On this page

Traveling with Lung Conditions: Common Fears and Real Risks
Yes, you can travel with asthma, COPD, bronchiectasis, cystic fibrosis, or interstitial lung disease (including pulmonary fibrosis) if your condition is stable. Good planning makes the biggest difference to how you feel when you travel.
Airplane cabins feel like high altitude. Oxygen drops a bit, so you can feel more short of breath. With medical clearance and a simple plan, most people fly safely.
If you had a recent flare, infection, or hospital stay, ask your doctor about timing. You might need extra steps, like in‑flight oxygen, or to wait until you recover. If your doctor says your lung condition isn’t stable yet, it’s safer to postpone your trip.
These travel tips for people with respiratory conditions help you plan safely without giving up trips you love.
Medical disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk to your doctor about your symptoms, travel plans, and any changes to your medications or oxygen.
Takeaway: Most people with stable lung disease can travel safely with planning and medical clearance.
Before You Travel: Medical Checkup and Clearance
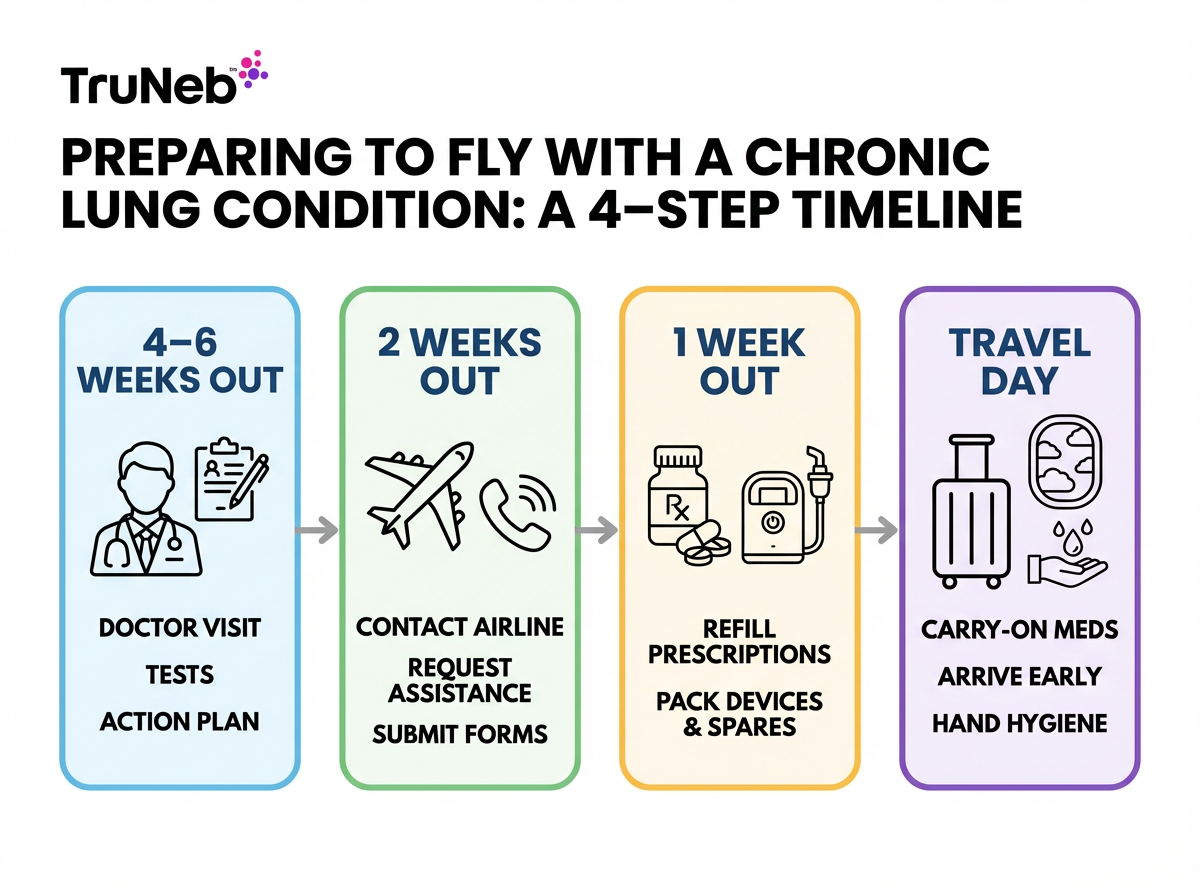
Book an appointment 4–6 weeks before your trip. If your trip is last‑minute, still call your doctor as soon as you can.
- Share your route, flight lengths, destination altitude, and activity plans.
- Confirm you're fit to travel. Your doctor can check lung function or walking tolerance.
- Ask about a fit‑to‑fly test if your oxygen runs low. This test simulates airplane cabin oxygen levels and shows whether you'll need oxygen on the plane.
- Update vaccines: flu, COVID‑19, and pneumococcal.
- Get a written Asthma or COPD Action Plan with clear steps.
- Ask if you should carry “just in case” meds like an antibiotic or a short steroid course.
- See your clinician 4–6 weeks before departure to confirm you are fit to travel.
- Ask about a hypoxic challenge (fit‑to‑fly) test if you have moderate to severe disease or borderline oxygen levels (European Lung Foundation).
- Update influenza, COVID‑19, and pneumococcal vaccines before you go (CDC).
Safety note: Talk to your doctor before trying a new medication or adjusting oxygen.
Takeaway: See your doctor early to confirm fitness to travel and update your action plan.
Travel Documents, Letters, and Insurance
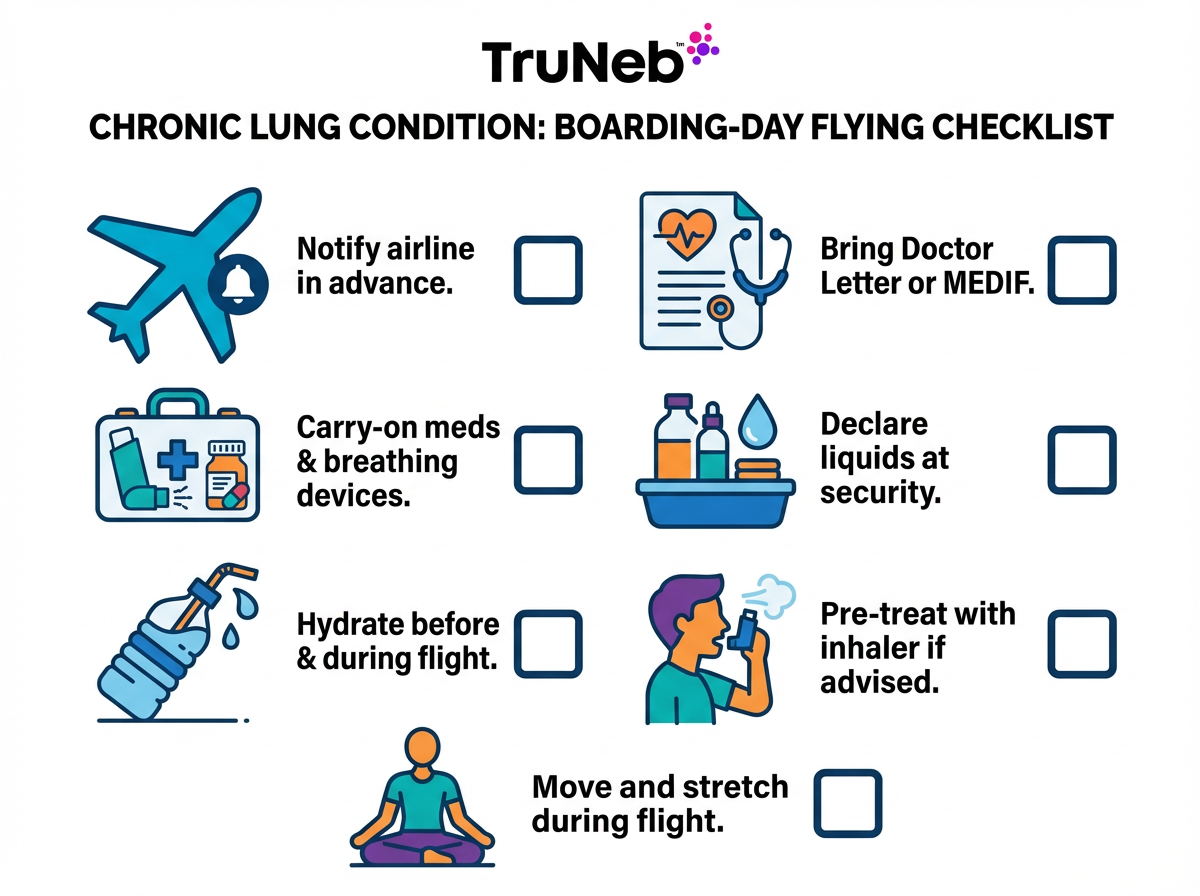
The right paperwork keeps your trip running smoothly.
- Doctor’s letter listing your condition, medicines, and devices. Note that they are medically necessary.
- Copies of prescriptions and a current medication list.
- Travel insurance that covers pre‑existing conditions and emergency care.
- Contact info for your doctor and a clinic or hospital at your destination, and the local emergency number (the country’s equivalent of 911).
- Airline forms (MEDIF) if required.
- Medical ID bracelet or wallet card that lists your lung condition and medicine allergies.
Store these with your passport so you can reach them quickly.
Takeaway: A doctor’s letter, a meds list, and pre‑existing condition coverage remove most travel friction for people with lung conditions.
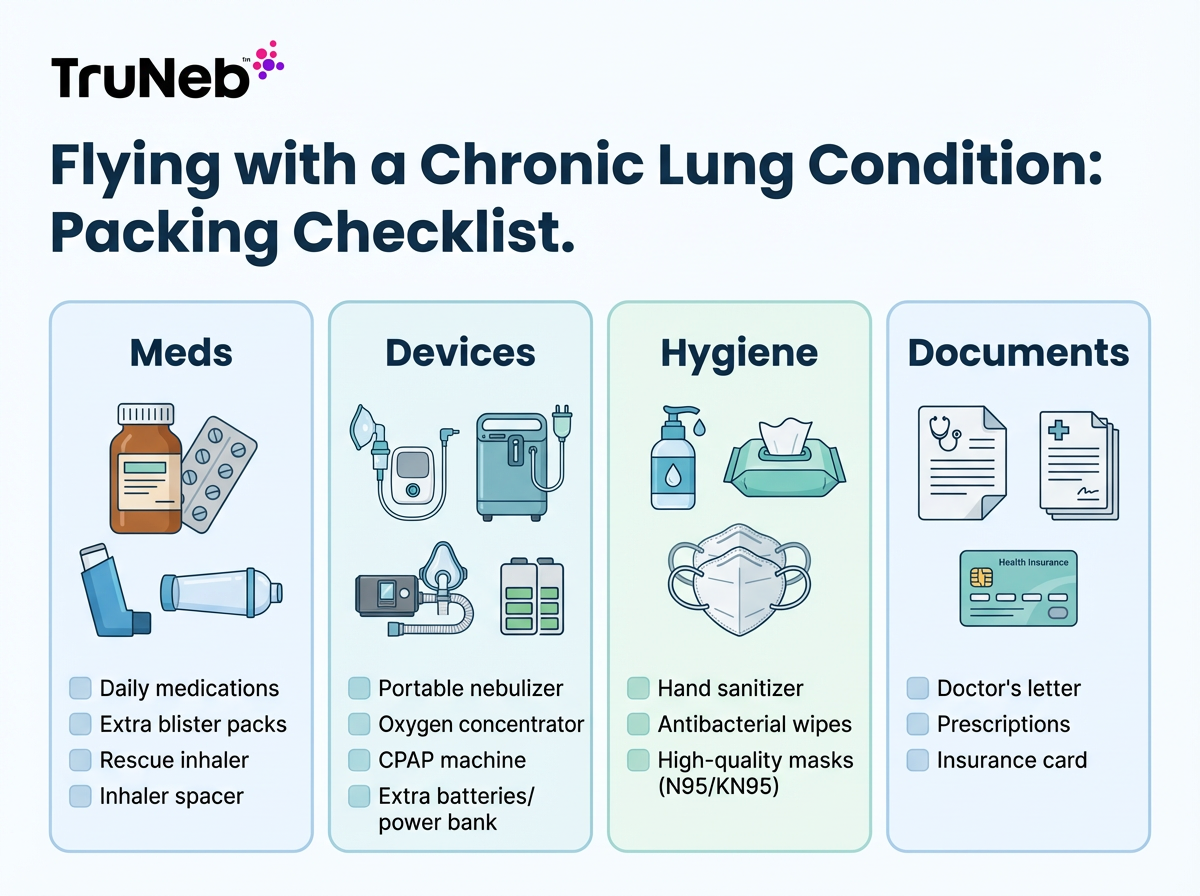
Packing Checklist for Healthy Travel
Put all critical items in your carry‑on. Never put essential medications or devices in checked bags, in case they're lost or delayed.
Medications and supplies:
- Daily medicines plus extra doses in original labeled bottles
- Rescue and controller inhalers
- Spacer, if you use one
- Portable nebulizer, mask or mouthpiece, tubing, charger, and unit‑dose vials
- Spare parts for your devices (extra nebulizer mouthpiece or mesh, extra tubing) if you rely on them daily
- Portable oxygen concentrator with spare cannulas and batteries, if you use oxygen
- CPAP or BiPAP with power adapter (for sleep apnea)
- Pulse oximeter or peak flow meter (optional)
Hygiene and comfort:
- Hand sanitizer and disinfecting wipes
- Quality masks for crowds or poor air quality
- Saline nasal spray, tissues, scarf for cold air
- Water bottle
Documents:
- Doctor’s letter, prescription copies, insurance info, action plan
Takeaway: Keep all essential meds and devices in your carry‑on so a lost bag isn't a health risk.
Choosing and Using Portable Respiratory Equipment
Nebulizers:
- Pick a small, quiet, battery‑powered mesh model.
- USB charging helps on the go.
- If your doctor prescribes saline therapy, 3% or 7% unit‑dose hypertonic saline vials are easy to pack and travel‑friendly.
Example: The TruNeb™ Portable Mesh Nebulizer is pocket‑sized and quiet. It runs on batteries and can make treatments easier during layovers or at the hotel.
Oxygen:
- If you use oxygen, ask your doctor about settings for flights or altitude.
- Airlines generally do not allow personal oxygen tanks on board; they usually require an approved portable oxygen concentrator instead.
- Check with your airline that your portable oxygen concentrator model is approved for in‑flight use.
- Portable oxygen concentrators are typically allowed on planes. Bring extra charged batteries.
- Don't change your oxygen settings on your own; only adjust them if your doctor has told you how.
Power and backups:
- Pack chargers, adapters, and a spare mask or mesh part if your device uses one.
- If you use CPAP or BiPAP, keep it in your carry‑on and ask your airline how to plug it in on overnight flights.
Caution: Ask your doctor before adding hypertonic saline or changing your schedule.
Takeaway: A compact, battery‑powered mesh nebulizer keeps your breathing treatments easy anywhere.
Air Travel with a Respiratory Condition
Before the flight:
- Tell the airline about oxygen or special assistance as early as possible. Many ask for at least 48 hours notice.
- Ask if a medical form or doctor’s letter is needed.
- Arrive early so you aren't rushed. Request wheelchair help if long walks are hard.
Security:
- Nebulizers, CPAPs, and medicines are allowed. Tell the agent you have medical devices. Keep liquid meds together and declare them. Liquid medicines for your nebulizer are allowed in larger amounts if you declare them as medical.
During the flight:
- Drink water. Cabin air is dry. Saline nasal spray can help.
- Avoid drinking a lot of alcohol or taking sedating medications without your doctor’s advice; they can slow breathing and make you feel worse in the air.
- Use your reliever inhaler as directed. Some people pre‑treat before takeoff or landing if advised.
- If you use a POC, follow your prescribed setting and watch battery life.
- Move legs and stretch on longer flights to keep circulation.
- If you feel much more short of breath than usual, use your rescue inhaler as your doctor directed and tell the cabin crew early so they can help.
Why planes feel different:
- On a plane, cabin pressure is like being at 6,000–8,000 feet. Oxygen levels are lower than at sea level.
Takeaway: Inform the airline early, carry all meds, and plan for dry air and lower cabin oxygen.
Tips for Road Trips, Cruises, and Trains
Road trips:
- Stop every two hours to stretch, breathe, and hydrate.
- Keep the cabin smoke‑free. Skip strong scents.
- Secure oxygen gear. Don't leave meds or tanks in a hot car.
- If climbing to altitude, take it slow and rest at mid‑points.
Cruises and trains:
- Tell the cruise line or rail operator if you'll bring a POC. Pack extra supplies you can't replace at sea.
- Know where the ship’s or train’s medical center is located and what hours it's staffed.
- Avoid smoking areas on ships. Use elevators on large vessels.
- Practice hand hygiene in crowded areas.
Takeaway: Build in breaks, keep clean air, and carry spares you can't buy on the road.
Plan Your Destination for Altitude, Weather, and Triggers
Altitude:
- Higher places have less oxygen. Go easy the first one to two days. Use oxygen if prescribed. Ask your doctor if you need to adjust your oxygen at higher altitudes. Watch for headache or unusual fatigue.
Cold weather:
- Cold, dry air can tighten airways. Cover your nose and mouth with a scarf or mask. Ask if pre‑treating with a reliever is right for you.
Heat, humidity, and pollution:
- Plan outdoor time for mornings or evenings. Check air quality and pollen. Choose smoke‑free, pet‑free lodging. Avoid strong scents.
- Plan an easy first 1–2 days at altitude and discuss oxygen needs with your clinician (European Lung Foundation).
- Cold, dry air can trigger bronchospasm; cover your nose and mouth and consider pre‑treating if advised (CDC).
- Check local air quality and pollen and schedule indoor time on high‑AQI days (CDC).
Takeaway: Check altitude and air quality so you can plan around triggers.
Stick to Your Treatment Plan on the Road
Time zones and busy days can shift your schedule. Use phone alarms so you don't miss doses. If you're crossing several time zones, ask your doctor or pharmacist how to adjust your medicine times before you leave.
Daily rhythm:
- Do morning treatments before you head out.
- Schedule rest between activities.
- Tell travel partners you need 20–30 minutes for treatments.
Health basics:
- Hydrate, eat on time, and sleep enough to keep your lungs steady.
Takeaway: Use alarms and a simple plan so time zones don't cause missed doses.
Be Ready for Emergencies
Have a backup plan:
- Know the nearest clinic or hospital and how to call for help at your destination.
- Keep your rescue inhaler on you, not in a bag.
- Use your action plan early if your symptoms start creeping up. If your rescue medicine doesn't help, get medical care right away.
- Carry any “just in case” meds your doctor provided and follow your plan.
- Keep your travel insurance hotline number handy.
⚠️ If you have severe trouble breathing, can't speak in full sentences, notice blue lips or fingertips, or feel confused, seek emergency medical care right away or call the local emergency number.
Medical disclaimer: Never start, stop, or change prescription treatments without your doctor's guidance.
Takeaway: Act early with your plan and get help fast if your breathing symptoms do not ease.
Travel Confidently and Breathe Easy
Good planning turns worry into a smooth trip. Check in with your doctor, pack your essentials, arrange airline help, and pace your days. With the right gear and a clear plan, your lungs can go wherever you go.
Takeaway: Good preparation turns a risky trip into a regular trip for your lungs.
Frequently Asked Questions
Tap or click a question below to see the answer:
Yes. Most people with well-controlled COPD or asthma can fly safely. See your doctor first. Some need a fit-to-fly assessment to decide on in-flight oxygen. Bring your inhalers, follow your action plan, and inform the airline if you need assistance or a portable oxygen concentrator.
Yes. Nebulizers and CPAP machines are allowed. Tell the agent you have medical devices. Keep liquid medicines together and declare them. Medical liquids can exceed standard liquid limits when declared. Always carry these items on the plane rather than checking them.
Carry a doctor's letter listing your diagnosis, medicines, and any devices you need. Ask your airline about a medical form (MEDIF). Keep copies of prescriptions and your medication list in your carry-on.
Stop and use your rescue inhaler or prescribed treatment right away. Follow your action plan. If symptoms don't improve or you feel worse, call the local emergency number or go to the nearest emergency department. On a plane, alert the crew early. They can assist and access emergency oxygen for acute events.
Yes. Thin air at altitude can lower oxygen levels and increase shortness of breath. Ascend gradually, take it easy the first days, and use supplemental oxygen if prescribed. Ask your doctor how to adjust your plan for altitude.
It's smart to buy a policy that covers pre-existing conditions. Declare your condition so emergencies related to your lungs are covered. Keep the insurer's emergency number with you.
Wash hands often, use sanitizer in crowded places, wear a quality mask in tight indoor spaces, and stay up to date on flu and COVID-19 vaccines. Avoid smoke and people who are clearly ill.