On this page

Understanding the Feeling: Why You Get Breathless Lying Flat
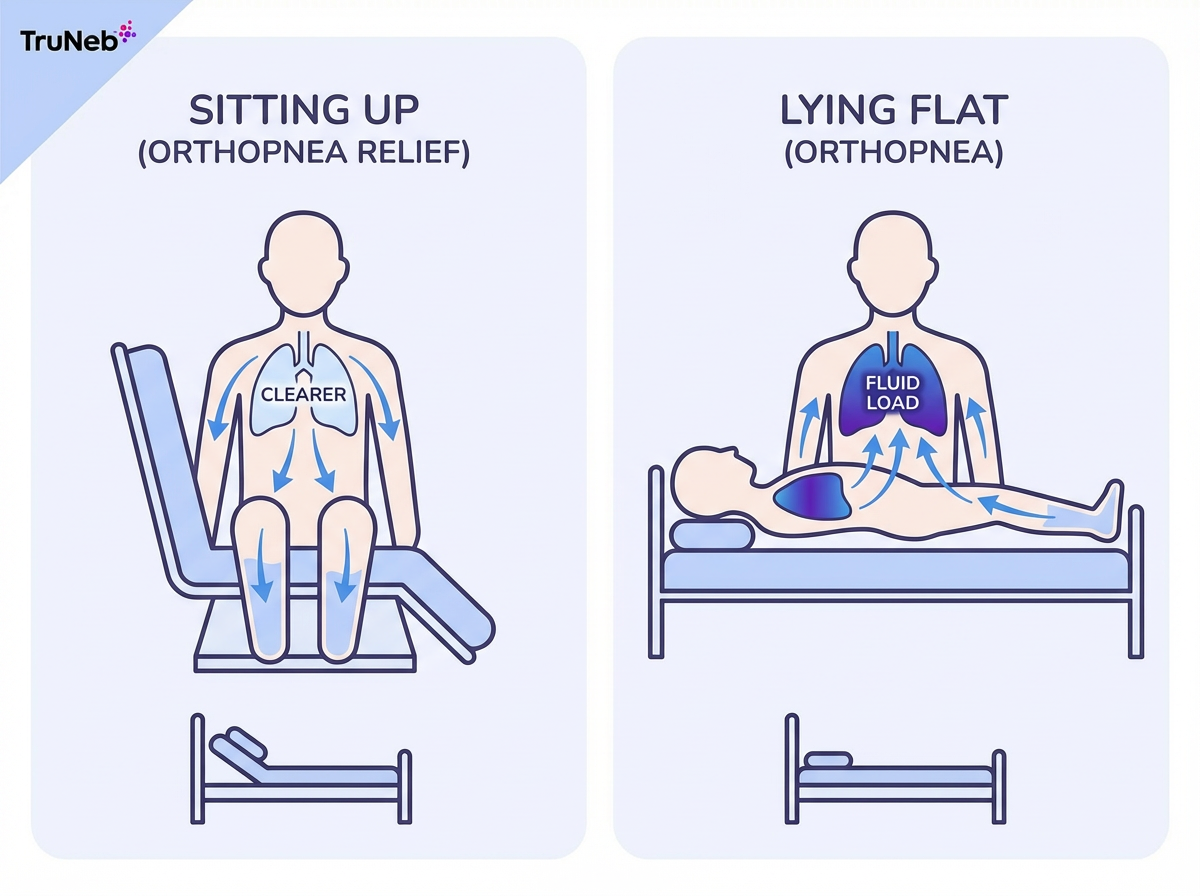
Shortness of breath when lying down is called orthopnea. It usually eases when you sit or stand.
When you lie flat, gravity shifts blood and fluid toward your chest. Your lungs have less room to expand, so breathing can feel tight until you sit up.
If you sleep better propped up on extra pillows, that's a clue you're dealing with orthopnea.
Orthopnea isn't the same as paroxysmal nocturnal dyspnea. With PND, you fall asleep, then wake up after a while suddenly gasping; sitting up brings relief.
Key point: Orthopnea is a symptom, not a disease, and it deserves attention.
If you only feel short of breath when lying flat and it eases quickly when you sit up, doctors consider that abnormal and worth checking.
Heart-Related Causes: Why Lying Down Can Point to Your Heart
A top cause of orthopnea is heart failure. Lying flat sends more blood back to a weak heart, which can push extra fluid into the lungs (pulmonary edema), making it hard to breathe until you sit up.
Doctors often ask, "How many pillows do you use?" Needing two or more pillows is a red flag that your heart needs a check.
Other, less common heart problems can do this too, like severe valve disease or fluid around the heart. Paroxysmal nocturnal dyspnea (waking up gasping after a while asleep) often happens in the same heart failure setting as orthopnea.
If you notice new or worsening breathlessness in bed and you have heart risk factors, call your doctor promptly. Use the red flags below to know when to go to the ER.
Key point: New or worsening breathlessness when you lie down is a classic warning sign of heart trouble and deserves prompt evaluation.
Lung and Airway Causes: Breathing Conditions That Make Lying Down Hard
Not all nighttime breathlessness comes from the heart. Lung and airway problems can do it too.
COPD and severe asthma can feel worse when you recline. Your lungs don't expand as well and mucus can spread out and clog airways. A lot of people feel better sleeping slightly upright or in a recliner. Using your prescribed inhaler or a nebulizer before bed can help keep airways open.
Obesity can press on your diaphragm when you lie on your back, so breathing gets shallow and oxygen levels can drop at night. You might notice your pulse oximeter readings fall when you lie flat.
Obstructive sleep apnea is different but common at night. The airway can collapse during sleep, causing loud snoring, pauses in breathing, and gasping awakenings. A sleep study and CPAP can help.
A portable mesh nebulizer such as TruNeb can deliver your prescribed bronchodilator or hypertonic saline (3% or 7%) before bed to help clear mucus. Use it only as directed by your doctor. If you see products labeled "steam inhaler," know they're not the same as nebulizers and are not for breathing prescription medications. Never rely on a nebulizer instead of urgent care for new or severe shortness of breath.
Device comparison: nebulizer vs steam inhaler vs CPAP
| Device | Main purpose | Delivers prescription meds? | Typical use at night | Not for |
|---|---|---|---|---|
| Nebulizer | Turn liquid medicine or saline into a fine mist you breathe | Yes, as prescribed | COPD or asthma airway therapy, mucus clearance | Heart-related fluid in the lungs or emergencies |
| Steam inhaler | Provide warm moisture for comfort | No | Dry nose or throat comfort | Breathing prescription medicines or treating lung disease |
| CPAP | Keep the airway open for sleep apnea | No | Obstructive sleep apnea treatment | Shortness of breath from heart or lung disease |
Key takeaway: Nebulizers deliver medication into your lungs; steam inhalers only provide warm moisture and aren't for medicines; CPAP treats sleep apnea by keeping your airway open.
Note: CPAP requires a sleep study and a prescription.
Key point: Lung and airway problems like COPD, asthma, obesity, and sleep apnea can all make breathing harder when you lie flat, while inhalers or nebulizers can help when used exactly as your doctor prescribes.
Other Causes: Pregnancy, Reflux, Allergies, Anxiety, and Rare Issues
Pregnancy can make you short of breath, especially late in pregnancy. The growing uterus pushes up on the diaphragm. Sleeping on your left side with extra pillows usually helps. Severe or sudden breathlessness in pregnancy needs prompt care. Call your doctor or go to urgent care right away.
Acid reflux can trigger coughing or a choking feeling when you lie down, so try finishing dinner a few hours before bed and raising the head of your bed.
Anxiety or panic can also make it feel hard to breathe when you lie down. Fast, shallow breathing and focusing on every breath can create a smothered feeling even when your lungs are healthy. If your doctor has ruled out heart and lung problems, nighttime anxiety could be part of the picture.
Nasal allergies and congestion can force mouth-breathing and make you feel tight when supine. Clearing your nose and propping your head can help.
Rarely, weakness of the breathing muscles (like a paralyzed diaphragm or certain neuromuscular diseases) or severe thyroid problems can cause orthopnea, almost always alongside other obvious symptoms. Your doctor can sort this out.
Key point: Pregnancy, reflux, allergies, anxiety, and a few rare conditions can all play a role in orthopnea, so any new or severe symptoms in these settings still warrant a check with your doctor.
When to Seek Help: Nighttime Breathing Red Flags
Know the danger signs so you can act fast.
- ⚠️ Call 911 now if you can't catch your breath even when upright, you have blue lips or face, chest pain or pressure, confusion or fainting, or heavy sweating with severe shortness of breath. Don't drive yourself.
- Go to the ER if symptoms start suddenly, are getting worse, or you can't reach your doctor and feel significantly unwell.
- Go to the ER if you have high fever and a bad cough or new leg swelling along with shortness of breath, as these can signal pneumonia, blood clots, or heart failure.
- Make a prompt doctor's appointment if orthopnea is new or worsening, or if you have known heart or lung disease.
Key point: If you can't breathe even when sitting up, treat it as an emergency.
Talk to your doctor before trying a new medication.
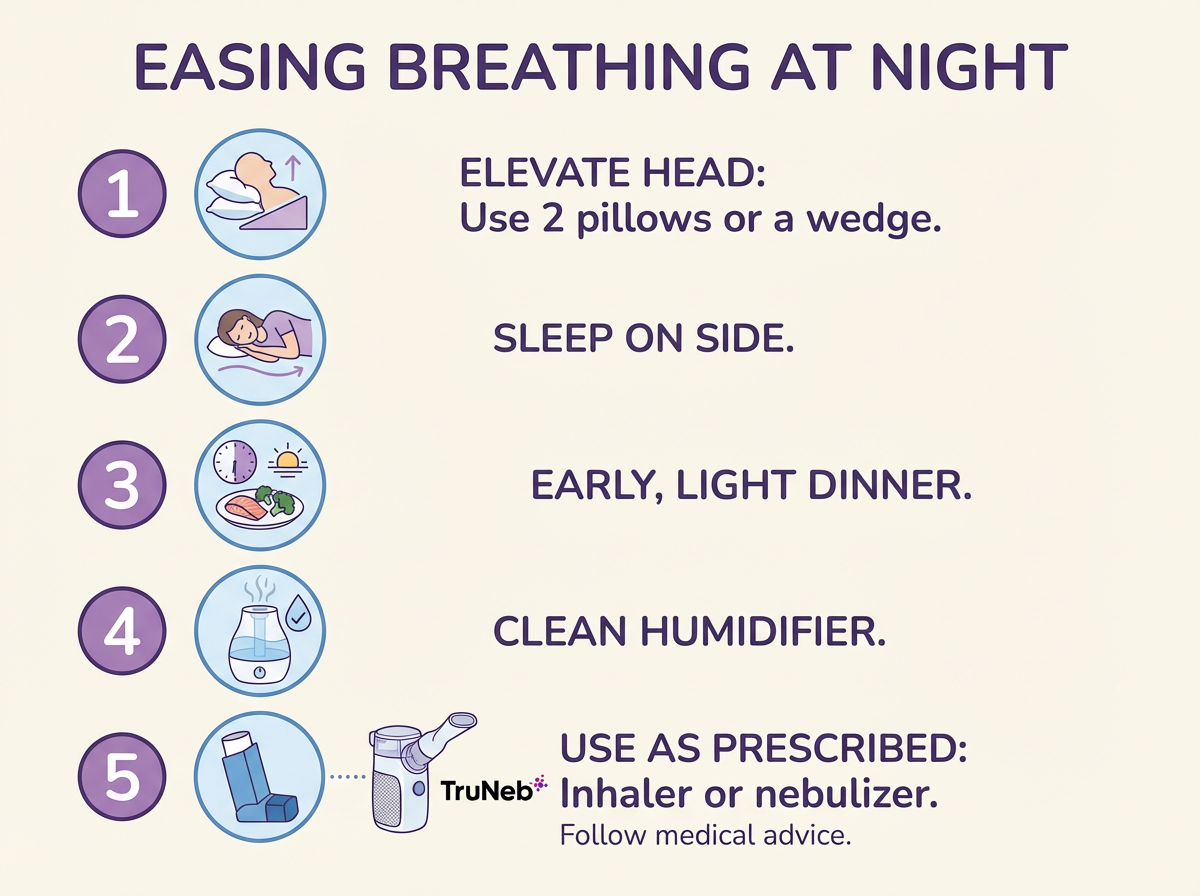
How to Ease Breathing at Night: Simple Ways to Sleep Better
While your care team treats the cause, these steps can make nights easier:
- Raise your head and upper body with extra pillows or a wedge, or elevate the head of the bed. Side-sleeping, especially on your left side can also help.
- Follow the nighttime plan you've set up with your doctor: use your prescribed inhalers or nebulizer before bed; use oxygen or CPAP only if your doctor prescribed it. Avoid big meals and alcohol late in the evening, and keep a clean humidifier for comfort.
- Practice a simple breathing or relaxation exercise at bedtime if anxiety is part of your symptoms, such as slow belly breathing or a short relaxation routine.
Key point: Sleeping with your head elevated and following your treatment plan can make breathing easier at night.
Frequently Asked Questions
Use these quick answers to understand common questions about orthopnea and nighttime breathlessness. Tap or click a question below to see the answer:
Not always. Heart failure is a classic cause, but COPD, asthma, obesity, reflux, congestion, and even anxiety or panic can also play a role. Because heart failure is common and serious, get checked if you notice new or worsening symptoms.
Orthopnea starts right when you lie flat and eases when you sit up. Paroxysmal nocturnal dyspnea wakes you from sleep after a while, and also eases when you sit up.
In COPD, obesity hypoventilation, or sleep apnea, lying on your back can limit airflow and lower oxygen. Tell your doctor if your oximeter readings fall when supine.
It can help if you have a diagnosed lung condition that benefits from airway therapy (like COPD or asthma). For example, a small portable device like TruNeb can deliver your prescribed medicine or saline before bed. It won't treat heart-related fluid in the lungs. Use only under medical guidance.
They use your story and an exam, plus tests like a chest X-ray, blood tests, an echocardiogram for heart function, breathing tests for lung disease, or a sleep study for suspected apnea. The goal is to find the cause and target it.
⚠️ Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms and before changing any medications or treatments.