On this page

Understanding Croup and Why Recurrent Croup Raises Concern
Croup is swelling of the upper airway near the voice box and windpipe. It’s usually caused by viruses like parainfluenza; RSV, rhinovirus, and influenza can do it too. It typically starts with a cold, then a barky cough, hoarse voice, and a harsh sound on inhale called stridor. Most cases happen between 6 months and about 3 years old and improve in a few days.
Recurrent croup means the pattern keeps returning. Doctors usually call it recurrent when a child has more than two episodes in a year, or when croup shows up outside the usual toddler years. Most kids have only one or two episodes, so a repeated history is a signal to look deeper.
Some kids have spasmodic croup. These episodes can start suddenly at night, can have little or no fever, and tend to repeat. Allergies or a sensitive airway can play a role.
Most croup is viral and simple to treat. But recurring episodes can point to airway sensitivity (similar to asthma), reflux irritation, or a structural narrowing that makes any small cold feel big.
Recurrent croup is a pattern, not a diagnosis.
Can Recurrent Croup Indicate Asthma? The Short Answer
Yes, it can. Studies show children with recurrent croup have a higher chance of later asthma compared with children who don’t have repeat episodes. It doesn’t mean your child has asthma now, but it is a clue that the airways can be sensitive.
Key point: Recurrent croup raises asthma risk, but many children never develop chronic asthma.
Think of the airway like a tree. Croup affects the upper trunk near the voice box. Asthma affects the small branches deep in the lungs.
Recurrent croup is a risk signal, not a sure sign.
Why Are Asthma and Recurrent Croup Connected?
The core link is airway hyperreactivity. In some children, the airway lining is extra sensitive. A cold can inflame the voice box (croup) and also trigger the lower airways to spasm (asthma). The same child can show both patterns at different times.
Asthma is chronic inflammation of the lower airways that causes wheeze, cough, and breathing trouble.
Family history matters. Kids with allergies, eczema, or a parent with asthma are more likely to have sensitive airways. That sensitivity can show up first as recurrent croup and later as wheeze or night cough.
Age is a clue. Croup outside the usual toddler years, especially in school-age kids, is less typical and raises the chance of an underlying issue. When croup happens again and again with each cold, that recurring history also points toward a reactive airway.
Newer evidence adds hope. Some specialists report that, under their guidance, starting an inhaled corticosteroid at the first signs of a cold can reduce the severity of recurrent croup in a number of children without fixed airway problems. This supports the idea that inflammation and reactivity drive the pattern for a lot of kids.
Shared airway sensitivity links croup and asthma in some kids.
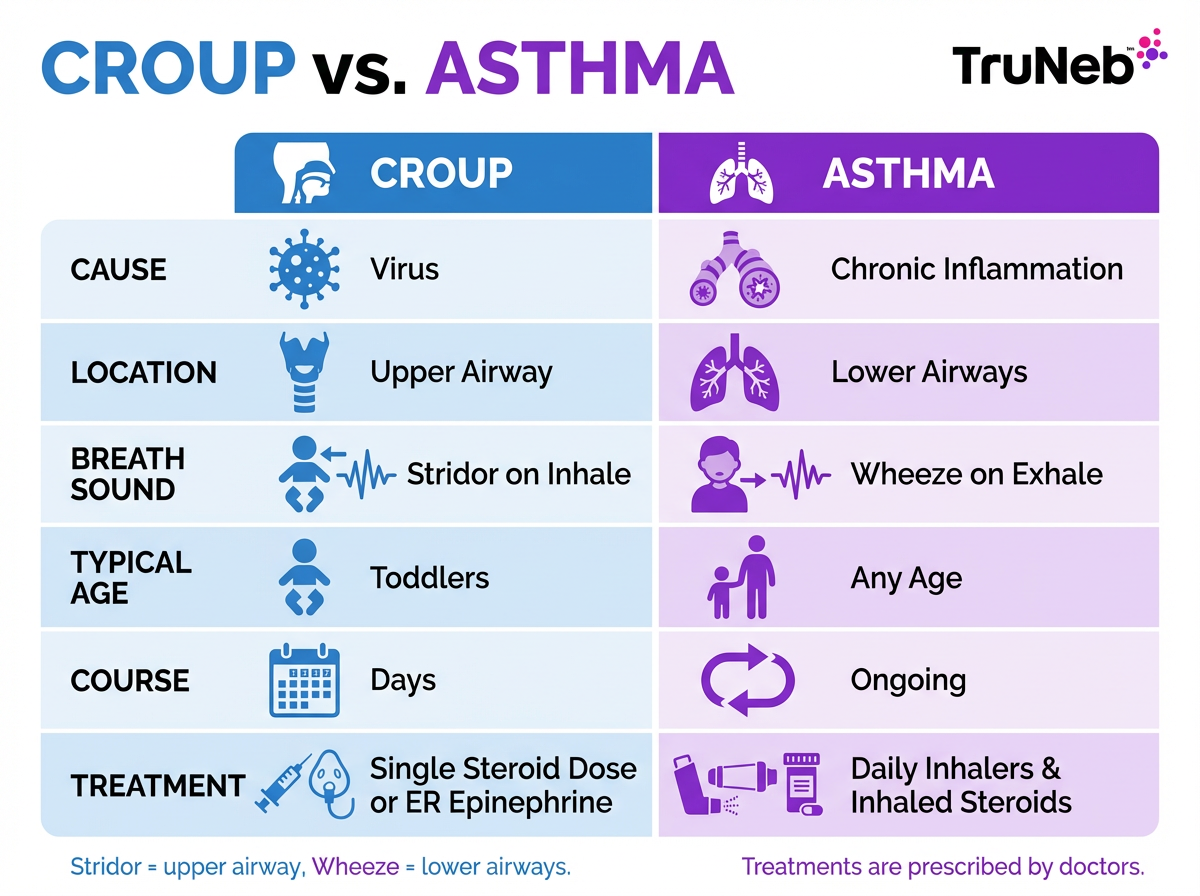
Croup vs Asthma: Telling the Difference
These clues help you tell upper-airway croup from lower-airway asthma.
Croup vs asthma: quick comparison
| Feature | Croup | Asthma |
|---|---|---|
| Cause | Usually a virus (parainfluenza, RSV, other cold viruses) | Chronic inflammation of the lower airways with flares |
| Where It Acts | Upper airway near vocal cords and windpipe | Lower airways inside the lungs |
| Main Sound | Barky cough; stridor on inhale | Wheeze on exhale; chest tightness |
| Typical Age | Common in toddlers; rare beyond ~6 | Any age; commonly starts in school years |
| Course | Lasts days, then resolves | Ongoing tendency with flares over months |
| Usual Treatment | Usually treated by doctors with a single steroid dose; hospital nebulized epinephrine if severe | Managed with doctor-prescribed inhaled bronchodilators and inhaled steroids, typically as part of an asthma action plan |
Key takeaway: Stridor on inhale often suggests croup, while wheeze on exhale often suggests asthma, but your doctor should confirm what’s going on.
Note: Treatments are prescribed and given by doctors. Don’t start medicines without medical advice.
What Causes Recurrent Croup?
If you’re wondering, "why does my child keep getting croup?", here are the most common reasons.
Usually, it’s repeat viral infections in a child whose airway reacts strongly. Young children catch colds frequently, and a sensitive upper airway can swell with each virus.
Airway hyperreactivity is common. Some children have a reactive pattern that overlaps with asthma. They can wheeze with some colds and have a croupy cough with others. This overlapping pattern is one reason doctors look for asthma in kids with recurrent croup.
Allergies and atopy can add irritation. Eczema or allergic rhinitis in the child, or asthma in the family, raises the odds of repeat episodes. Reflux (GERD) can also inflame the upper airway, especially at night. Rarely, eosinophilic esophagitis contributes through chronic irritation.
Sometimes structure is the driver. Subglottic stenosis (narrowing under the vocal cords), laryngomalacia or tracheomalacia (floppy airway), a vascular ring pressing on the trachea, vocal cord paralysis, or a laryngeal cleft can all mimic or trigger croup again and again. Very rarely, recurrent respiratory papillomatosis does the same. A stuck foreign body or smoke exposure can also keep symptoms returning.
Most repeated croup is viral atop a sensitive airway; sometimes anatomy or reflux is the driver.
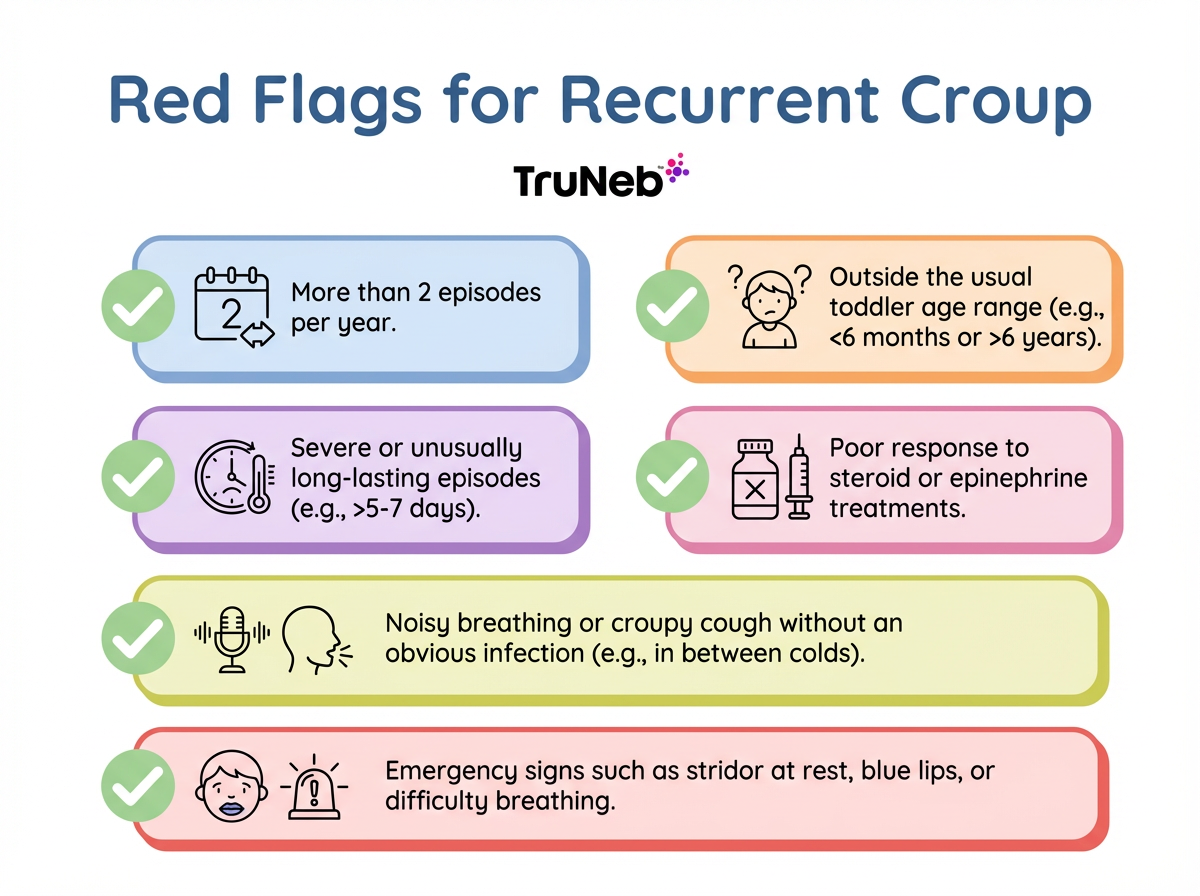
When to Worry: Red Flags in Recurrent or Atypical Croup
Most single croup episodes pass quickly. These signs mean it’s time to look deeper:
- More than two bouts in a year, or croup with nearly every cold.
- Croup outside the usual age range (under 6 months or older than about 5–6 years).
- Severe or prolonged episodes, or little relief after standard treatments like dexamethasone or ER epinephrine.
- Barky cough or stridor even without a cold, or with exercise or allergen exposure.
- Trouble swallowing, drooling, voice changes between illnesses, or poor weight gain.
- ⚠️ Emergency signs anytime: stridor at rest, struggling to breathe, blue lips. Go to the ER.
Key point: If red flags show up, ask your pediatrician about referral to an ENT or a pediatric pulmonologist.
Frequent, older-age, severe, or treatment-resistant croup deserves a specialist visit.
Getting Diagnosed: How Doctors Investigate Recurrent Croup
Your child’s doctor starts with the story: how often it happens, what helps, whether there’s wheeze between colds, feeding trouble, or a family history of asthma or allergies. The exam looks for stridor, wheeze, and growth patterns.
Next comes targeted testing. A number of children are referred to an ENT specialist or pediatric pulmonologist. Depending on your child’s pattern of symptoms, the team can order a neck or chest X-ray. The most direct test for structure is airway endoscopy under anesthesia. Doctors use tiny scopes to inspect the voice box, subglottic area, trachea, and sometimes the esophagus (sometimes called a triple scope). This can find narrowing, floppiness, or other anatomy, and it frequently comes back normal, which is reassuring.
If asthma is suspected and your child is old enough, spirometry (a breathing test) can check for reversible airway narrowing. If a child is too young, doctors can try a short, doctor-led trial of asthma medicines to see if symptoms improve. Allergy or reflux evaluations are added based on clues from the history.
Not every child needs every test.
Airway endoscopy checks structure; a breathing test or guided medicine trial checks for reactive airways.
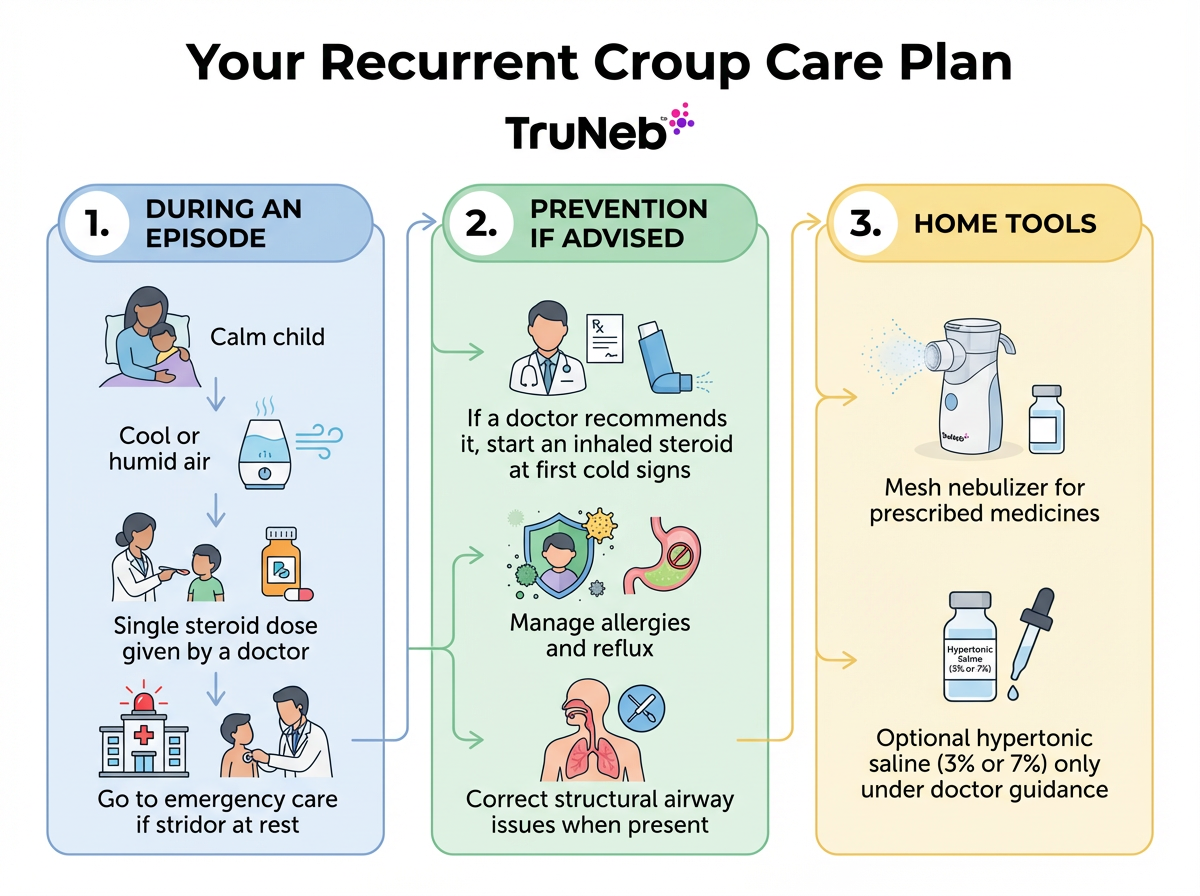
Managing Recurrent Croup and Preventing Future Episodes
During an episode, keep your child calm, offer cool or humidified air, and follow your doctor’s plan. Doctors usually treat croup with a single dose of steroid (like dexamethasone). ⚠️ If your child has stridor at rest, is working hard to breathe, or has blue lips, go to the emergency room right away.
To reduce future episodes, treat the driver. If the pattern points to airway hyperreactivity or asthma, your doctor can prescribe an inhaled corticosteroid (ICS). Starting ICS at the first sign of a cold has been reported, under specialist guidance, to ease recurrent croup in some children without fixed airway problems.
If asthma is confirmed, an action plan with rescue bronchodilators and controller therapy helps prevent wheeze and night cough. Allergies and reflux, if present, should be treated to lower airway irritation. Structural problems can sometimes be corrected by specialists.
At home, tools can make care easier. If your child needs inhaled medicines, a quiet portable mesh nebulizer like the TruNeb™ portable mesh nebulizer can make giving prescribed treatments easier, even at night or during travel. Some doctors also use pre-measured hypertonic saline (3% or 7%) to loosen thick mucus during respiratory infections; this should only be used under medical guidance. ⚠️ Boxes labeled "steam inhaler" are not nebulizers and aren’t meant for breathing prescription medications. Avoid smoke exposure and skip over-the-counter cough syrups that don’t help croup.
Talk to your doctor before trying a new medication.
Addressing the cause can make episodes less frequent.
Frequently Asked Questions
Tap or click a question below to see the answer:
Not necessarily. Recurrent croup raises the chance of an asthma diagnosis, but plenty of kids don’t develop chronic asthma. Talk with your doctor if you notice wheeze or night cough between colds.
Yes. A virus can swell the upper airway (croup) and also trigger wheeze in the lungs (asthma). Doctors treat both — the croup inflammation and the lower-airway bronchospasm.
Spasmodic croup means sudden nighttime barking cough with little or no fever that tends to recur. It ties to a sensitive airway and allergies, which overlaps with asthma-style reactivity. Your doctor can help sort out triggers and a plan.
More than two bouts in a year, croup in an infant under 6 months or in a school-age child, severe or long episodes, or poor response to standard care should prompt a deeper evaluation. Ask about referral to an ENT or pediatric pulmonologist.
In the ER, nebulized epinephrine can quickly ease moderate to severe croup. At home, a nebulizer helps when a doctor prescribes medicines for wheeze or asthma; saline mist can soothe but doesn’t cure croup. Use only the medicines your doctor prescribes for your child.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your child’s symptoms and treatment options.







