On this page
You're recovering from COVID-19, and now a cough or low fever crept back. Worried about walking pneumonia after COVID? This guide will help you recognize symptoms, know when to see a doctor, and understand treatment and recovery.
How a COVID-19 Infection Can Lead to Walking Pneumonia
COVID-19 can leave your airways irritated. As you start to feel better, your defenses can still be low. That makes it easier for bacteria like Mycoplasma pneumoniae to move in. This is called a secondary bacterial pneumonia. When this infection stays mild, doctors call it an atypical pneumonia—many people know it as walking pneumonia. In people recovering from COVID, this can show up as post-COVID pneumonia that is on the mild side, meaning walking pneumonia after COVID. It usually shows up 1–3 weeks after the first COVID symptoms, with cough and low fever coming back. Not every secondary pneumonia is mild; some become serious. Here, we focus on the milder "walking" pattern.
Bottom line: COVID can open the door, and bacteria can step in and cause a mild pneumonia during recovery.
Key Symptoms — Normal COVID Recovery vs Walking Pneumonia
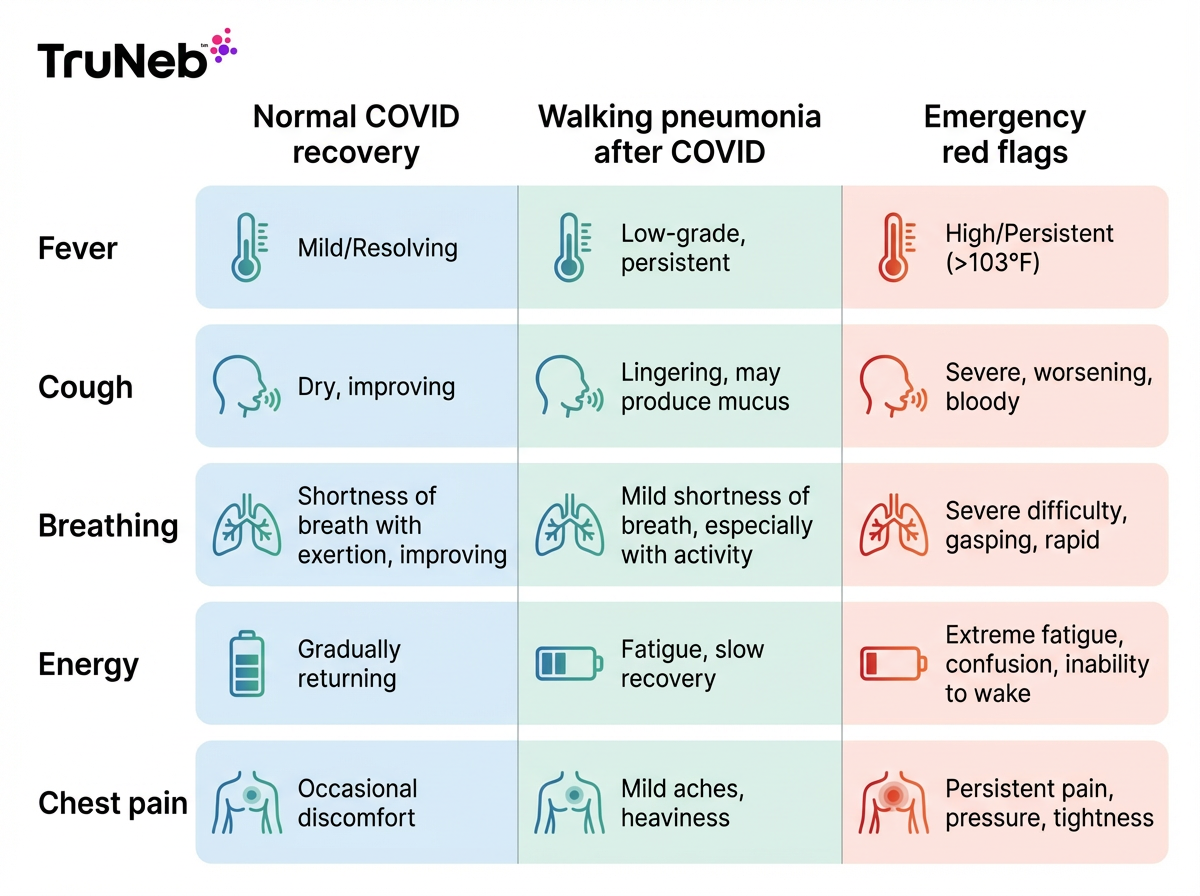
After COVID, normal recovery means symptoms ease week by week. Walking pneumonia looks different.
Fever: In normal recovery, fever fades and stays away. With walking pneumonia, a low fever, usually under 101°F, returns or lingers after a few better days.
Cough: In normal recovery, cough gets a little better each week. With walking pneumonia, cough holds steady or gets harsher. It can start dry and later bring up a small amount of mucus.
Breathing: In normal recovery, breathlessness steadily improves. With walking pneumonia, you notice shortness of breath on mild activity that wasn’t there a few days ago.
Energy: In normal recovery, energy comes back. With walking pneumonia, you feel drained again.
Chest discomfort: Normal recovery can leave a scratchy throat from coughing. Walking pneumonia can cause a sharp, small pain when you take a deep breath or cough.
Nasal clues: Heavy stuffy nose or loss of smell is not typical for pneumonia; those fit more with a cold, flu, or leftover viral symptoms.
In adults, symptoms of walking pneumonia include a returning or persistent low-grade fever, a cough that stays the same or worsens (sometimes with a little mucus), mild shortness of breath with light activity, new or renewed fatigue, and a small, sharp pain with deep breaths or coughing. Here are the main symptoms of walking pneumonia after COVID.
These are milder than classic COVID pneumonia symptoms, which usually include higher fever, rapidly worsening shortness of breath, and sometimes low oxygen levels. Walking pneumonia is a milder form of pneumonia—you can still be up and moving, unlike many cases of typical pneumonia.
In short, normal recovery gets steadily better, while walking pneumonia brings back or worsens fever, cough, and shortness of breath.
Long COVID or Lingering Cough? Distinguishing Pneumonia from Other Post-COVID Issues
A lasting cough and fatigue after COVID can mean different things. Long COVID lasts beyond 4 weeks and typically does not bring a new fever or new changes on a chest X-ray. Walking pneumonia is an active infection, so it commonly brings a returning low fever, chest discomfort, and X-ray changes.
Walking pneumonia vs long COVID: walking pneumonia brings signs of a fresh infection (new low fever, changes on a chest X-ray), while long COVID usually does not.
A post-viral bronchitis can also mimic pneumonia. Bronchitis causes a nagging cough and sometimes wheeze, but fever is uncommon and a chest X-ray is clear. If your cough is the only symptom and you slowly improve with inhalers, it's more likely bronchitis or a reactive airway flare.
Walking pneumonia vs bronchitis: bronchitis mainly affects the airways and causes a long cough, usually without a fever or lung changes on X-ray.
When in doubt, see your doctor. A quick exam and, if needed, an X-ray can separate normal recovery, long COVID, bronchitis, and walking pneumonia.
Bottom line: Pneumonia brings new infection signs like fever or X-ray changes; long COVID usually does not.
Getting Diagnosed — Don’t Guess, Confirm With Your Doctor
A short visit can usually give you a clear answer. Your doctor will check your temperature, breathing rate, and oxygen. They will listen for crackles or other changes in your lungs. A chest X-ray is a quick, common way to help confirm pneumonia, even in mild cases.
Some clinics run a nose or throat swab to look for Mycoplasma pneumoniae as part of a respiratory panel. In practice, if your exam and imaging fit, treatment starts without waiting for every test. Some very mild cases can be diagnosed based on symptoms and an exam, especially in children.
Key point: A chest X-ray is a fast, reliable tool doctors use to help diagnose walking pneumonia.
Treatment for Walking Pneumonia and Recovering Safely at Home
Walking pneumonia treatment usually includes antibiotics. Doctors usually treat walking pneumonia with antibiotics. A common choice is azithromycin. Most people feel better in a few days, but it’s important to finish the full course.
Home care helps. Rest more than you think you need. Drink fluids to thin mucus. Use fever reducers if your doctor says they’re safe for you. Warm liquids can soothe your throat and ease coughing.
To help stubborn mucus, some doctors use inhaled therapy. A portable mesh nebulizer such as the TruNeb™ device can deliver a fine saline mist directly to your airways. With your doctor’s guidance, 3% or 7% hypertonic saline can help draw moisture into the airways so mucus loosens and clears more easily. This supports comfort and airway clearance. It does not replace antibiotics when they are prescribed.
Don’t swap in a steam inhaler or humidifier for a nebulizer—they warm and moisten the air but don’t deliver medicines or saline into your lungs the same way.
Talk to your doctor before trying a new medication or nebulized saline. If you are not improving within 48–72 hours, or if you feel worse at any point, check back with your doctor.
Bottom line: Antibiotics treat the infection; nebulized saline, rest, and fluids can help you breathe easier while you heal.
When To Seek Emergency Care (Red Flag Symptoms)
⚠️ Go to the emergency room or call 911 (or your local emergency number) right away for any of the following:
- Trouble breathing at rest or speaking in full sentences
- High fever of 102°F or higher that won’t come down
- Blue lips or face
- Severe chest pain, or pain that gets worse fast
- Confusion, fainting, or severe dizziness
- In children: ribs pulling in with each breath, very high fever, or unusual sleepiness
If your cough is getting worse or you have a new low fever but you can breathe comfortably, arrange a same-day or next-day visit with your doctor.
Bottom line: If breathing is hard, fever is high, or lips look blue, go to the ER.
Frequently Asked Questions
Tap or click a question below to see the answer:
Suspect walking pneumonia if symptoms return or worsen after early improvement: a low fever comes back, your cough gets harsher instead of easing, or you feel more short of breath on mild activity. The only sure way to know is a checkup with your doctor, often with a chest X-ray.
Post-viral bronchitis and long COVID can look similar. Bronchitis brings a long cough, usually without a fever, and a clear chest X-ray. Long COVID lasts beyond 4 weeks and typically lacks new fever or X-ray changes. An exam helps sort these out.
Yes. Mycoplasma pneumoniae spreads in droplets when you cough or sneeze. Cover your cough, wash hands, and consider masking around others for a few days after starting treatment or as your doctor advises.
Most people feel better 3–5 days after starting antibiotics, but the cough and tiredness can last 2–4 weeks. Follow up if you are not improving in 48–72 hours or as your doctor advises.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms, questions, or before starting or changing any treatment.