On this page

Urgent Care for Asthma: Home, Clinic, or 911
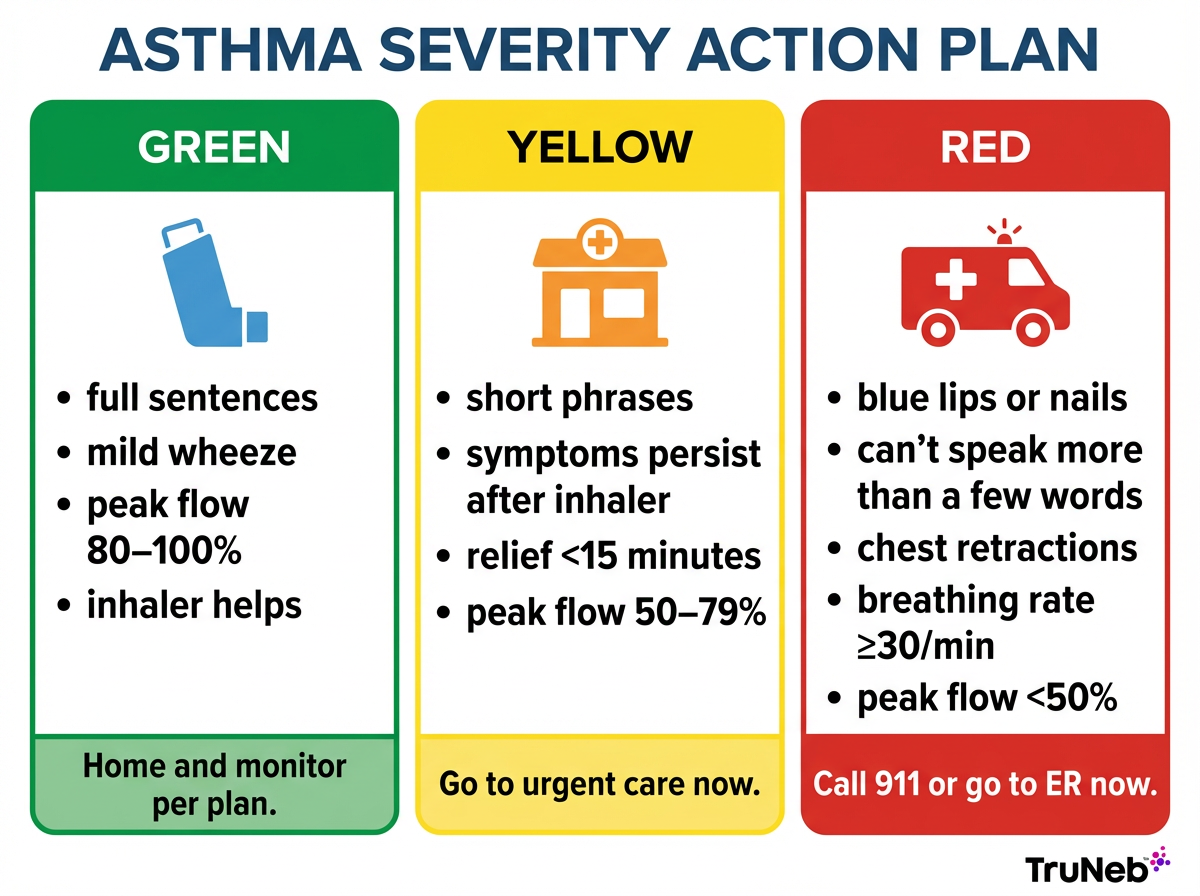
Here’s a simple way to decide fast during an asthma flare. If you're trying to decide when to go to urgent care for asthma, think in three zones.
This is the same stoplight system most asthma action plans use.
Green Zone: Manage at Home
- You can speak in full sentences.
- Mild wheeze, chest tightness, or cough.
- Peak flow is about 80% to 100% of your personal best on your peak flow meter.
- Your rescue inhaler helps and relief lasts.
- Follow your action plan and keep monitoring.
Yellow Zone: Go to Urgent Care
- Wheeze, tightness, or cough keeps coming back after your inhaler.
- Speaking is harder. You use short phrases.
- Breathing feels like work and you feel short of breath. Nostrils can flare. Walking at a normal pace is difficult.
- Peak flow is about 50% to 79% of your personal best on your peak flow meter.
- If you need repeat rescue doses without lasting relief, go to urgent care now. They can treat a moderate attack before it turns severe.
Red Zone: Call 911 or Go to the ER Now
- Blue or gray lips or nails.
- You can't speak more than a few words.
- Breathing rate is very fast, around 30 or more breaths per minute.
- Skin pulls in between ribs or at the base of the neck with each breath.
- You feel faint, confused, or very agitated.
- Your inhaler is not helping or you have a silent chest with little to no air movement.
- This can be life-threatening. A severe, unrelenting attack that does not improve with initial treatment is called status asthmaticus. Call 911.
⚠️ If you have blue or gray lips or nails, can't speak more than a few words, or feel faint or confused, treat it as an emergency. Call 911 right away.
If you're unsure, choose the safer option. It's better to get checked early than to wait too long.
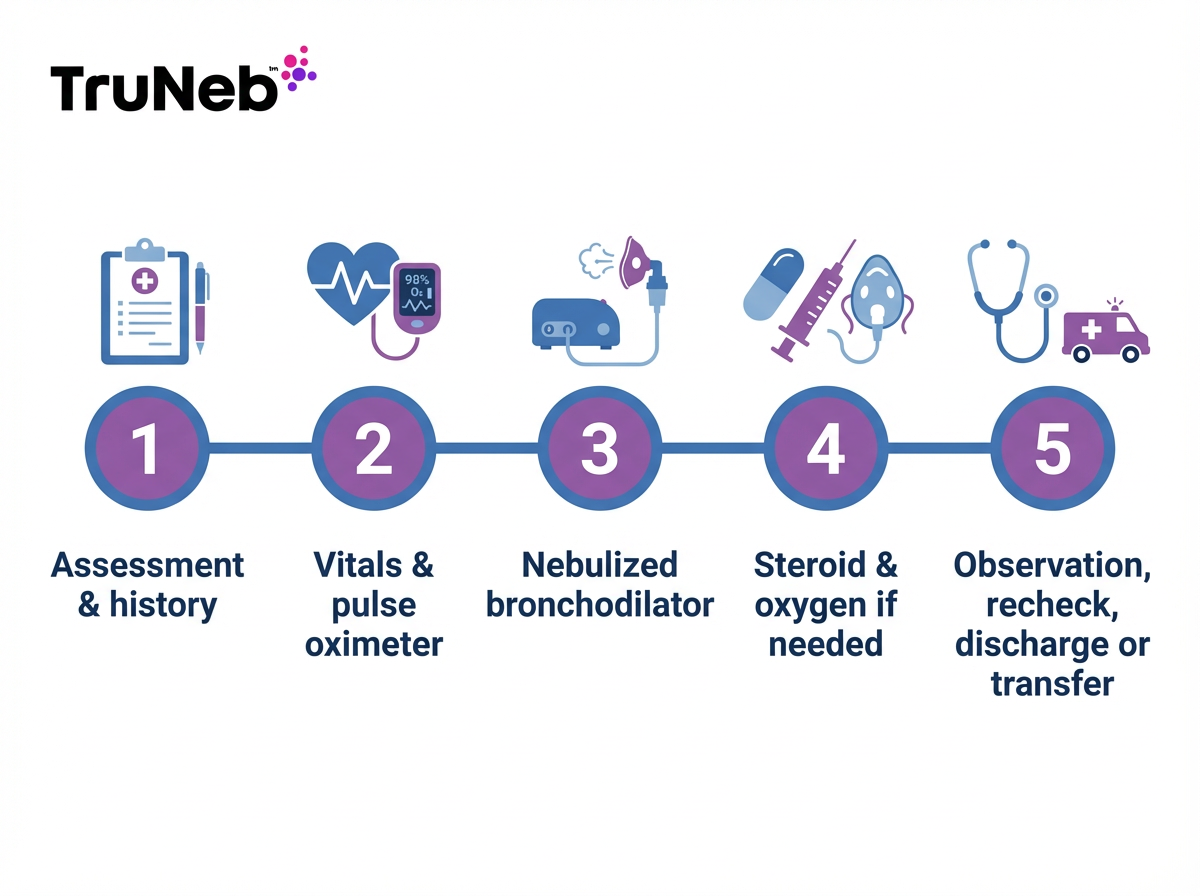
Once you've decided you're in the Yellow Zone, here's what to expect when you walk into urgent care.
Takeaway: Use a simple green–yellow–red system based on your symptoms and peak flow to decide whether to stay home, go to urgent care, or call 911 for an asthma attack.
What to Expect at Urgent Care During an Asthma Attack
Urgent care clinics treat mild to moderate asthma attacks every day. Here’s what usually happens.
Assessment
- A doctor or nurse asks about your symptoms, triggers, and what you’ve already tried.
- They listen to your lungs and check how well you can talk and move.
Vitals and Monitoring
- They check your oxygen level with a pulse oximeter (a small clip on your finger), heart rate, breathing rate, and blood pressure.
- They can measure your peak flow with a peak flow meter to gauge severity.
Breathing Treatment and Medicines
- You’ll likely get a nebulized bronchodilator (often albuterol) to relax tight airways.
- If needed, they give a steroid by mouth or injection to calm airway swelling.
- If oxygen is low, they add oxygen through a mask or nasal tube.
- If there’s a strong allergic reaction, they might also give an epinephrine shot.
Recheck and Next Steps
- Staff watch you for a short time, then recheck lungs and oxygen.
- If you improve, you can usually go home with instructions. They can prescribe refills for a rescue inhaler or a short steroid course when appropriate.
- If you don’t improve or start to feel worse, they arrange transfer to an ER. Urgent care clinics do not have ICU-level support or breathing machines (intubation and mechanical ventilation), so they transfer you if you need more advanced emergency care.
Key takeaway: Use urgent care for moderate symptoms that aren’t easing; go to the ER or call 911 for red-zone signs.
| Setting | Best for | Common treatments | Not available | When to choose |
|---|---|---|---|---|
| Urgent care | Yellow-zone symptoms: wheeze, tightness, shortness of breath that returns after inhaler; peak flow about 50–79%. | Nebulized bronchodilator, oral/IM steroid, oxygen, monitoring, prescriptions. | ICU care, intubation, mechanical ventilation, advanced imaging. | When symptoms aren’t severe but aren’t resolving with your action plan. |
| ER/911 | Red-zone signs: blue/gray lips or nails, can’t speak in full sentences, very fast breathing, confusion, “silent chest,” peak flow under 50%. | All urgent-care treatments plus advanced emergency care and continuous monitoring. | — | When severe signs are present or symptoms are rapidly worsening. Call 911. |
Note: Availability can vary by location. If in doubt, choose emergency care.
Urgent care can quickly assess your breathing, give you a nebulizer treatment and other medicines, and decide whether it’s safe for you to go home or if you need the ER.
Immediate Actions During an Asthma Flare
Start your quick-relief plan right away.
- Use your rescue inhaler exactly as your asthma action plan and doctor direct—don’t change doses based on advice you read online. If you have a spacer, use it to get more medicine into your lungs.
- Sit upright or lean slightly forward. Don't lie down. Take slow, steady breaths and try to stay calm.
- Get away from triggers like smoke, dust, or cold air.
- If your asthma action plan includes a home nebulizer treatment your doctor prescribed, follow that step while you’re arranging urgent care or 911. A handheld device can deliver your prescribed nebulized medication at home or on the way to care.
- Recheck after treatment. When relief is brief or symptoms keep coming back, go to urgent care.
- If severe signs appear (blue lips, gasping, confusion, chest retractions), call 911.
- Severe allergic reactions (anaphylaxis) can look similar, especially if there is swelling of the lips or face or a widespread rash along with trouble breathing. Treat this as a 911 emergency.
- Avoid lookalikes: products labeled "steam inhaler" are not for asthma medicines and shouldn’t replace a nebulizer.
Takeaway: During an asthma flare, follow your action plan by using your quick-relief inhaler or nebulizer as prescribed, sitting upright, avoiding triggers, and getting urgent or emergency care if symptoms don't ease quickly.
Safety note: Talk to your doctor before trying a new medication.
Important: Hypertonic saline (3 percent or 7 percent) can help with mucus in some lung conditions, but it isn’t a standard treatment for asthma attacks and should only be used if your doctor includes it in your written plan.
Staying Safe and Prepared with an Asthma Action Plan
A written Asthma Action Plan gives you clear steps before things get serious. If you don't have one yet, ask your doctor to create an Asthma Action Plan with you.
- Know your zones. Many plans use peak flow cutoffs: Green 80 to 100 percent of personal best, Yellow 50 to 79 percent, Red below 50 percent.
- Track your peak flow with a peak flow meter. Check during symptoms or daily if your doctor recommends it.
- Control triggers. Smoke, pollen, dust mites, mold, cold air, and infections can set off flares. Reduce exposure and keep up with vaccines like the flu shot.
- Take controller medicines exactly as prescribed. Good daily control means fewer emergencies.
- Keep tools ready. Portable nebulizers can make it easier to follow your Yellow Zone steps at home or on the go. TruNeb also offers 3 percent and 7 percent saline for mucus clearance in certain lung conditions. For asthma, only use saline if your doctor includes it in your plan.
- Always follow up after any urgent care or ER visit. Your doctor or asthma specialist (such as an allergist or pulmonologist) might update your plan or adjust medications so the next flare is easier to manage.
Takeaway: An asthma action plan turns your symptoms and peak flow readings into clear green, yellow, and red steps so you know exactly when to treat at home, go to urgent care, or call 911.
Remember, don't delay emergency care when you have red-zone signs. Emergency departments are required to treat true emergencies.
Frequently Asked Questions about Urgent Care for Asthma
These quick questions and answers explain when urgent care is enough for an asthma attack and when you should head straight to the ER or call 911. Tap or click a question below to see the answer:
Use severity to decide. Yellow-zone symptoms are usually right for urgent care. Red-zone signs like blue or gray lips or nails, severe shortness of breath, confusion, or not being able to speak in full sentences are 911/ER emergencies.
Yes. Urgent care clinics treat mild to moderate attacks with nebulized bronchodilators, steroids, oxygen, and monitoring. Severe attacks are transferred to an ER.
Don’t wait—go to urgent care or the ER. Try to stay calm and upright while you get there. If you have a nebulizer and solution your doctor prescribed for attacks, you can use it while you’re on the way for care—don’t let it delay getting seen.
Yes. They can give a nebulizer treatment on the spot and prescribe inhalers or a short steroid course when needed.
Only if symptoms are mild to moderate and you feel in control. If you feel faint or have red-zone signs, ⚠️ don’t drive—call 911.
Many urgent cares aren’t open overnight. For more than mild symptoms, go to the ER. If symptoms are mild, follow your action plan and seek care as soon as you can.
Take controller medications exactly as prescribed, avoid triggers, use your peak flow meter and action plan to spot early changes, and schedule regular check-ins with your doctor or an asthma specialist.
Always check with your doctor before adding or changing any asthma medicine.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms and treatment options, and seek emergency care right away if you have severe breathing problems.