On this page

Silent asthma is when you have an asthma attack without obvious wheezing. Because it’s quiet, it’s easy to miss and can still become dangerous fast. In this guide, you’ll learn the subtle symptoms, how doctors diagnose it, what to do in the moment, and where tools like the TruNeb™ portable mesh nebulizer may fit into your plan.
Silent Asthma Attack Symptoms: What To Watch For
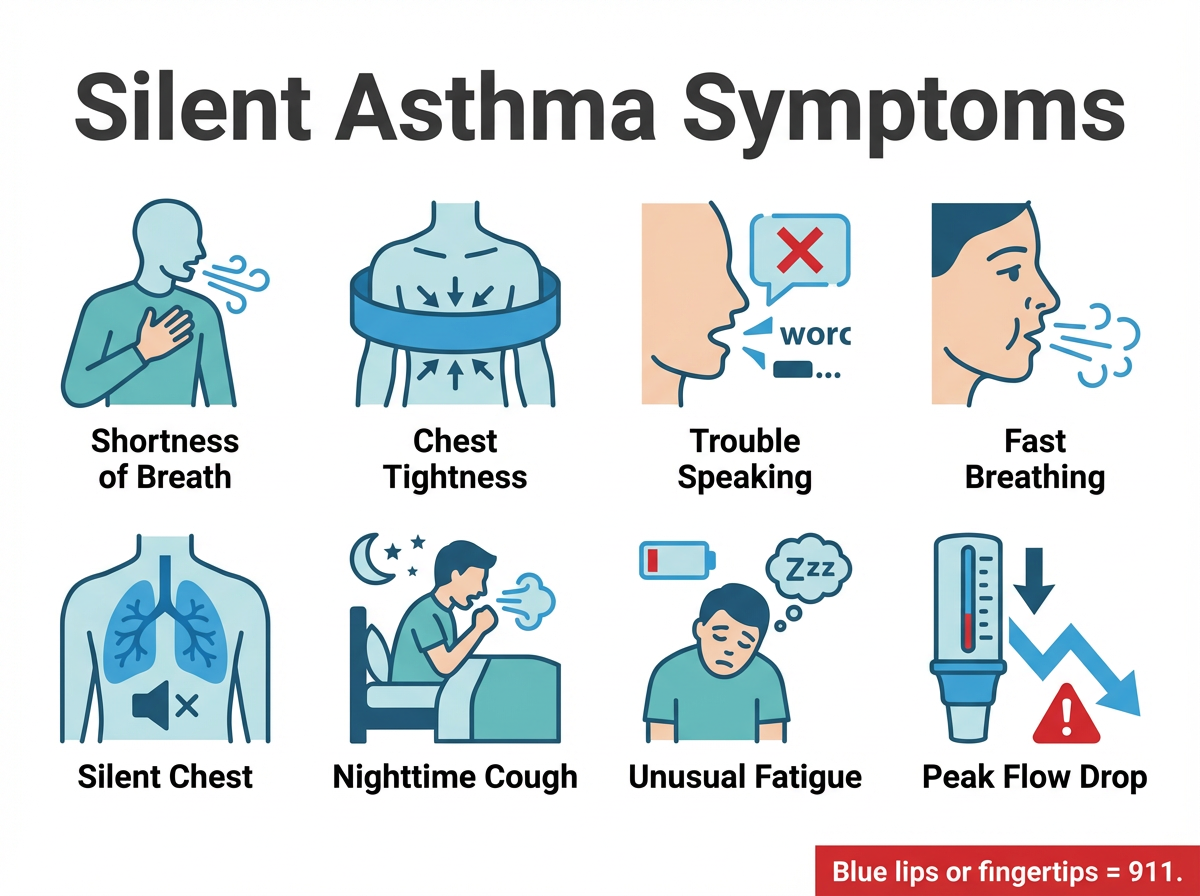
Silent asthma means you are having an asthma attack without the usual wheeze or obvious wheezing sounds (an asthma attack without wheezing). The signs are quiet but serious. Key silent asthma symptoms include:
- Shortness of breath (breathlessness) that feels out of proportion to the activity
- Chest tightness or pressure
- Trouble speaking in full sentences without stopping for air
- Fast, shallow breathing
- Quiet chest with little to no wheeze, sometimes called a silent chest
- Nighttime cough or waking up short of breath
- Unusual fatigue, restlessness, or anxiety
- Drop in peak flow compared with your personal best
- ⚠️ Blue or gray lips or fingertips are an emergency. Call 911.
Rule of thumb: If you have to pause mid-sentence for air, follow your action plan now.
Why Silent Asthma Is Dangerous
No wheeze does not mean mild. In some severe attacks, airflow drops so low you hear little to no sound. This silent chest is a red flag and needs urgent care. These hidden asthma signs can lead to delayed treatment and low oxygen.
Warning signs of danger include breathing faster and chest tightness that is getting worse. Trouble speaking more than a few words, using neck or belly muscles to breathe, confusion, or a blue tint to lips or nails are emergency signs. Start your action plan early. Do not wait for a loud wheeze.
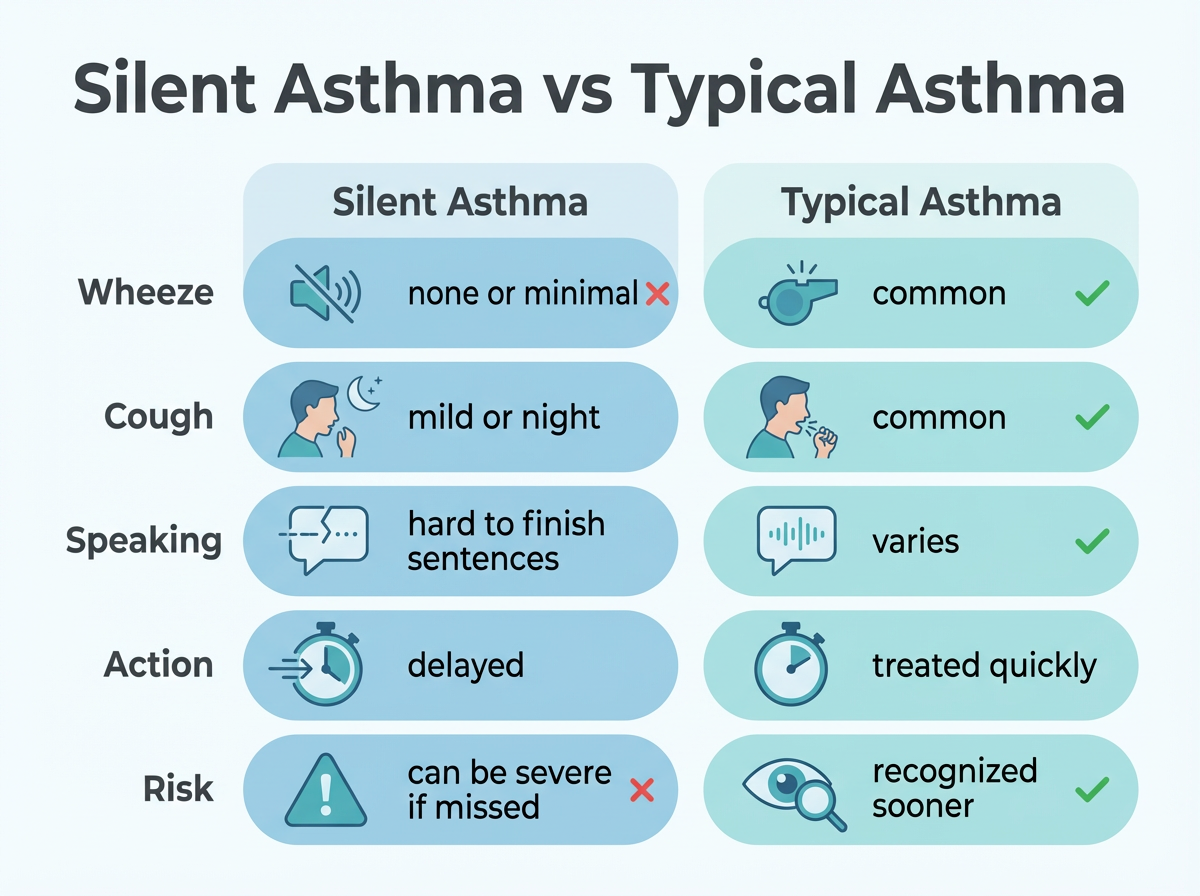
Silent asthma can be easy to miss. Compare key signs with typical asthma so you know what to watch for.
| Feature | Silent Asthma | Typical Asthma |
|---|---|---|
| Wheeze | None or very quiet | Common |
| Cough pattern | Mild, nighttime more common | Frequent during flare |
| Speaking | Hard to finish sentences | Varies |
| First signs noticed | Breathlessness, chest tightness, fatigue | Audible wheeze, cough, chest tightness |
| Action timing | Sometimes delayed because signs are subtle | Treated sooner because signs are obvious |
| Risk if missed | Can become severe or life-threatening | Lower when treated promptly |
Note: Use these clues alongside your written asthma action plan from your doctor.
Key line: No wheeze does not mean no danger—silent asthma attacks can still be severe or life-threatening.
Silent Asthma Symptoms in Adults
Adults usually show quieter patterns that are easy to miss:
- Short breath during routine tasks like one flight of stairs or carrying groceries
- Chest heaviness or pressure that comes and goes
- Nighttime cough or waking up tight
- Needing more breaks during exercise
- Feeling unusually tired or edgy
- Slow recovery after a cold or smoke exposure
Many adults blame these signs on aging, stress, or being out of shape. If these patterns are new or getting worse, talk with your doctor and update your asthma action plan. Because these signs overlap with other conditions, your doctor can help sort out whether silent asthma is part of the problem.
Takeaway: In adults, silent asthma usually looks like short breath and fatigue, not loud wheeze.
How Silent Asthma Is Diagnosed
Your doctor will listen to your story and then test how your lungs move air. Common tools include:
- Spirometry to measure how much and how fast you exhale
- Peak flow checks to compare against your personal best
- FeNO or other tests to assess airway inflammation
- Oxygen level check and a careful chest exam
Keeping a symptom and peak flow diary helps connect triggers, timing, and flares. If quick-relief medicine improves your breathing and numbers, that supports a diagnosis of asthma. Only a doctor can diagnose asthma and decide which tests you need. Build a simple action plan you can follow at home.
Takeaway: Diagnosis relies on your story plus lung tests like spirometry and peak flow.
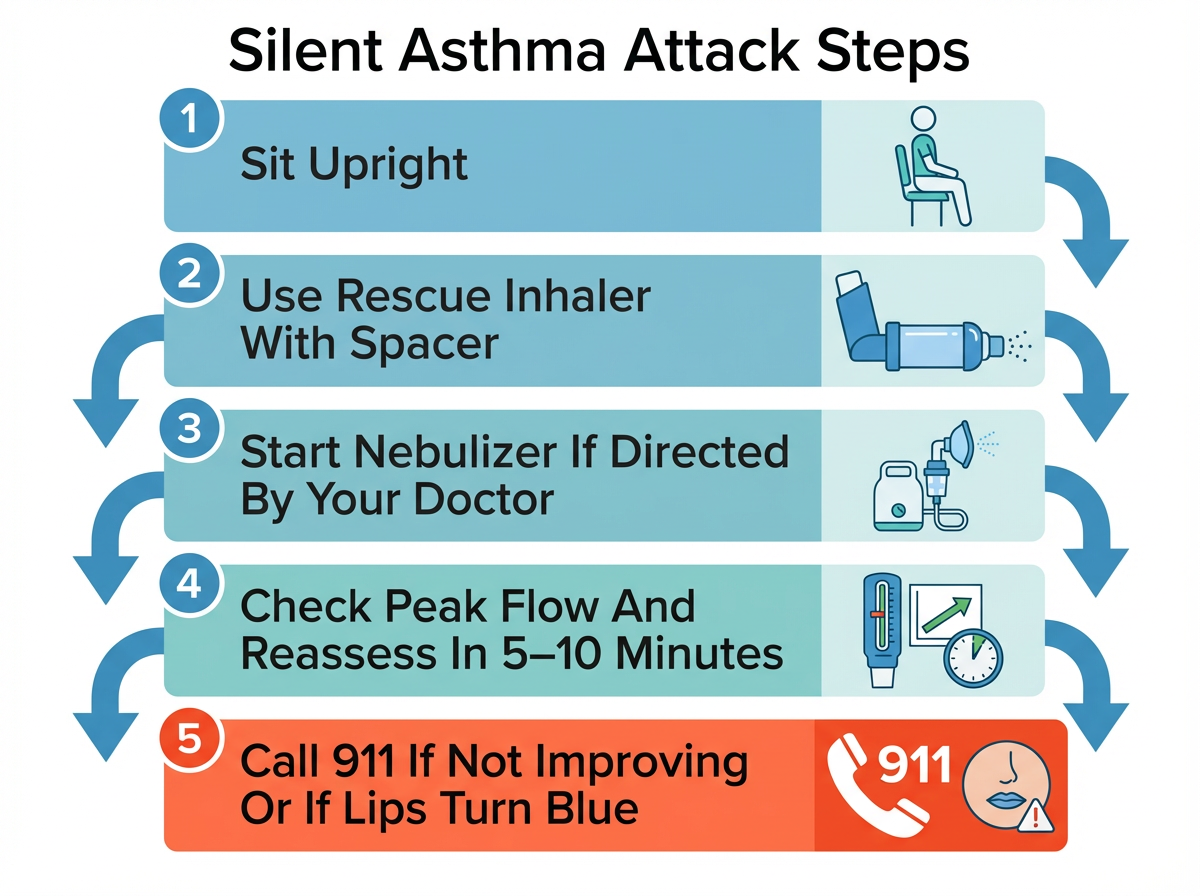
Immediate Steps During a Silent Asthma Attack
These steps are general guidance and don’t replace the specific asthma action plan from your doctor.
Follow your written asthma action plan. If you do not have one, use these steps while you seek guidance:
- Sit upright and focus on slow, steady breaths.
- Use your quick-relief inhaler with a spacer as directed by your doctor.
- If your doctor has told you to use a nebulizer for flares, start it now.
- Check your peak flow if you have a meter and compare it to your zones.
- Recheck symptoms in 5 to 10 minutes. Repeat rescue steps per your plan.
- If symptoms are severe, you cannot speak in full sentences, your lips or nails turn blue or gray, or your peak flow is in the red zone, call 911.
- Do not drive yourself to the ER if breathing is getting worse.
Safety note: Talk to your doctor before trying a new medication or changing doses. If you are not sure what your plan says, call your doctor or seek urgent care.
Rule: Start rescue steps from your asthma action plan early and call 911 if breathing is not improving within minutes.
Treatment Options for Silent Asthma
Treat the swelling daily and act fast during a flare. Silent asthma is treated with the same medicines used for asthma, but you and your doctor focus closely on early warning signs.
- Daily control: inhaled corticosteroids or combination inhalers as prescribed
- Quick relief: short-acting bronchodilator for sudden symptoms
- Add-ons your doctor might consider: leukotriene modifiers, biologics, or short courses of oral steroids for severe flares
- Nebulized medicines when you cannot use an inhaler well or need longer breathing time
- Airway clearance techniques for mucus when recommended
- Trigger control: smoke, dust, cold air, viral illness, strong smells
Safety note: This is general information. Do not start, stop, or change medicines on your own. Talk to your doctor before trying a new medication.
Takeaway: Control airway swelling every day and treat quiet flares early.
Portable Nebulizers and Hypertonic Saline
A portable nebulizer like the TruNeb portable mesh nebulizer can help you stay ready at home and on the go. It is compact and quiet, so it fits easily in a bag or on your nightstand. If your doctor prescribes a nebulized rescue medicine or sterile hypertonic saline (3% or 7%) for mucus clearance, a mesh nebulizer can deliver the treatment where you are. Hypertonic saline is not for everyone and can irritate some people’s airways.
TruNeb offers portable nebulizers and sterile hypertonic saline options so you can keep your kit simple. Use only the strength and schedule your doctor recommends. Keep your rescue inhaler, spacer, and portable nebulizer together as part of your action kit.
⚠️ If you see products labeled “steam inhaler,” know these are not the same as nebulizers and are not meant for breathing in asthma medications.
Safety note: These tools support care but do not replace urgent evaluation for severe or rapidly worsening symptoms. Talk to your doctor before trying a new medication. If you’d like to learn more about portable nebulizers and how they fit into your plan, talk with your doctor.
Takeaway: Keep rescue tools close so a quiet flare does not catch you far from help.
How Long Does a Silent Asthma Attack Last?
It depends on the person and the trigger. Mild attacks can ease within minutes after quick-relief medicine. Some flares build over hours, especially with a cold or smoke exposure. If symptoms do not improve after your first rescue steps, or they return within a short time, follow the next step in your action plan or contact your doctor. Your own action plan from your doctor may use different time frames—follow that first.
Seek emergency care now if you cannot speak in full sentences, your peak flow is in the red zone, your lips or nails turn blue or gray, or you feel worse despite treatment.
Guide: If rescue steps do not ease symptoms within 15–20 minutes, seek urgent care, unless your doctor has given you different instructions.
Prevention and Your Action Plan
A clear plan turns quiet clues into quick action.
- Know your personal triggers and reduce exposure
- Take daily controller medicines as prescribed
- Keep a spacer with your inhaler and check your technique
- Track peak flow and set simple green, yellow, red zones
- Store rescue inhaler and a portable nebulizer together for fast access
- Update your plan after any ER visit or flare
- Ask your doctor about recommended vaccines and manage allergies, reflux, or sinus issues
Print your plan, place copies at home and work, and teach a family member how to help if you cannot speak during a flare. You can even keep a printed checklist of your silent asthma warning signs and the steps you will take.
Takeaway: A written action plan makes early signs easier to act on.
Frequently Asked Questions
Tap or click a question below to see the answer:
These answers are general and don’t replace medical advice from your own doctor.
A silent chest is when airflow is so limited that you hear little to no wheeze. It is a red-flag emergency. Start your action plan and call 911 if breathing is getting harder or you cannot speak.
Yes. Quiet symptoms can delay treatment, which can lead to a serious drop in oxygen. Start rescue steps early and seek emergency care if symptoms are severe or not improving.
Yes. This is called silent asthma—an asthma attack without wheezing. Look for shortness of breath, chest tightness, trouble speaking, fast breathing, and a drop in peak flow.
Your doctor uses your symptom history plus lung tests like spirometry and peak flow. Some clinics also use FeNO to measure airway inflammation. Only a doctor can diagnose asthma. See the section above for more detail.
Mild attacks sometimes improve within minutes after rescue medicine. Others can last hours, especially with a cold or smoke. If not improving after 15–20 minutes or worsening, seek urgent care and follow your own action plan first. See the section above for more detail.
Daily controller medicines reduce airway swelling. Quick-relief inhalers treat sudden symptoms. Some people use nebulized medicines when advised. Your exact plan should come from your doctor.
No. A nebulizer does not replace an inhaler. It is another way to deliver medicine. Some people use both, depending on the situation and what their doctor recommends.
Hypertonic saline (3% or 7%) can help thin mucus for some people when a doctor recommends it. It is not for everyone and can irritate airways. Talk to your doctor before trying a new medication.
Keep it with your rescue inhaler and spacer so you can treat early signs at home or on the go, as your plan directs. A compact device like TruNeb can make this easier, but your doctor should tell you when to use it.
Go now if you cannot speak in full sentences, your lips or nails turn blue or gray, your peak flow is in the red zone, or symptoms do not improve quickly after rescue treatment.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk to your doctor about your asthma symptoms and treatment, and call 911 in an emergency.