On this page

What Is Pulmonary Rehabilitation and Can It Be Done at Home?
Pulmonary rehabilitation is a program that helps you move, breathe, and feel better with a lung condition. It usually includes breathing techniques, aerobic exercise, strength training, and education.
These exercises can help people living with COPD, asthma, pulmonary fibrosis (ILD), bronchiectasis, cystic fibrosis, and those recovering after COVID.
Yes, most parts of pulmonary rehab can be done at home. Research shows home-based programs can improve exercise capacity and quality of life about as much as center-based programs when done consistently. With steady practice, you can build stamina and improve lung capacity in everyday terms. Your routine can include walking, simple strength moves, daily breathing practice, and, if needed, mucus clearance.
Safety first: ask your doctor if a home plan is right for you, especially if you have severe COPD, frequent flare-ups, low oxygen levels, or heart problems.
Home-based pulmonary rehab can help you build stamina and reduce shortness of breath with simple daily practice.
Home-based pulmonary rehab can deliver gains similar to center-based when done consistently .Use the talk test to keep activity moderate and exhale longer than you inhale with pursed-lip breathing during effort. People with COPD, ILD, bronchiectasis, cystic fibrosis, or post-COVID often benefit; ask your clinician to tailor a plan.
Key Breathing Exercises to Do at Home
These are core techniques taught in pulmonary rehab to control shortness of breath. Breathing exercises help you control breathlessness and use your diaphragm more. Practice these daily. Use them during activity and anytime you feel winded.
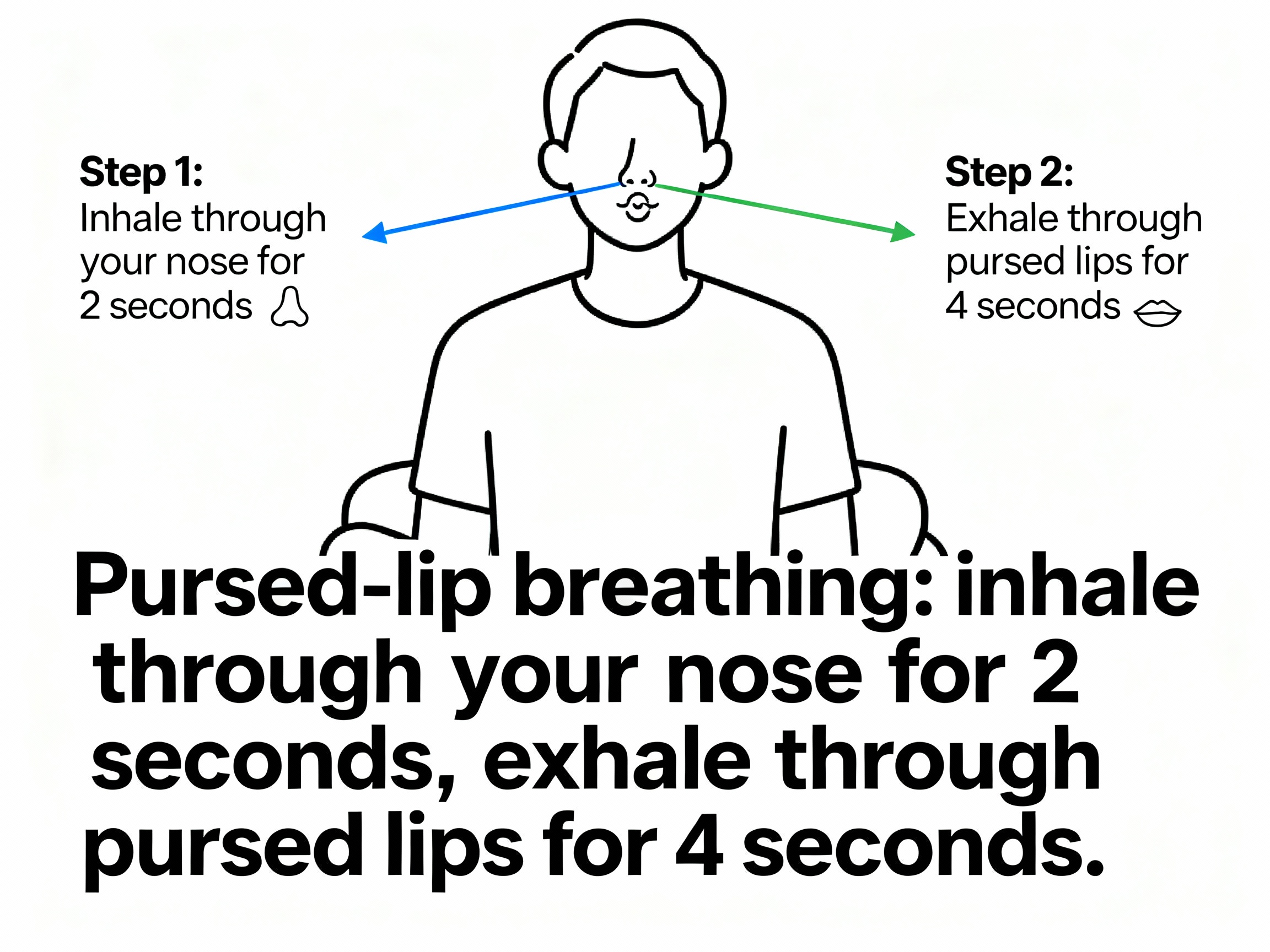
Pursed-Lip Breathing
- Sit tall and relax your shoulders.
- Inhale gently through your nose for 2 counts.
- Purse your lips like you are blowing out a candle.
- Exhale slowly through pursed lips for about 4 counts (exhale longer than you inhale).
- Repeat for 5–10 minutes or until your breathing eases.
How it helps: Pursed-lip breathing keeps your airways open longer and helps clear trapped air, which can reduce shortness of breath during walking, stairs, or chores.
Diaphragmatic (Belly) Breathing
- Lie down or sit comfortably. Place one hand on your upper chest and one on your belly.
- Inhale through your nose so your belly hand rises (your chest hand stays mostly still).
- Exhale slowly through pursed lips while your belly hand falls.
- Practice for 5–10 minutes, 1–2 times per day.
Coordinate breath with effort—inhale before the effort, exhale during the effort (for example, exhale as you stand up or lift).
One-liner: Exhale longer than you inhale to calm your breathing and ease tightness.
Airway Clearance: How to Remove Mucus From Your Lungs
If mucus builds up, clearing it can help you breathe easier and can lower your risk of infection. These airway clearance techniques at home can be part of your routine. Also called chest physiotherapy or lung physiotherapy.
Huff Cough
- Sit up tall. Take a slightly deeper breath than normal.
- Keep your mouth open and use your belly muscles to force air out quickly like you are saying "ha" (as if fogging a mirror). This is a huff.
- Do 2–3 huffs from that breath, then cough to bring mucus up and spit it out if needed.
- Rest and repeat as needed.
Why it works: Huffing moves mucus from smaller to larger airways with less strain than hard coughing.
Simple Postural Drainage Positions
- Side-lying: Lie on your side with a pillow under your hips so your chest is a bit lower than your hips. Breathe slowly for 5–10 minutes, then use huff coughs.
- Seated forward: Sit and lean forward onto pillows on a table. Relax, breathe, then huff cough.
Helpful add-ons: Stay well hydrated. Using your prescribed bronchodilator before clearance can make it easier. Some people also use positive expiratory pressure (PEP) devices or an incentive spirometer if recommended. Some people are taught ACBT (Active Cycle of Breathing Technique) by a respiratory therapist; if you've learned it, use it at home as instructed. An inspiratory muscle training device can be helpful if your doctor recommends one.
One-liner: Use gravity, slow breaths, and huff coughs to move and clear mucus without exhausting yourself.
At-Home Endurance Exercises for Better Breathing
Warm up for 3–5 minutes at an easy pace, cool down the same way after. Aerobic activity trains your heart and lungs so daily tasks feel easier. Go at a pace where you are a bit breathless but can still talk in short sentences. These activities improve exercise tolerance over time.
Walking
- Start with what you can: even 5 minutes around your home counts.
- Use the "talk test" to keep it moderate. If you can't speak at all, slow down.
- Try to add 1–2 minutes every few days.
- Aim to build toward 20–30 minutes most days. You can split time into 2–3 shorter walks.
Use pursed-lip breathing while walking (for example, exhale every 2–3 steps) to stay in control.
Other Simple Options
- Stationary cycling or pedal exerciser: start 5–10 minutes at low resistance.
- Light dancing or marching in place with music.
- Swimming or water exercise if available and approved by your doctor.
One-liner: A little movement most days adds up to better stamina and fewer breathless moments.
Strength Training Exercises for Lung Health
Stronger muscles use less oxygen to do the same job. That means less huffing and puffing with chores. Don't hold your breath—exhale during the hardest part of the movement.
Lower Body
- Sit-to-stand: From a sturdy chair, feet hip-width. Lean slightly forward, stand up, then sit down slowly with control. Do 5–10 reps. Exhale as you stand.
- Calf raises: Hold the chair. Rise onto toes, then lower. Do 8–10 reps.
Upper Body
- Bicep curls: Use light dumbbells or water bottles. Curl up as you exhale, lower slowly. Do 8–10 reps.
- Wall push-ups: Hands on wall at shoulder height, step back. Bend elbows to lean in, then push away. Do 8–10 reps.
Core and Posture Support
- Seated torso rotations or gentle chest-opening stretches to keep the ribcage and shoulders moving well.
Do strength training 2–3 days per week (non-consecutive). When 10 reps feel easy, add a few more reps or slightly heavier weight.
One-liner: Two short strength sessions a week can make stairs, lifting, and carrying feel easier.
Sample Weekly Plan
| Day | Plan | Notes |
|---|---|---|
| Mon | 10–15 min walk + 5 min pursed-lip breathing | Keep it moderate (talk test). |
| Tue | Strength: sit-to-stands, wall push-ups, curls (1–2 sets of 8–10) | Exhale during the effort. |
| Wed | 12–18 min walk or pedal exerciser | Split into two short sessions if needed. |
| Thu | Strength (same as Tue) + chest/shoulder stretches | Move slow and controlled. |
| Fri | 15–20 min walk + belly breathing 5 min | Add 1–2 minutes if you feel okay. |
| Sat | Light activity (dance/march) 10–15 min + huff coughs if congested | Use pacing; take breaks. |
| Sun | Rest or gentle stroll + relaxation breathing | Recovery helps progress. |
This simple weekly plan blends endurance, strength, and breathing practice so you can build stamina week by week. Adjust times based on your energy and symptoms.
Safety Tips and Staying Motivated
Exercise Safely at Home
- Warm up and cool down for 3–5 minutes at an easy pace.
- Stop and rest if you have chest pain, dizziness, or severe breathlessness that doesn't settle with pursed-lip breathing.
- Avoid breath-holding (Valsalva). Exhale during the hardest part of any movement.
- If you feel breathless, try a recovery position: lean forward onto a table or place your hands on your thighs while seated or standing.
- If you use oxygen, wear it as prescribed during exercise and keep tubing clear to prevent tripping.
- Keep your rescue inhaler nearby if your doctor has prescribed one. Use it as directed.
- Choose a clutter-free, well-lit space. Avoid extreme heat, cold, or poor air quality.
- Consistency beats intensity. Small, regular sessions help more than rare, hard ones.
⚠️ If you have severe chest pain, confusion, fainting, blue lips/face, or worsening shortness of breath that doesn't improve with rest and your usual medicines, call emergency services.
Stay Motivated
- Set tiny goals (add 2 minutes of walking this week). Track time and reps in a simple log.
- Pair exercise with music or a favorite show.
- Ask a friend to check in, or join an online COPD community for support.
Note: Talk to your doctor before trying a new medication or changing how you use prescribed treatments.
One-liner: Go slow, be steady, and celebrate small wins—they add up.
When to Seek Professional Help
Home rehab works well for people with chronic lung disease, but some situations need extra support.
- Talk with your doctor before starting if you have severe COPD, frequent flare-ups, very low oxygen levels, or heart issues.
- Ask about a formal pulmonary rehab program if you feel stuck, your symptoms are getting worse, or you want supervised training and education.
- Ask your doctor about virtual rehab options if travel is hard.
- Get urgent care if you have severe chest pain, fainting, or breathing trouble that doesn't improve with rest and your usual medicines.
Studies show home-based rehab can match center-based results when it's consistent and safe.
One-liner: If you aren't improving after a few weeks, ask your care team for a referral or virtual rehab options.
If you use inhaled medicines before exercise or airway clearance, a portable nebulizer can make it easier to take your dose anywhere. Use medications as prescribed.
Note: Steam inhalers aren't nebulizers and aren't for breathing medications.
Always follow your doctor's instructions.
Frequently Asked Questions
Tap or click a question below to see the answer:
Yes. Many people benefit from home-based programs and see better stamina and less breathlessness when they practice consistently. Studies report similar gains to center-based rehab for patients who stick with it.
Aim for aerobic activity most days (work toward 20–30 minutes), strength training 2–3 days per week, and breathing exercises daily. Break sessions into shorter blocks if needed.
A sturdy chair, comfortable shoes, and light weights (or water bottles) are enough to start. A pedal exerciser or stationary bike is optional. A pulse oximeter can be helpful if your doctor wants you to monitor oxygen at home.
A lot of people notice progress in a few weeks. After 6–8 weeks of steady practice, daily tasks usually feel easier and recovery is quicker.
Yes. Airway clearance methods such as huff coughing and simple drainage positions can help move and clear mucus at home.