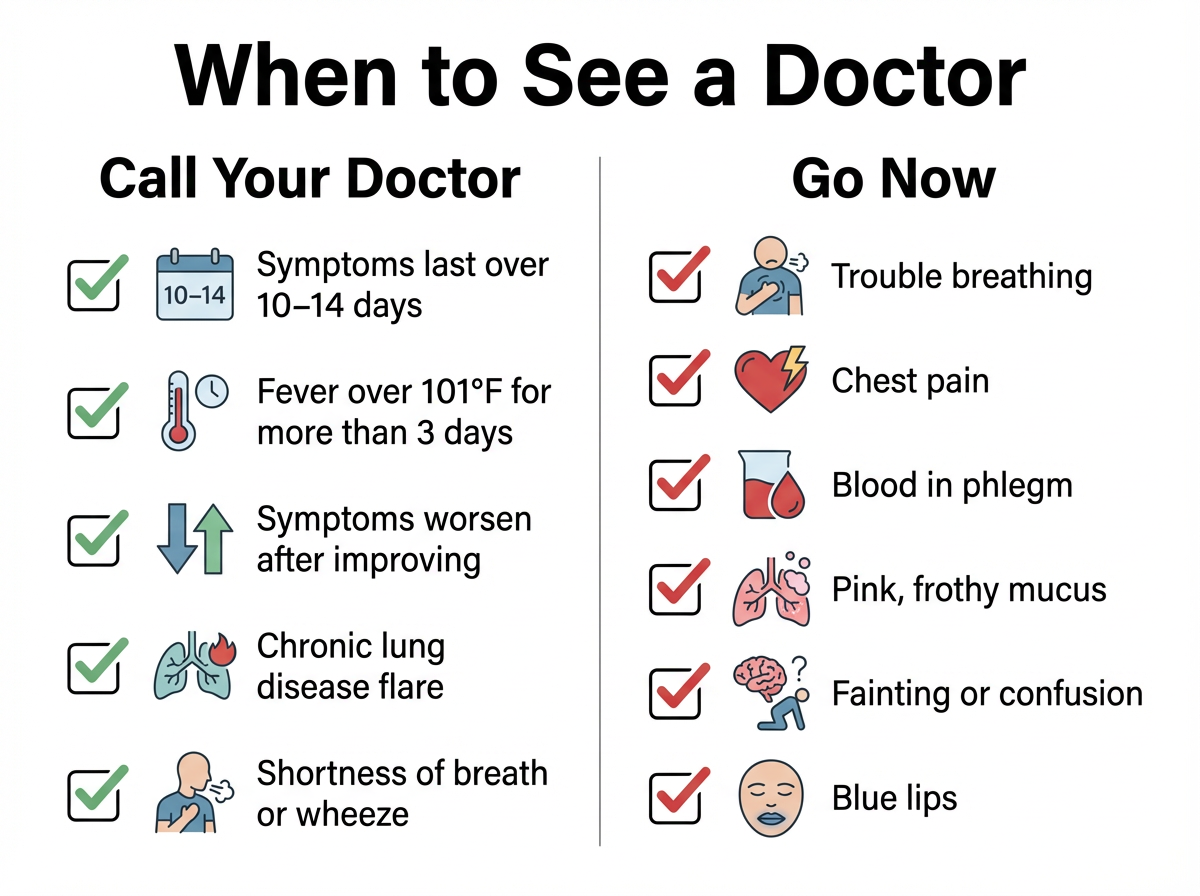
When to See a Doctor for Green Phlegm
Call your doctor if:
- Your cough and green phlegm last more than 10–14 days or get worse after improving.
- You have a fever above about 101°F (38.3°C) for more than 3 days, or a fever that returns.
- You feel short of breath, wheezy at rest, or have chest discomfort.
- You have asthma, COPD, or another chronic lung disease and your symptoms are flaring.
⚠️ Get urgent help right away if you notice any of the following:
Seek urgent or emergency care if:
- You have trouble breathing, chest pain, or blue-tinged lips.
- You cough up more than a few streaks of blood, or pink, frothy phlegm.
- You faint, feel confused, or your child is in distress.
Doctors may examine your chest, order a chest X-ray, or check a sputum sample to guide treatment.
Key takeaway: Get medical help if green phlegm lasts more than a week or two, gets worse, or comes with trouble breathing, chest pain, or blood.
Frequently Asked Questions
Tap or click a question below to see the answer:
Not always. It shows a high number of white blood cells in your mucus, which happens in viral and bacterial infections. Color alone can’t tell the germ type.
Not by itself. Mucus usually moves from clear to yellow to green as your immune response ramps up. The overall symptoms and timeline matter more than the exact shade.
Not by itself. Green usually appears at the height of the illness. You’re getting better when your fever drops, your cough eases, and mucus lightens again.
For a typical viral infection, a few days to about a week, with the whole cold lasting 1–2 weeks. Some coughs can linger up to 2–3 weeks. When you’re not improving by about two weeks, check in with your doctor.
Allergies usually cause clear or white mucus. Green usually points to infection. Bad allergies can set the stage for a sinus infection that turns mucus green.
When you otherwise feel okay, it could be leftover from a recent cold or sinus drainage. Hydrate and monitor. If new symptoms appear or it persists, talk with your doctor.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk to your doctor about your symptoms and before starting, stopping, or changing any treatment.
If you’re worried or things just don’t feel right, it’s always okay to call your doctor—they can help you sort out what’s going on.







