On this page

What Saline to Use for a Baby’s TruNeb Portable Nebulizer and Why
For most infants, pediatricians use sterile 0.9% normal saline in nebulizers because it matches the body’s salt level. It’s gentle and adds moisture. No medicine. Hypertonic saline (3% or 7%) is stronger and is used only if your pediatrician prescribes it for very thick mucus. For most babies, the best saline solution for a nebulizer is sterile 0.9% normal saline made for inhalation.
A portable mesh nebulizer delivers a fine, quiet mist. What you put in the cup matters most for safety and comfort.
Key takeaway: For most babies, pediatricians recommend sterile 0.9% normal saline in the nebulizer, and 3% hypertonic saline should only be used if your doctor prescribes it.
Normal Saline Is the Gold Standard for Infants
Normal saline is sterile 0.9% sodium chloride. It matches the salt level in body fluids, so it feels gentle on tiny airways. It adds moisture, helps loosen mucus, and doesn’t contain medicine.
Use only vials labeled for inhalation. Single‑use, preservative‑free saline vials are made to be nebulized. These are available over the counter in most pharmacies—look for unit‑dose vials labeled for inhalation use. This is what hospitals and pediatricians rely on for babies with mild coughs and stuffy chests.
Key takeaway: Normal saline is 0.9% sodium chloride made for inhalation in nebulizers and is gentle for babies.
Why Hypertonic Saline Is Doctor Directed
Hypertonic saline is saltier than 0.9%. The common strengths are 3% and 7%. This pulls water into the airways to thin very sticky mucus. Is hypertonic saline safe for infants? Hypertonic saline can be safe for infants, but only when a pediatrician prescribes and supervises its use.
Doctors often use 3% saline for infants with bronchiolitis from RSV when mucus is thick. Some hospital studies found that 3% hypertonic saline can ease breathing and sometimes shorten hospital stays for infants with bronchiolitis. But it can also make babies cough more or feel throat irritation. That’s part of how it works, but it’s not routine for home use unless your pediatrician prescribes it. The 7% solution is much stronger and is usually reserved for specialist care, like cystic fibrosis.
Parents should not switch from 0.9% to 3% or 7% saline on their own; that decision belongs to your baby’s doctor.
TruNeb offers 3% and 7% sterile vials made in an FDA‑approved lab, as an option when your pediatrician prescribes hypertonic saline.
Key takeaway: In infant nebulizers, 3% hypertonic saline can thin stubborn mucus in bronchiolitis but must be used only under a doctor’s guidance because it can irritate sensitive airways.
Normal vs Hypertonic Saline for Infant Nebulizers at a Glance
For infant nebulizer treatments, 0.9% normal saline is the everyday gentle option; 3% is doctor-directed for thick mucus; 7% is typically specialist use.
| Saline type | What it does | When it’s used | Who decides | Availability |
|---|---|---|---|---|
| 0.9% normal (isotonic) | Adds moisture, helps loosen mucus, gentle on infant airways | Most baby nebulizer sessions when your doctor recommends saline | Your pediatrician; commonly used at home | OTC unit‑dose vials labeled for inhalation |
| 3% hypertonic | Draws water into airways to thin thick, sticky mucus | Selected cases (e.g., bronchiolitis/RSV) when prescribed | Doctor-directed only | OTC or behind the counter, depending on pharmacy |
| 7% hypertonic | Stronger mucus-thinning effect, higher irritation risk | Specialist care (e.g., cystic fibrosis) when prescribed | Specialist prescribes and supervises | Prescription/specialty supply |
Note: Use only sterile, inhalation-labeled saline vials. Follow your pediatrician’s plan for type, amount, and frequency.
Key takeaway: For infant nebulizers, 0.9% normal saline is the gentle everyday option, 3% hypertonic saline is doctor-directed for thick mucus, and 7% hypertonic saline is reserved for specialist use.
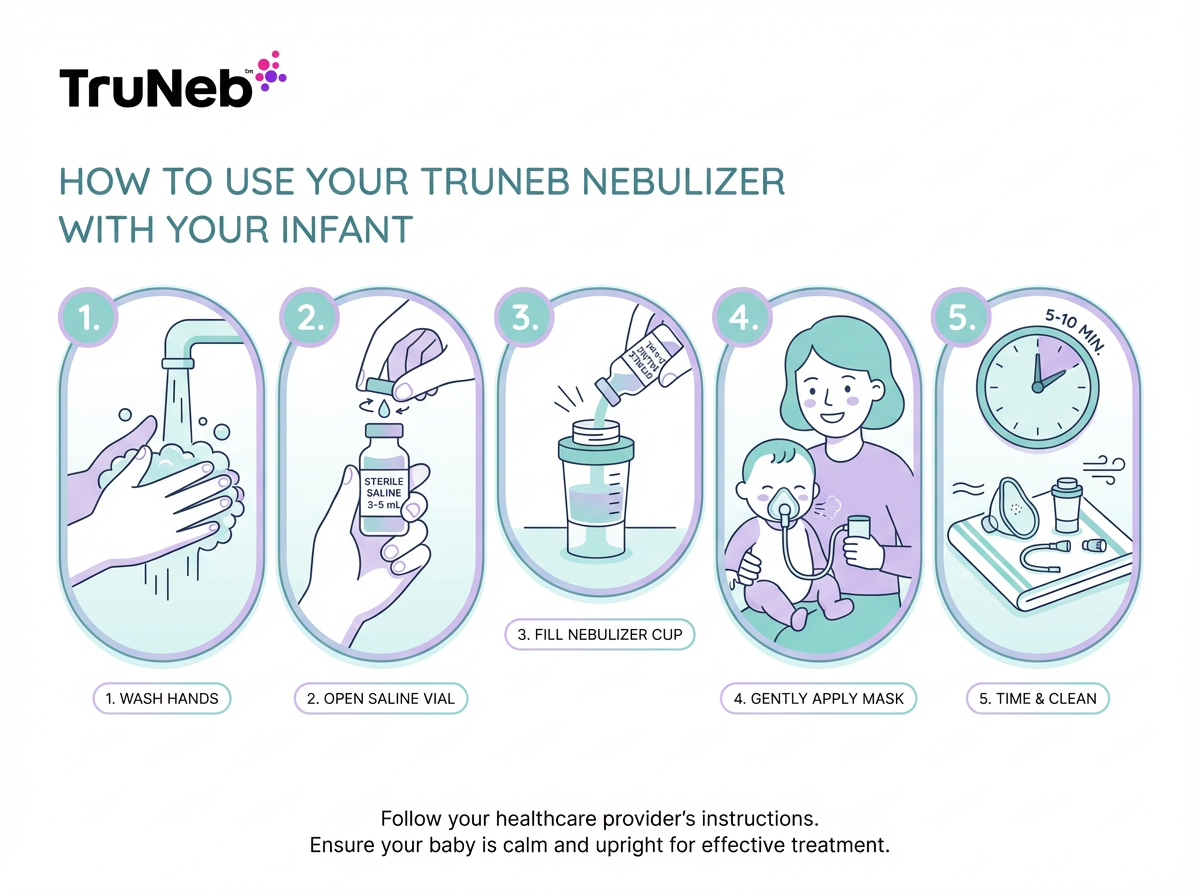
How to Nebulize Your Baby with Saline Step by Step
These steps are meant to help you follow your doctor’s plan safely. These steps apply whether you’re using a TruNeb portable mesh nebulizer or another baby‑friendly device.
- Wash your hands and set up. Have the nebulizer, a sterile saline vial, and the infant mask ready. Make sure your mesh nebulizer like TruNeb is charged and assembled.
- Measure the saline. Most unit‑dose vials for nebulizers contain about 3–5 mL. Use the amount your pediatrician prescribed.
- Fill the cup. Open the sterile vial and pour the saline into the medication cup. Do not add anything else.
- Fit the mask. Place the infant mask snugly over your baby’s nose and mouth. Keep your baby upright on your lap.
- Start the treatment. Turn on the nebulizer. A fine, quiet mist should flow. Sessions usually take 5–10 minutes. Keep the mask on until the mist slows or stops.
- Comfort and observe. Pause if your baby cries hard. Soothe and restart so more mist reaches their lungs.
- Clean up. Rinse the cup and mask per instructions and air‑dry. This helps prevent germs and residue.
Key takeaway: A safe saline nebulizer session for your baby means clean hands, one sterile saline vial, a snug infant mask, and about 5–10 minutes of calm mist as directed by your doctor.
Safety Tips for Nebulizing Saline with Babies
- Use only sterile, inhalation‑grade saline. Do not use tap water, homemade mixes, contact lens saline, or nasal rinse solutions in a nebulizer.
- Follow the prescribed concentration. Don’t switch to 3% or 7% on your own.
- One vial per session. Discard leftovers. Use fresh vials and store as labeled.
- Stay with your baby. Pause if they cry hard or seem distressed. Restart when calm.
- Keep parts clean. Rinse and air‑dry after each use to prevent germs and residue.
- Don’t use steam inhalers in place of a nebulizer—steam is not for breathing medications or saline into the lungs.
- Expect mild cough or sneezing as mucus loosens. If breathing worsens or you see distress, stop and call your pediatrician.
⚠️ If your baby has very fast or labored breathing, ribs pulling in, grunting, pauses in breathing, or blue‑tinged lips or face, call emergency services or go to the ER right away. - Never add essential oils or unapproved substances to the cup.
Safety note: Talk to your doctor before trying a new medication or changing saline strength.
Key takeaway: Only sterile inhalation saline goes in the cup—nothing homemade.

Frequently Asked Questions
Tap or click a question below to see the answer:
Yes—when your pediatrician recommends nebulizer treatments, using sterile 0.9% saline is a common, drug‑free way to add moisture and help loosen mucus in infants.
Most saline vials for nebulizers hold about 3–5 mL. That’s a common vial size, not a dose. Use the amount your pediatrician prescribed, and if you’re unsure, check with your pediatrician instead of guessing.
Yes, devices like TruNeb can nebulize 0.9%, 3%, or 7% saline. Only use hypertonic if your doctor prescribes it, and clean the cup and mesh after use.
0.9% normal saline vials are usually over the counter. 3% is commonly OTC or kept behind the counter depending on the pharmacy. 7% is typically prescription or specialty supply. Always choose products labeled for inhalation.
Saline helps with moisture and mucus clearance, but it doesn’t open tight airways like a bronchodilator. If you see fast or labored breathing, wheezing, ribs pulling in, grunting, pauses in breathing, or blue‑tinged lips or face, seek medical care right away—call your pediatrician urgently or call 911/go to the ER if your baby seems in distress.
Key takeaway: In babies, saline nebulization supports mucus clearance, but any signs of breathing distress still need prompt medical care.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your pediatrician or doctor about your baby’s symptoms, treatments, and any questions about using a nebulizer or saline.