On this page

What’s the Difference Between Reactive Airway Disease and Asthma?
Hearing a doctor mention reactive airway disease when you expected to hear asthma can be confusing, especially when it’s about your child or someone you love. Both terms relate to breathing problems, wheezing, and coughing, but they’re not the same. And knowing the difference matters.
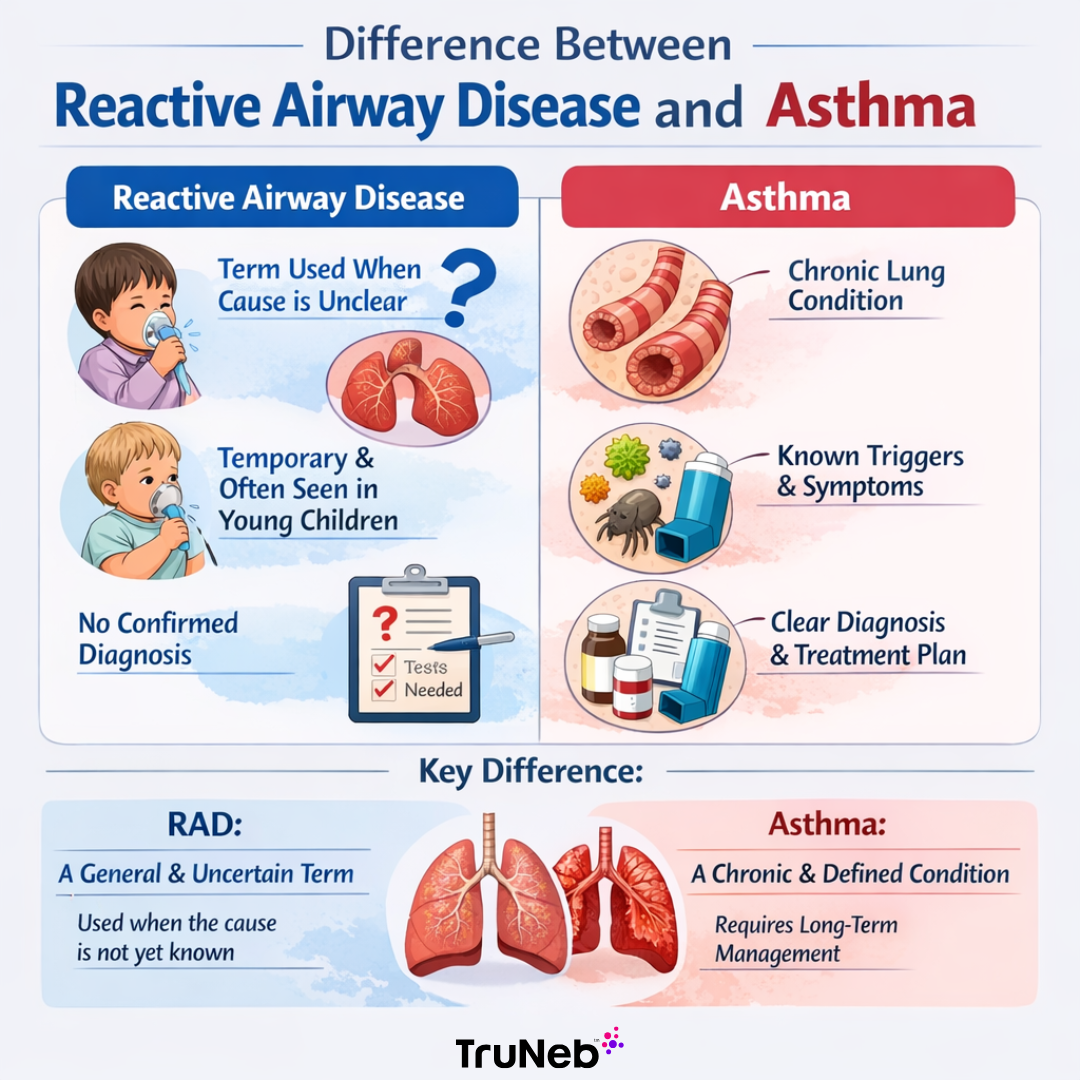
Here’s the short answer: Reactive Airway Disease (RAD) isn’t a specific diagnosis. It’s a general term doctors may use when someone shows asthma-like symptoms, but the cause isn’t clear yet. Asthma, on the other hand, is a well-defined chronic lung condition with known triggers, treatments, and diagnostic criteria. So while RAD is often a temporary label used in early stages - especially in kids - asthma is a chronic condition that requires long-term management.
Understanding this difference can reduce the stress of uncertainty and help you or your child get the right care, faster. Let’s break down what each term means and what it means for your family’s health.
• RAD = Not a diagnosis, often used in young kids
• Asthma = Chronic condition with clear criteria
Reactive Airway Disease is not a formal medical diagnosis. You won’t find it listed in official diagnostic manuals. Instead, it's a placeholder term doctors use when someone shows symptoms like wheezing, coughing, and shortness of breath, but the exact cause isn't clear yet.
Think of it this way: the airways are reacting, but we don't know exactly why.
RAD is most commonly used in young children, especially toddlers. That’s because diagnosing asthma in kids under five can be difficult. Their lungs are still developing, and occasional wheezing doesn't always mean long-term asthma. So, doctors may use "reactive airway disease" as a temporary label while they monitor symptoms or run more tests.
In adults, RAD may come up during sudden breathing problems caused by things like smoke or chemical exposure, especially in urgent care settings, when a full diagnosis can't be made immediately.
Even medical experts use the term cautiously. The American Academy of Allergy, Asthma & Immunology describes RAD as a "highly nonspecific term" with no official clinical definition. In short, it is a description, not a diagnosis.
What Is Asthma?
Asthma is a chronic inflammatory condition that affects the airways and makes breathing more difficult during asthma attacks (a flare up). It causes the airways to become inflamed and create excess mucus . And unlike reactive airway disease, asthma is a well-defined condition with specific diagnosis criteria.
What sets asthma apart is that it involves underlying airway inflammation that doesn’t go away, even when symptoms seem to. That inflammation keeps the airways overly sensitive, so exposure to a trigger—like allergens, cold air, smoke, or exercise—can bring on an asthma attack at any time.
Asthma is also extremely common. In the U.S., it affects about 1 in 12 kids and millions of adults. There are different types of asthma (including allergic, non-allergic, and exercise-induced), but all involve a chronic process that needs long-term management.
RAD vs Asthma: The Differences
Now let’s compare reactive airway disease and asthma side by side—looking at their symptoms, causes, diagnosis, and treatment. They look similar on the surface, but the key differences help with finding the best path forward.
Symptoms: Do RAD and Asthma Feel the Same?
Yes, they absolutely can. It’s easy to see why reactive airway disease (RAD) and asthma get confused. Both can make it harder to breathe and often show up with the same telltale signs.
Shared symptoms:
- Wheezing (a high-pitched whistling sound when breathing out)
- Coughing (especially at night or after physical activity)
- Shortness of breath or difficulty breathing
- Chest tightness or a feeling of pressure in the chest
But the pattern of symptoms is where the difference becomes clear.
With RAD, the symptoms are usually short-lived and tied to a specific trigger. For example, a child might wheeze for a few days after catching a cold. Once the infection passes, the breathing difficulty disappears completely. You might notice symptoms flare up around smoke, dust, or strong smells—but they fade quickly once the irritant is gone. There’s no persistent cough or wheeze between episodes.
Asthma, on the other hand, tends to hang around. Symptoms can be persistent or come back again and again… even without an obvious trigger. For some asthmatics, they only show up during exacerbations, while others deal with daily symptoms. Asthma also tends to worsen at night or early in the morning if not well controlled. The inflammatory nature of asthma means the airways stay sensitive, making flare-ups more likely over time.
Here’s a simple way to think about it:If symptoms only appear in specific situations and go away quickly, it’s likely RAD. If they come back frequently or stick around, asthma is more likely.
RAD episodes can feel just as intense as asthma attacks in the moment. Asthma points to a chronic issue that needs ongoing treatment.
Reactive Airway Disease vs. Asthma
| Reactive Airway Disease (RAD) | Asthma |
|---|---|
| Not a formal diagnosis | Clinically defined medical condition |
| Often used when the exact cause of symptoms is still unclear | Diagnosed based on symptoms, lung function tests, and history |
| Temporary label, especially in young children | Chronic condition that requires long-term management |
| May or may not involve airway inflammation | Always involves underlying airway inflammation |
| Symptoms may resolve or evolve into asthma over time | Symptoms tend to recur and require consistent treatment |
| Commonly used in emergency or pediatric settings | Affects both children and adults |
| No specific treatment guidelines | Managed with inhalers, medication, and trigger avoidance |
Causes & Triggers: Why They Happen
If reactive airway disease and asthma look so similar on the surface, what’s actually setting them off? Turns out, the triggers, underlying causes, and even the way the airways respond tell two very different stories.
What Triggers RAD?
Reactive airway disease (RAD) usually shows up after a short-term event—something sudden that irritates the airways and causes a temporary overreaction. Think of it as your lungs saying, “Hey, that wasn’t normal.”
Some of the most common RAD triggers include:
- Viral infections like a cold or RSV (especially in babies and toddlers)
- Breathing in smoke, dust, or chemical fumes
- Cold air exposure
- Exercise, especially if you’re out of shape or breathing hard in cold weather
With RAD, the key difference is that the reaction often resolves completely once the irritant is gone. There's no evidence of chronic inflammation hanging around. It's more like a reflex—a short burst of breathing difficulty and respiratory symptoms tied to a specific trigger.
In more extreme cases, there’s something called Reactive Airways Dysfunction Syndrome (RADS). It happens when someone inhales a large amount of a toxic irritant (like smoke from a fire or harsh chemicals) and develops asthma-like symptoms immediately after. RADS can last for months, but it typically goes away with time. It still isn’t considered asthma unless the symptoms become long-term.
Why Asthma Is Different
Now let’s look at asthma. Asthma is a condition, not a reaction. The airways are inflamed all the time, even when you feel fine. That’s part of what makes asthma so tricky: the inflammation is always there, sitting beneath the surface, waiting for a trigger to set it off.
And yes, many of the same things that trigger RAD can also trigger asthma attacks:
- Smoke or air pollution
- Allergens like pollen and pet dander
- Dust, cold air, or exercise
- Even a simple cold can provoke a flare-up
But asthma runs deeper. What’s in the air is one thing, how your body responds to it is another. An overactive immune system is thought to play a role. The cause of asthma is usually a combination of genetic predisposition, early-life respiratory infections, and exposure to irritants like tobacco smoke. Obesity and urban pollution have also been linked to asthma risk.
In short: RAD is usually a reaction to something external. Asthma is a condition that lives in your airways every day.
If asthma were a smoldering fire, RAD would be the spark that flares up and fades when the match is gone.
Diagnosis: How Doctors Tell the Difference
When your child is coughing, wheezing, or struggling to breathe, you want answers fast. But telling the difference between asthma and reactive airway disease (RAD) isn’t always immediate, especially in younger children.
Both conditions can start out looking the same. So most doctors begin by reviewing your medical history and doing a physical exam. That helps rule out anything serious and gives them a baseline to monitor symptoms over time.
Why RAD Is Often a Starting Point
If your child is under 5, it’s tough to get clear results from standard lung function tests. For example, spirometry, which measures how much air someone can exhale and how fast, requires a level of coordination most toddlers just don’t have. In fact, most asthma tests cannot provide accurate results in children under 5, so instead of confirming a diagnosis, doctors may use “reactive airway disease” as a placeholder.
That doesn’t mean they’re taking a wild guess, it just means they’re watching closely. If symptoms clear up completely over time, it may have just been a short-term RAD episode. If symptoms keep coming back or get worse, that’s when asthma becomes more likely.
How Asthma Gets Diagnosed Later On
Once a child is old enough—or in adults with recurring symptoms—doctors can run more specific tests to help diagnose asthma:
- Spirometry: Measures lung function before and after using a bronchodilator (like albuterol). If breathing improves, it’s probably asthma.
- Peak flow monitoring: Tracks airflow changes daily, often used by older kids or adults.
- Methacholine challenge: A more advanced test where breathing gets measured after inhaling a substance that causes airway tightening. A drop in lung function confirms airway hyperreactivity.
- Allergy testing: Since asthma is often tied to allergies, skin prick or blood tests may help identify triggers.
- Chest X-ray: Used to rule out other causes like infection, but not to confirm asthma.
If test results aren’t clear or symptoms remain confusing, your primary care doctor may refer you to a pulmonologist, a specialist in lung conditions, for further evaluation.
There’s no single test to confirm reactive airway disease. It’s a diagnosis of exclusion, meaning other possible causes like pneumonia or structural problems have been ruled out. That’s why follow-up and ongoing observation are so important.
It can be frustrating not to have a definite label right away. But giving it time helps your care team get the full picture so your child gets the right support!
Treatment & Management: Short-Term vs Long-Term
The way you treat reactive airway disease versus asthma depends on one big factor: is it a one-time flare-up, or something more persistent?
How Reactive Airway Disease Is Managed
Since RAD isn’t a specific diagnosis, treatment is usually short-term and focused on relieving symptoms quickly. The first step is always to remove or avoid whatever triggered the episode. That could mean stepping away from smoke, treating a viral infection, or avoiding cold air.
Doctors will prescribe a bronchodilator like albuterol or atrovent to help open up the airways. This might come in the form of a nebulizer treatment, especially in urgent care or ER settings when a child is wheezing. Sometimes, a short course of oral or inhaled corticosteroids is used if the episode is more severe and there's airway inflammation.
Most of the time, long-term medication isn’t needed for RAD. If your child improves once the trigger is gone and symptoms don’t return, there’s usually no need for daily treatment. But if episodes keep happening, your doctor may re-evaluate whether it’s actually early-stage asthma and adjust the care plan.
How Asthma Is Treated Over Time
Asthma is a chronic condition, so treatment focuses on keeping symptoms under control every day, not just during a flare-up.
There are two main types of asthma medications:
- Daily control meds: These include inhaled corticosteroids and sometimes leukotriene modifiers like montelukast. They reduce inflammation and help prevent symptoms.
- Rescue meds: These are fast-acting inhalers, like albuterol, used during an asthma attack or before exercise.
For moderate or severe asthma, doctors may recommend combination inhalers, long-acting bronchodilators, or even biologic injections for allergic asthma. Some may also benefit from allergy shots or oxygen therapy in advanced cases.
Avoiding triggers is a big part of managing asthma well. That might mean using dust-proof bedding, keeping pets out of bedrooms, or not smoking around the child. Many families also use an Asthma Action Plan, which is a written plan created with your doctor to track symptoms, adjust medications, and know when to seek help.
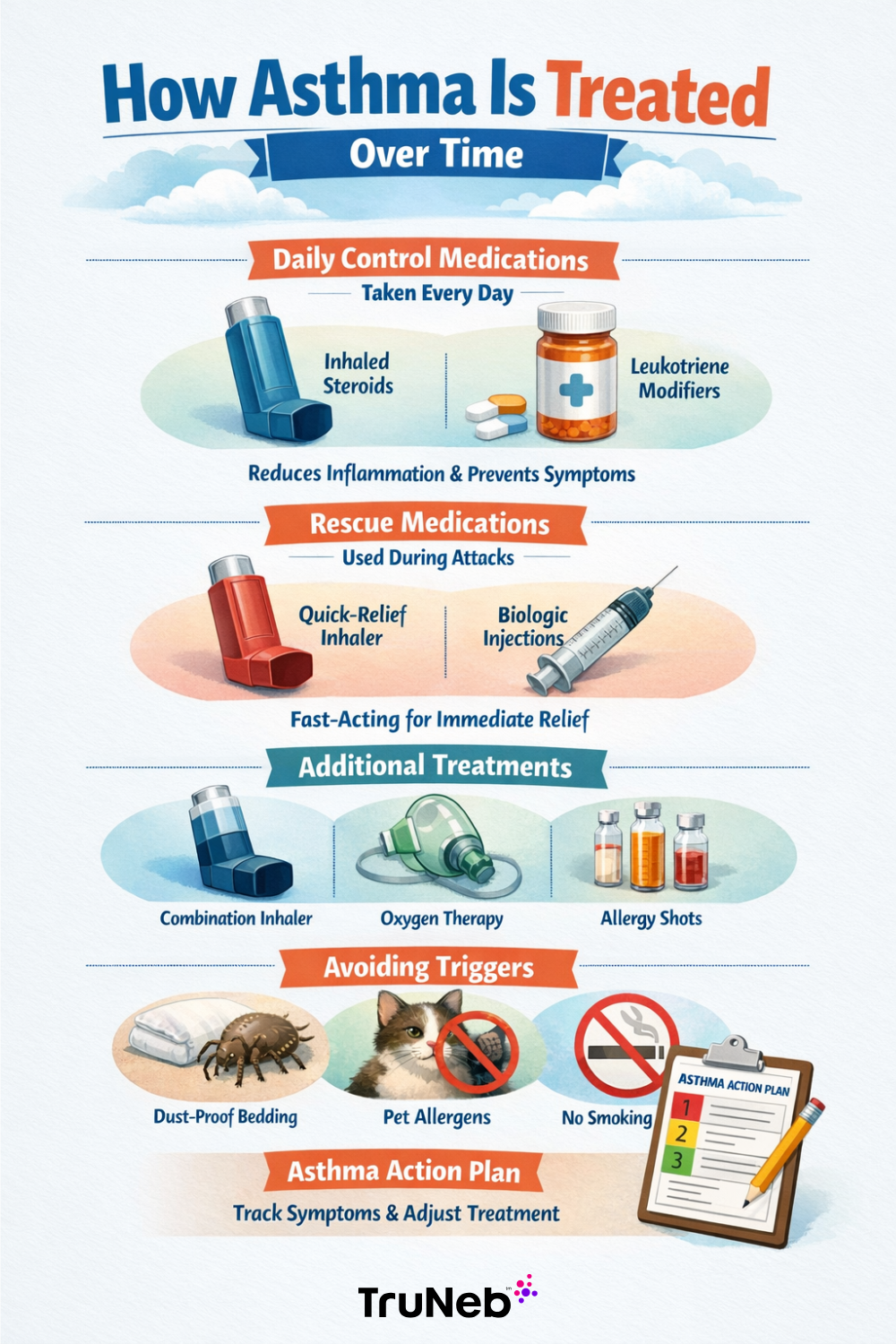
You can also use tools like spacers (which help young kids get the full dose from an inhaler) or nebulizer machines, which turn medication into a fine mist that’s easy to breathe in. These are especially helpful for kids who struggle with inhalers. If you’re looking for more details, we’ve covered almost everything about nebulizers. You can also check out how much nebulizers cost and what types are available.
What’s the Difference in Care?
The main difference is how long you need to manage the condition. A RAD episode might only require treatment for a few days. Once the irritant is gone and breathing improves, no more medication is usually needed. Asthma, on the other hand, calls for a long-term plan to prevent flare-ups, reduce inflammation, and stay ahead of symptoms.
If you or your kiddo keeps needing a rescue inhaler, that could be a sign it’s more than just RAD. Talk with your doctor about starting a daily treatment plan.
Can Reactive Airway Disease Turn into Asthma?
This is one of the biggest questions for parents: if my child has reactive airway disease now, will it turn into asthma later? Or if you’re an adult, does an episode of RAD mean you’re destined to deal with asthma forever?
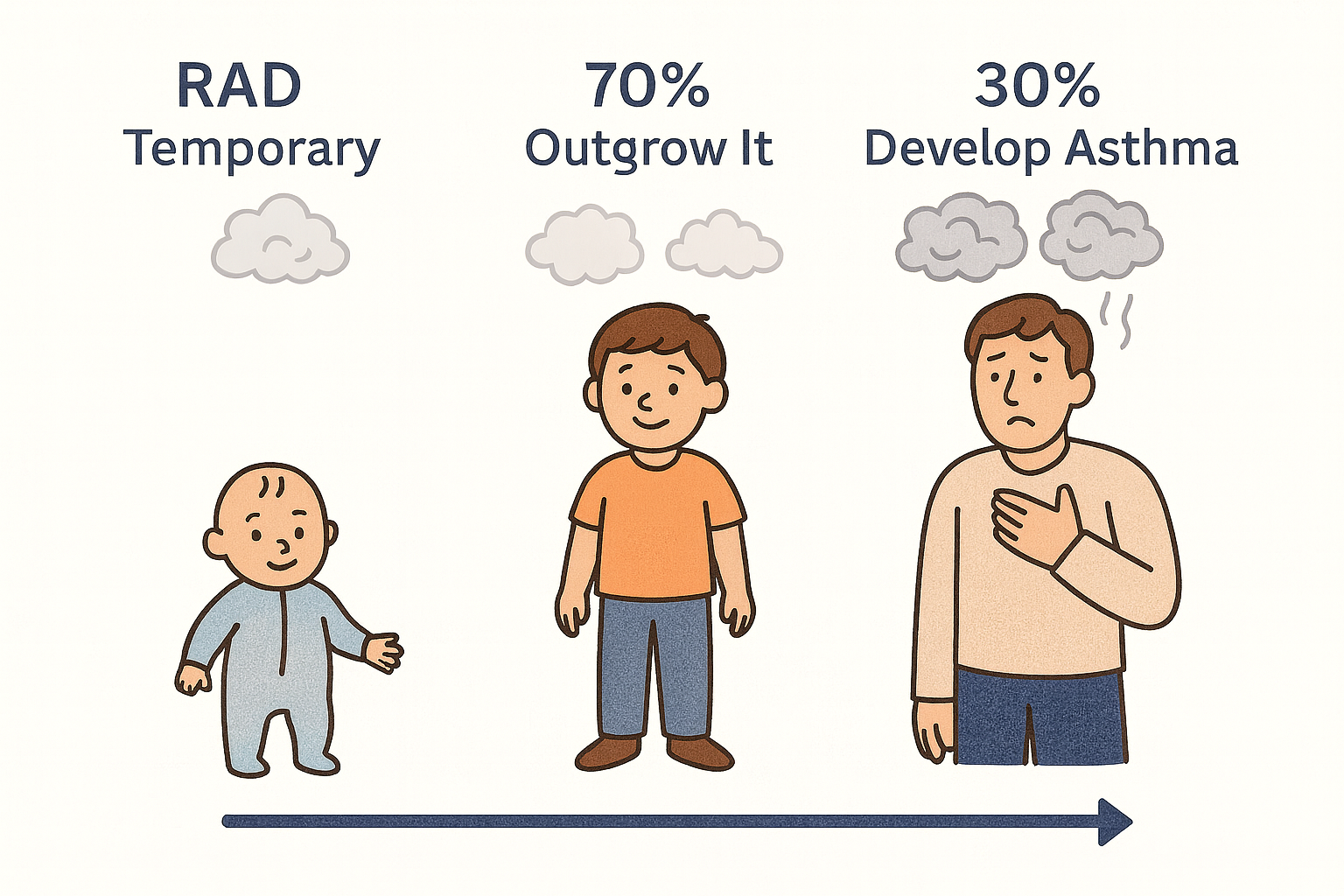
The answer is reassuring: most kids who wheeze early in life do not develop asthma. Yes, it’s possible, but less likely.
The majority of kids outgrow it. As their immune systems mature and airways grow, their symptoms typically disappear, especially if wheezing only happens during viral infections like colds or RSV.
That said, some children do go on to develop persistent asthma. It’s more likely if they also have eczema, allergies, or a strong family history of asthma. Repeated episodes that require emergency care are another red flag. These kids may not just outgrow RAD—they may be showing the early signs of true asthma.
In adults, RAD often comes from a specific occupational exposure or chemical irritant. If symptoms clear up and don’t return, it’s likely a one-time event. But if the airways stay reactive and symptoms keep coming back, doctors may diagnose asthma.
The key is time and monitoring. RAD can be a temporary phase (especially in children). But for others, it’s the first sign of something chronic. Following up with your doctor helps ensure the right prognosis, whether it’s something your child will outgrow or a condition that needs ongoing care.
Living with RAD or Asthma: Tips for Breathing Easier
Whether you’re managing occasional reactive airway episodes or persistent asthma, a few smart habits can make a big difference in how you feel day to day:
- Follow your doctor’s plan: If you’ve been prescribed an inhaler or nebulizer for symptoms, use it exactly as directed. For young children or anyone who struggles with inhalers, a portable nebulizer like TruNeb™ delivers medication as a gentle mist very quietly.
- Avoid your triggers: Watch for what tends to bring on symptoms—smoke, pet dander, pollen, cold air, or exercise—and do what you can to limit exposure. For asthma, this is part of daily management. For RAD, it helps prevent new episodes.
- Monitor your symptoms: Keep a journal or use a peak flow meter (for asthma) to notice patterns. If symptoms get worse or more frequent, let your doctor know. It could be a sign of persistent asthma developing.
- Keep up with follow-ups: Especially with kids, don’t assume they’ll simply outgrow RAD. Regular check-ups help confirm the diagnosis over time.
- Know when it’s an emergency: Seek help right away if you or your child has trouble speaking, seems to be sucking in their stomach to breathe, or develops blue lips. These are signs of a severe asthma attack or reactive airway episode that needs urgent care.
- Stay prepared: Keep your rescue inhaler or portable nebulizer handy, especially if you've had past episodes. Planning ahead brings peace of mind.
Breathing without too much struggle is possible. With the right tools, a little awareness, and the support of your care team, you can stay ahead of symptoms and feel more in control.
FAQs: Quick Answers to Common Questions
Q1: Is reactive airway disease the same as asthma?
No. Asthma is a chronic diagnosis. Reactive airway disease (RAD) is a term doctors use when a patient has asthma-like symptoms like wheezing or coughing, but it’s too early or unclear to confirm asthma.
Q2: What triggers reactive airway disease?
RAD episodes are set off by things like cold viruses, smoke, dust, chemical fumes, cold air, or exercise. These irritants cause the airways to tighten temporarily, leading to cough or wheeze.
Q3: Is RAD a form of asthma?
No, not exactly. Some experts describe asthma as one type of chronic reactive airway disease, but when doctors say “RAD,” they usually mean symptoms that haven’t yet been confirmed as asthma. If symptoms stick around or keep coming back, the label usually changes to asthma.
Q4: How do I know if it’s asthma or just RAD?
Time and testing help sort it out. If the symptoms are ongoing, or if they show a certain pattern over time, doctors may diagnose asthma. If the episode was brief and doesn’t return, it was likely a one-time reactive airway event. Always follow up to get a clear answer.
When to Get Help
It’s not always easy to know when a cough or wheeze is just passing through, or a sign of something more. Here’s how to tell when it’s time to call the doctor, and when it’s time to act fast.
Talk to your doctor if:
- You or your child has repeated episodes of wheezing, coughing, or breathing difficulty, especially after exercise or exposure to triggers like smoke, cold air, or dust.
- The symptoms keep coming back, or don’t fully go away between episodes. This may signal persistent asthma, not just reactive airway disease.
- A child under 5 is having symptoms regularly. They may be too young for formal spirometry, but doctors can still start tracking patterns and adjusting care.
- You’re using a rescue inhaler or nebulizer more often than your care plan suggests. This can be a sign that control medication may be needed.
Go to the ER or call emergency services if:
- Breathing is very hard or fast
- There’s retraction (belly or neck muscles pulling in with each breath)
- The person can’t speak in full sentences
- Lips or fingernails look blue or gray
- The inhaler or nebulizer doesn’t seem to help
Your instincts are there for a reason. If something feels off or you’re not sure what’s normal, it’s always okay to reach out for help. Early treatment makes a big difference, and you don’t have to figure it out alone.