On this page
Normal vs Abnormal Breath Sounds
When your doctor listens to your lungs with a stethoscope, a clear, soft rustling called vesicular breathing is normal.
Abnormal sounds are called adventitious sounds. The main ones are rhonchi, crackles (also called rales), and wheezes. Sometimes you might also hear stridor or a pleural rub in some conditions.
These sounds help point to mucus, fluid, or narrowed airways. They guide the next steps, but they don't provide a final diagnosis by themselves. Only a doctor can interpret these sounds in context alongside your symptoms and exam.
In short: rhonchi, crackles, and wheezes are abnormal noises that can signal a problem in your airways or air sacs.
What Are Rhonchi?
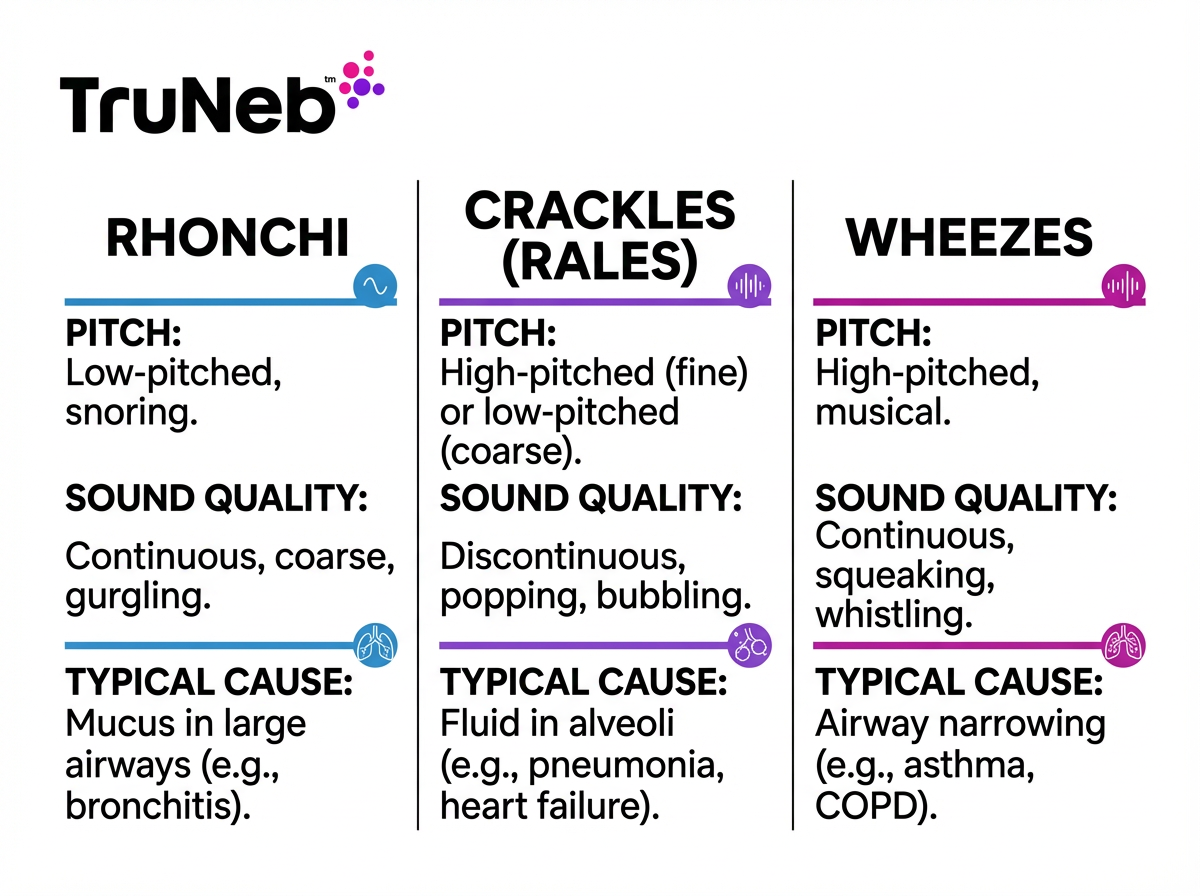
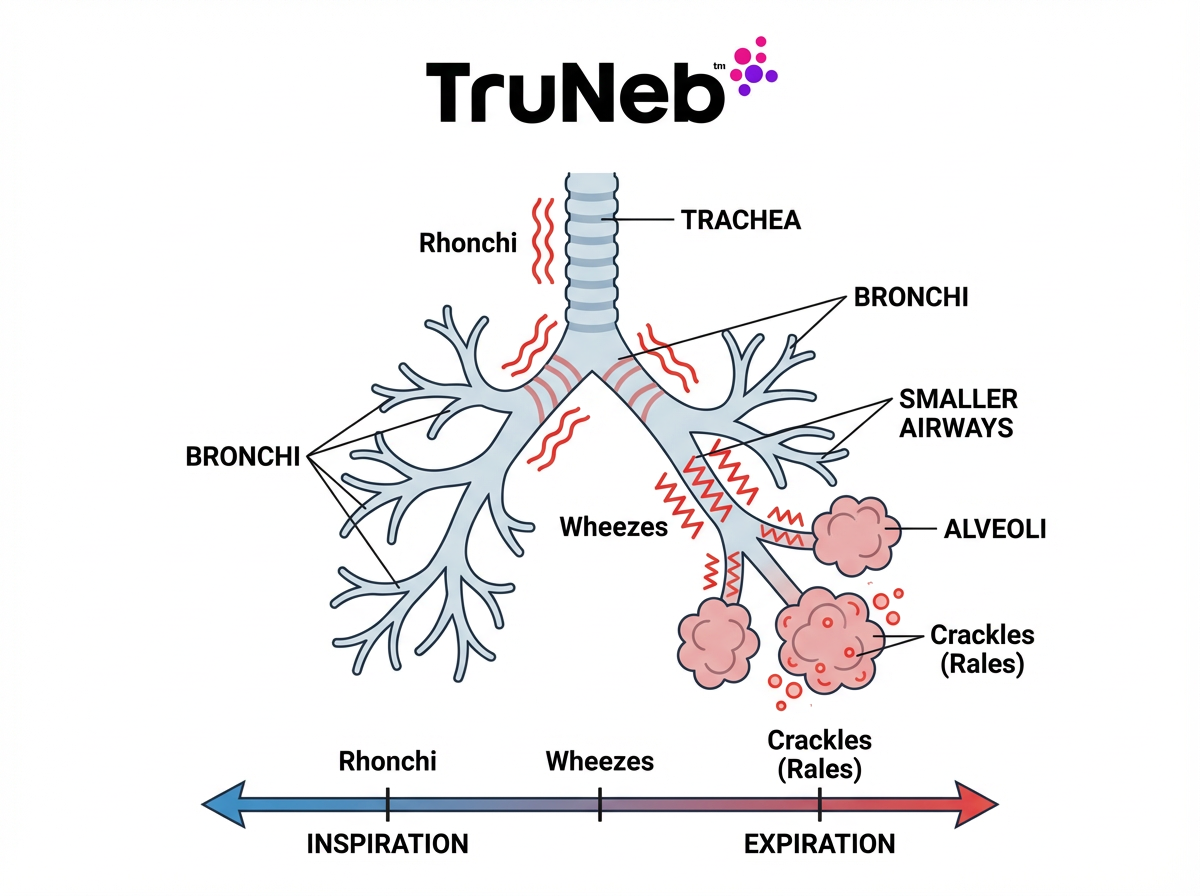
Rhonchi are low-pitched, continuous lung sounds that usually resemble snoring or a wet rumble. They are most noticeable on exhalation, but can be heard during the whole breath.
They happen when air moves past thick secretions or a blockage in the larger airways (the bronchi). Many clinicians describe rhonchi as a type of low-pitched wheeze, also called a sonorous wheeze.
A helpful clue: rhonchi often change or clear after a good cough. Common causes include chronic bronchitis, COPD flare-ups, mucus-heavy pneumonia, cystic fibrosis, and bronchiectasis.
In short: rhonchi = low, snoring sounds from mucus in big airways that usually improve after coughing.
What Are Crackles (Rales)?
Crackles are brief, popping lung sounds. The older word rales means the same thing. Crackles are discontinuous, like tiny snaps or bubbling.
Fine crackles are soft and high-pitched, like rubbing hair between your fingers near your ear. Coarse crackles are louder and lower, like velcro being pulled apart or pouring out a bottle of water.
They are usually heard on inhalation. Crackles form when small airways or alveoli pop open against fluid or sticky walls, or when air moves through fluid. They usually do not clear with a cough. Common causes include pneumonia, heart failure with pulmonary edema, and pulmonary fibrosis. Fine crackles at both lung bases with leg swelling and shortness of breath point to heart failure.
In short: crackles (rales) = brief pops from small airways or air sacs that usually don’t clear with coughing.
Rhonchi vs Crackles: Key Differences and How To Tell
Here’s how to sort them out at the bedside.
Key point: rhonchi typically clear with a cough; crackles usually do not. If rhonchi don't change after repeated coughing, your doctor will consider other causes.
- Pitch: Rhonchi are low and rumbling. Crackles are higher (fine) or lower but brief (coarse).
- Quality: Rhonchi sound like a snore or gurgle. Crackles sound like popping, fizzing, or velcro.
- Timing: Rhonchi are heard more on exhale. Crackles are heard more on inhale.
- Origin: Rhonchi start in larger airways with mucus. Crackles come from small airways or alveoli.
- Causes: Rhonchi point to mucus-heavy problems like bronchitis or COPD. Crackles point to pneumonia, heart failure, or fibrosis.
In short: rhonchi = low, continuous, cough-clearable. Crackles = brief pops that persist after coughing.
Wheezing and Rhonchi: High vs Low-Pitched Sounds
Wheezes are high-pitched, musical whistles from narrowed small airways. They are usually heard on exhalation and are common in asthma and some COPD.
Rhonchi are low-pitched wheezes in larger airways and have a snoring or gurgling quality because mucus is involved. Wheezes do not usually clear with cough. Rhonchi can change after a cough.
A generalized wheeze (for example, in asthma) differs from a wheeze heard in one area, which can suggest a blockage.
Stridor is different: a harsh, high-pitched sound heard mostly on inhalation from the upper airway. It is a warning sign and needs urgent attention. Call emergency services immediately.
In short: wheezes are high whistles from small airways, and rhonchi are low rumbles from mucus in larger airways.
What These Lung Sounds Can Indicate
Rhonchi usually indicate mucus or partial blockage in large airways. That pattern fits problems like bronchitis or a COPD flare.
Crackles indicate fluid or stiff air sacs. That pattern fits pneumonia, pulmonary edema from heart failure, or pulmonary fibrosis. Studies show crackles are a strong bedside clue for pneumonia.
Example: A person with fever and crackles in one lower lung could have pneumonia in that area, so a chest X-ray helps confirm it. Another person with swollen legs and crackles in both bases could have fluid from heart failure.
Doctors always combine lung sounds with your history, exam, and tests before deciding on a diagnosis. Hearing these sounds leads clinicians to next steps, like a chest X-ray or other tests, plus treatment of the underlying cause. Lung sounds are one clue among your symptoms, exam, and test results.
In short: rhonchi point to airway mucus, and crackles point to fluid or stiff air sacs and often prompt imaging to confirm the cause.
Managing Abnormal Lung Sounds and Clearing Airways
Treatment focuses on the cause. If rhonchi come from thick mucus, your doctor can use airway clearance steps: hydration, controlled coughing, chest physiotherapy, and sometimes medicines that thin mucus or open airways. These steps are chosen and guided by your doctor based on your overall health.
Nebulized therapy can help move secretions when prescribed by your doctor. A portable mesh nebulizer, such as TruNeb™, can deliver bronchodilators or hypertonic saline. These medications are prescribed by your doctor for specific conditions and aren't meant to be started on your own. Many clinicians use 3% or 7% hypertonic saline to thin mucus in conditions like bronchiectasis or cystic fibrosis. Hypertonic saline isn't right for everyone and is usually reserved for people with specific diagnoses.
If crackles are from fluid or infection, care targets that problem (for example, your doctor might prescribe diuretics for pulmonary edema or antibiotics for pneumonia). Nebulizers can help with mucus and bronchospasm but don't treat fluid from heart failure. As the condition improves, the crackles usually fade.
Safety note: Talk to your doctor before trying a new medication.
In short: rhonchi usually improve as mucus is cleared, and crackles tend to get better once the fluid or inflammation in the lungs is treated by your doctor.
When To Seek Medical Attention
See your doctor if cough, fever, or new noisy breathing doesn’t get better or gets worse. New crackles with fever can signal pneumonia. New rhonchi with lots of sputum can point to bronchitis or a COPD flare.
Get urgent care if you have severe trouble breathing, chest pain, confusion, or blue lips or fingernails (cyanosis). A harsh inspiratory noise from the upper airway. It is a warning sign and needs urgent attention. Call emergency services immediately.
⚠️ If you have severe trouble breathing, chest pain, confusion, or blue lips or fingernails, call 911 (or your local emergency number) right away.
Key point: if breathing is hard or you notice blue coloring around lips or nails, call emergency services right away.
In short: don’t wait on severe or fast-worsening breathing problems—get help now.
Frequently Asked Questions
This FAQ gives quick answers about rhonchi, crackles, and other lung sounds. Tap or click a question below to see the answer:
Yes. Rales is another word for crackles. Most clinicians now say crackles.
Rhonchi. They often improve after a cough because mucus moves. Crackles usually do not.
Rhonchi are low and snoring from mucus in larger airways. Wheezes are high and musical from narrowed small airways.
No. Crackles can come from pneumonia, heart failure, or fibrosis. Your doctor can order a chest X-ray to find the cause.
Loud rhonchi or wheezing can sometimes be heard at the mouth. Crackles are usually subtle and need a stethoscope.
Yes. Some conditions, like COPD with an infection or bronchiectasis, can produce more than one abnormal sound. Your doctor listens for patterns and decides what tests you need.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk to your doctor about any questions you have and before starting or changing any medication or nebulized therapy.