On this page
Here’s the simple truth: a metered-dose inhaler (MDI) with a spacer can work just as well as a nebulizer for most people with asthma when used correctly.
An inhaler with a spacer is fast and portable; a nebulizer is slower but lets you breathe normally. If you’re comparing nebulizer vs inhaler with spacer, think speed and portability versus ease during difficult breathing.
How Each Device Works
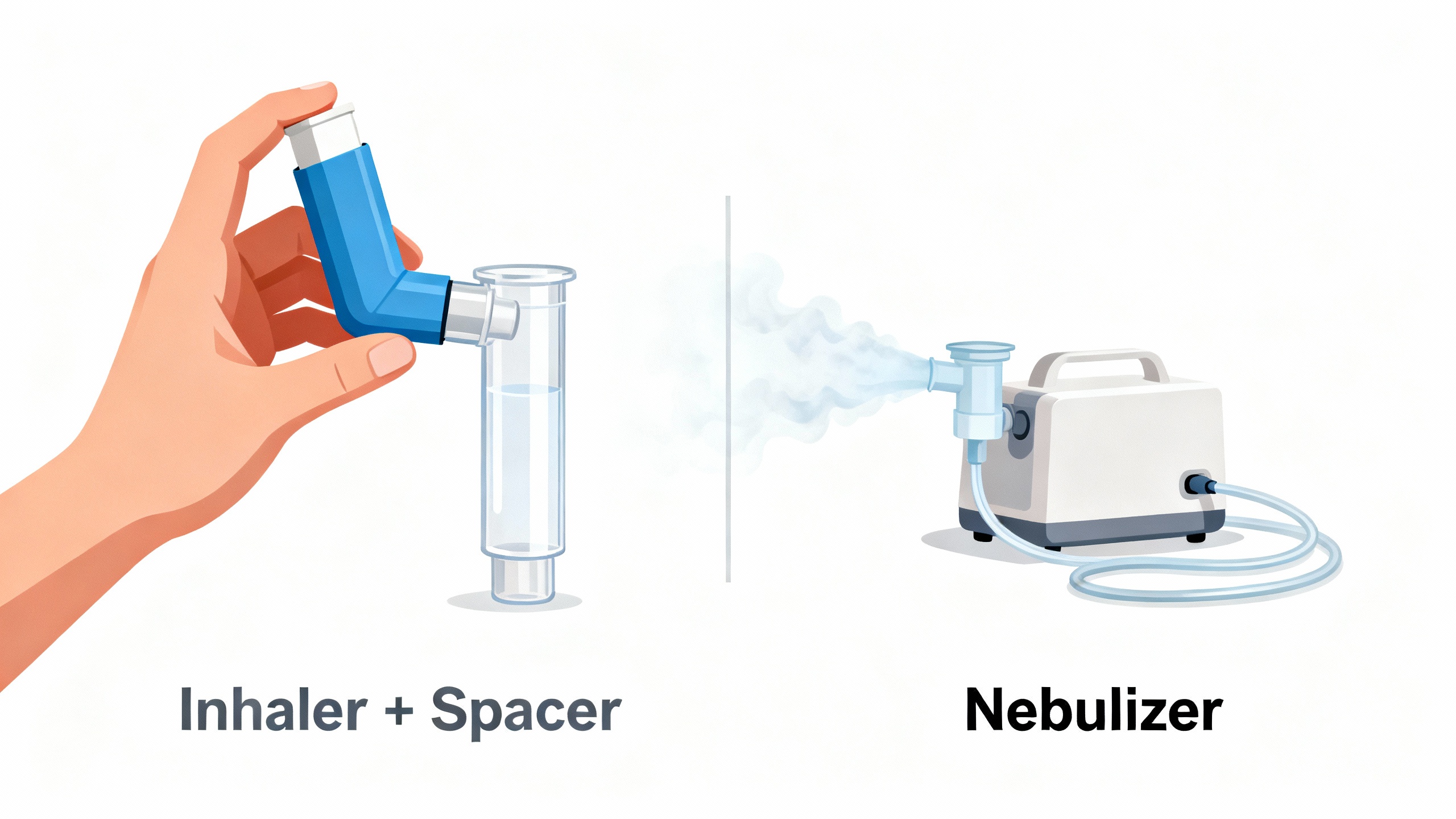
- Spacer (holding chamber): A plastic tube that attaches to an MDI. You press the inhaler, the medicine sits in the chamber, and you breathe it in slowly through a mouthpiece or mask. The spacer doesn’t create mist. The inhaler does, and the spacer holds it so you can inhale slowly.
- Nebulizer: A small machine that turns liquid medicine into a mist you breathe in through a mask or mouthpiece over several minutes.
The difference: a spacer helps an inhaler deliver quick puffs effectively, while a nebulizer delivers a steady mist over time.
A spacer attaches to an inhaler to hold and slow the spray, while a nebulizer is a separate machine that turns liquid medicine into a steady mist.
A spacer is a holding chamber used with a metered-dose inhaler; a nebulizer is a separate machine that makes a continuous mist.Time: spacer doses take seconds; nebulizer treatments usually take 5–10 minutes.Technique: spacer needs slow, deep breaths and a good seal; nebulizers use normal breathing.Both can deliver rescue bronchodilators effectively when used properly.
Do Spacers Work as Well as Nebulizers?
Short answer: yes.
When used correctly, an inhaler with a spacer can deliver relief comparable to a nebulizer.
What the research found: In children with acute asthma, MDI + spacer and nebulizer treatments led to similar improvements in breathing and similar chances of needing hospital care.
Why they’re comparable: Both methods get medicine into your airways. A spacer slows the spray so more medicine reaches the lungs. A nebulizer gives a continuous mist, which also reaches the lungs over time. Rescue medications (for example, albuterol) are delivered by both methods.
If inhaler technique is poor (no spacer, breathing too fast, bad seal), a nebulizer can seem better. Fixing technique or using a spacer often solves that.
When used correctly, an inhaler with a spacer can deliver relief comparable to a nebulizer.
Ease of Use and Daily Convenience
Key takeaway: a spacer is usually faster and easier to carry; a nebulizer is simpler to breathe with but takes more time.
- Time: Inhaler + spacer takes seconds per dose. A nebulizer often takes 5–10 minutes.
- Portability: A spacer and inhaler fit in a bag or pocket. A nebulizer needs power and has parts (machine, cup, tubing, mask).
- Technique: A spacer helps you breathe in slowly and get more medicine. A nebulizer requires normal breathing, which can help during a flare when timing is hard.
- Cleaning: Spacers need simple cleaning regularly. Nebulizer parts need cleaning after each use to reduce germ buildup.
Nebulizers need power (outlet or battery) and are less discreet in public settings.
If you want relief on the go, a spacer shines. If you need hands-off breathing during a hard flare, a nebulizer can help.
Bottom line: spacer for speed and portability, nebulizer for easier breathing during flares.
Spacer vs Nebulizer for Children
Bottom line for kids: Pediatric teams typically use spacers first because they’re fast and work well; nebulizers are helpful when a child can’t use an inhaler.
What works in real life:
- Spacers can attach to a soft face mask, so even toddlers can breathe the medicine in a few calm breaths.
- Nebulizers can help a young child who won’t cooperate with an inhaler or during an illness when breathing is shallow.
Evidence check: Studies in children show similar asthma relief with MDI + spacer compared to nebulizers when treatment is given correctly.
Parent tips:
- Make spacer time a game (count slow breaths, pretend it’s astronaut gear).
- During nebulizer time, use a calm routine (story, song, or show) to help them sit still.
For most kids who can use a mask and spacer, an inhaler + spacer is fast and effective; nebulizers help when cooperation or coordination isn’t possible.
Side-by-Side Comparison: Inhaler + Spacer vs Nebulizer
| Feature | Inhaler + Spacer | Nebulizer |
|---|---|---|
| How it delivers | Quick puffs into a holding chamber you inhale from | Continuous mist from machine over several minutes |
| Time per treatment | Seconds to about 1 minute | About 5–10 minutes |
| Portability | Pocket/bag friendly; no power needed | Bulky; needs outlet or battery |
| Technique needed | Slow, deep breaths with good seal | Breathe normally; less timing needed |
| Cleaning | Simple, regular cleaning | Clean parts after each use |
| Best for | Fast relief, school/work, travel | Young children who can’t use inhaler, tough flares |
This side-by-side view shows why a lot of people carry an inhaler with a spacer and keep a nebulizer at home as a backup.
At a glance, spacers prioritize speed and portability, while nebulizers trade speed for ease during difficult breathing.
Pros and Cons at a Glance
- Inhaler + Spacer Pros
- Fast: relief in seconds.
- Portable: no cord or power.
- Effective: similar symptom relief to nebulizers when used correctly.
- Inhaler + Spacer Cons
- Some technique needed: slow inhale and good seal.
- Extra piece: spacer adds one item to carry.
- Nebulizer Pros
- Easy breathing: just breathe normally.
- Good for little kids: or during distress.
- Nebulizer Cons
- Slow: 5–10 minutes per treatment.
- Less portable: needs power and parts.
- Less discreet in public: harder to use at school or work.
- More cleaning: after each use.
One-liner: choose speed and portability (spacer) or simplicity during a flare (nebulizer).
When to Use Which
Here’s a quick guide:
- For quick relief at school, work, or on the go, people typically use an inhaler with a spacer.
- For toddlers or anyone who can’t coordinate an inhaler, a nebulizer can be easier.
- Plenty of families keep both: spacer for daily use, nebulizer for tougher days.
Safety note: Follow your asthma action plan and ask your doctor to check your technique for whichever device you use.
Most people use an inhaler with a spacer day to day and keep a nebulizer as a backup for tougher times, based on their asthma plan.
Safety Reminder
- Device choice depends on age, coordination, and your action plan.
- Using either device the right way matters more than the device itself.
- Steam inhalers are NOT nebulizers and aren’t for prescription breathing medications.
- ⚠️ If you have severe symptoms such as trouble speaking, bluish lips or face, chest retractions, or symptoms that don’t improve with your quick-relief medicine, seek emergency care right away.
- Talk to your doctor before trying a new medication or changing how you take your current one.
- Ask your care team to watch your spacer or nebulizer technique once a year.
If symptoms are severe or rapidly worsening, treat it as an emergency and get help immediately.
Frequently Asked Questions
Tap or click a question below to see the answer:
Yes. When used correctly, an inhaler with a spacer is as effective as a nebulizer for most asthma medicines, including albuterol. Multiple studies show similar symptom relief and hospital outcomes.
If you can use an inhaler with a spacer, it can work as quickly as a nebulizer. If you are too short of breath to coordinate or need continuous delivery, a nebulizer may be easier. Follow your asthma action plan and seek emergency care if symptoms don’t improve.
Spacers with a mask work well for many children, even toddlers. Nebulizers help when a child cannot or will not use an inhaler or when breathing is shallow during illness.
Some people use both: an inhaler with a spacer for daily and on-the-go use, and a nebulizer at home for tougher episodes—based on their clinician’s advice and asthma action plan.
Yes. Mesh models are smaller and quieter than compressor units and can be convenient, but an inhaler with a spacer is still faster for quick relief.
Spacers and nebulizer machines are often sold without a prescription, but medications for both are prescription-only. Insurance coverage varies by plan.
Spacers typically cost less upfront ($10–$40). Nebulizer machines often cost $50–$100+ plus ongoing supplies. Medication costs and coverage differ by plan.