On this page

Why Postnasal Drip Makes You Cough More at Night
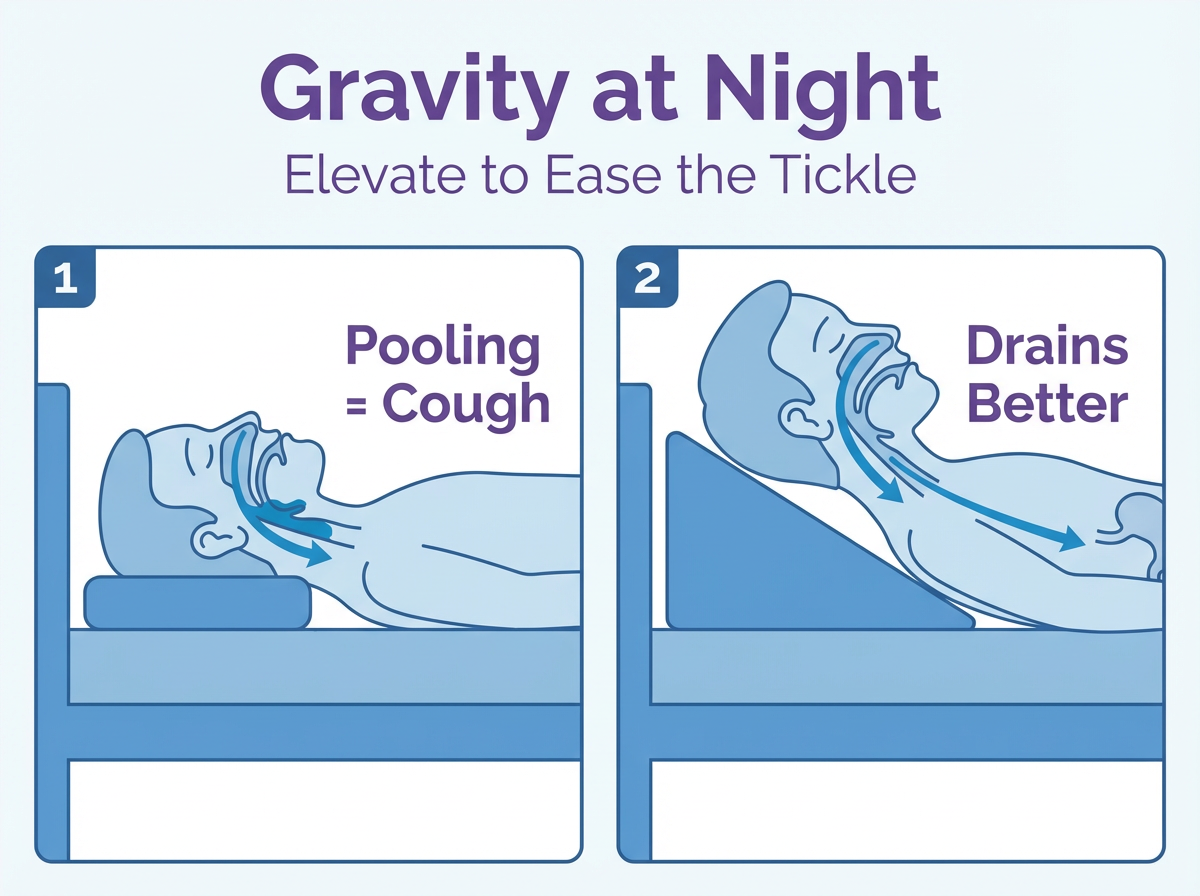
At night, gravity works against you. When you lie flat, mucus that drained fine during the day can pool in the back of your throat. That tickle lights up cough sensors and starts the coughing cycle. This is the classic post nasal drip cough at night.
Your body also clears mucus more slowly while you sleep. Tiny hairs in your nose and sinuses (cilia) don’t sweep as fast, and you swallow less frequently. The result is more mucus sitting where it irritates your throat.
Raise your upper body and keep your airways moist to reduce the tickle. Even a small incline can help mucus move down into your stomach instead of into your airway.
Key point: Lying flat lets mucus collect in your throat, which triggers a night cough.
Is It Postnasal Drip or Something Else?
Postnasal drip is a common cause of a stubborn cough, and it usually feels worse at night. You might feel a lump or tickle in your throat and need to clear it.
Asthma usually adds wheezing, chest tightness, or shortness of breath. That’s a lower-airway squeeze, not throat drip. Bronchitis brings chest mucus and an all-day, chesty cough.
Acid reflux (GERD) can also spark a night cough. A sour taste, heartburn, or coughing after lying down points to reflux. Sometimes reflux is silent, but the throat still gets irritated.
You can have postnasal drip without a runny nose. Thick mucus can drain only backward and show up as throat clearing and coughing.
One-line takeaway: A night cough with a throat tickle but no chest tightness or wheezing is more likely from postnasal drip than from asthma or bronchitis.
Common Triggers That Make Postnasal Drip Worse at Night
Allergies: Dust mites in bedding, pet dander on pillows, and bedroom mold are top night triggers. If allergies drive your symptoms, you’ll notice more drip after you get in bed.
Sinus infections and colds: Thick, sticky mucus lingers and is harder to clear when you lie down. Chronic sinus swelling can keep the drip going.
Dry indoor air: Heated winter air or very dry indoor air thickens mucus, so it moves slowly and irritates your throat.
Structure: A deviated septum or nasal polyps can block normal drainage. You might notice one side always feels more plugged.
Late-night eating and reflux: Eating or drinking alcohol near bedtime can lead to acid in the throat when you lie down. That irritation can mimic or worsen postnasal drip.
Some blood pressure medicines (ACE inhibitors) and pregnancy-related nasal swelling can also increase postnasal drip—ask your doctor if this could be part of your symptoms.
One-line takeaway: At night, allergies, sinus infections, dry air, structural nose issues, and reflux are the main triggers that turn postnasal drip into a worse cough.
Nighttime Relief Plan: Immediate Things to Do Before Bed
Here’s a simple plan you can use tonight to calm a postnasal drip cough.
- Add moisture. Run a bedside humidifier or take a steamy shower to loosen and thin mucus. You might see products labeled "steam inhaler" near nebulizers. These are not nebulizers and aren’t designed for breathing liquid medications.
- Elevate and position. Sleep with your upper body on a wedge or extra pillows. Side sleeping can help reduce throat drip.
- Cut triggers. Use dust-mite covers, keep pets off the bed, and avoid smoke and strong scents in the evening. If reflux is part of your symptoms, avoid heavy meals or alcohol close to bedtime.
- Soothe the throat. Sip warm, caffeine-free tea with honey, keep water by the bed, and consider a saltwater gargle.
Rinse with saline. Using a neti pot or squeeze bottle with sterile saline 15–30 minutes before bed can help clear the drip at the source.
One-line takeaway: Clearing mucus, adding moisture, and sleeping slightly elevated work together to calm a postnasal drip cough at night.

Hydrate and Thin the Mucus: Nebulizer Night Relief
A saline nebulizer for post nasal drip gives your nose and throat a fine mist that coats, hydrates, and helps thin sticky mucus. It’s like focused humidity where you need it most.
You can use sterile normal saline (0.9%). Your doctor might recommend hypertonic saline (3% or 7%) if swelling and thick mucus are a big problem. Hypertonic saline isn’t right for everyone, so get your doctor’s guidance before trying it. Always use sterile saline and follow device directions.
A portable mesh nebulizer like the TruNeb™ portable mesh nebulizer turns saline into a fine mist you can use at your bedside for 5–10 minutes before sleep. People often say breathing feels clearer right after a session.
This is drug-free support you can add to the rest of your plan.
One-line takeaway: A saline nebulizer gently coats your nose and throat with a fine mist that hydrates tissues and thins mucus for easier breathing at night.
Smart Medication Choices for Nighttime Postnasal Drip
Medicines can help, but they work best when you match them to the cause.
If you’re deciding between an antihistamine vs decongestant for postnasal drip, think about what’s really driving your symptoms.
Antihistamines help allergy-driven drip. Older, sedating options (like diphenhydramine) can dry mucus and make you drowsy. Non-drowsy options (like loratadine or cetirizine) ease allergy symptoms with less next-day fog.
Decongestants shrink swollen nasal tissue. Pills (like pseudoephedrine) can open you up but can keep you awake if taken late. Nasal decongestant sprays (like oxymetazoline) work fast, but do not use them more than 3 days in a row to avoid rebound congestion.
Nasal steroid sprays (like fluticasone or mometasone) reduce inflammation when used daily. They are not instant, but they are one of the most effective long-term tools for chronic drip.
Expectorants (like guaifenesin) can make thick mucus looser. A cough suppressant (like dextromethorphan) can help you sleep on a rough night, but it does not treat the cause.
Key point: Match the medicine to the driver (allergies, stuffiness, or ongoing inflammation) and use the simplest plan that works for you.
Safety note: Always follow the directions on the package and ask your doctor or pharmacist if you’re not sure what’s safe with your other medicines. Use cough suppressants only for short-term sleep support and only as directed on the label.
When to See a Doctor and Why It Matters
If you try the steps above for a couple of weeks and your night cough still disrupts sleep, it’s time to check in with a doctor. A doctor can help you build a targeted plan for allergies, chronic sinusitis, or reflux.
Get care sooner if you notice red flags: high fever or severe sinus pain, thick green or yellow mucus lasting more than a week, or blood in mucus. Wheezing or shortness of breath, chest pain, hoarseness that lasts over two weeks, weight loss, or a cough that lasts longer than eight weeks also deserve prompt evaluation.
⚠️ If you have severe trouble breathing, chest pain, confusion, or blue lips or face, call 911 or seek emergency care right away.
An ENT can look for blocked drainage (polyps, deviated septum) and chronic infection. Allergy testing can confirm triggers. If reflux is suspected, treatment for GERD can reduce night coughs.
You don’t have to power through sleepless nights. Help is available.
One-line takeaway: If your night cough doesn’t improve after a couple of weeks of home care or you notice any red-flag symptoms, it’s time for a doctor to look for allergies, sinus disease, reflux, or other causes.
Nighttime Postnasal Drip Relief: Checklist and Troubleshooting
Use this quick checklist on flare nights.
One-line takeaway: This checklist turns your whole night relief plan into quick steps you can run through whenever postnasal drip flares up.
- Do a saline rinse 15–30 minutes before bed. Clear the drip at the source.
- Set your room: run a humidifier, keep it clean, and keep pets off the bed.
- Elevate your upper body with a wedge or extra pillows; try side sleeping.
- Choose medicine based on your cause and time of day, and follow your doctor’s or the package directions. Avoid decongestants late if they keep you up.
- Soothe your throat: warm tea with honey now; water by the bed for wake-ups.
- Optional: a brief saline nebulizer session to hydrate and thin mucus.
- If you wake coughing, sit up, sip water, and reset your elevation. Most tickles settle in minutes.
If this keeps happening or you notice warning signs, call your doctor.
Frequently Asked Questions
Tap or click a question below to see the answer:
Think in three pillars: clear mucus, add moisture, and use gravity. Do a saline rinse before bed, sleep with your head and upper body slightly elevated (wedge or extra pillows), and use a humidifier if your room is dry. Sip water if you wake coughing. If allergies drive your symptoms, an evening antihistamine can help. Talk to your doctor before starting any new medicine.
Sleep on your side or on your back with your head and torso elevated on a wedge or extra pillows. Avoid lying flat. Elevation helps mucus drain to your stomach instead of pooling in your throat.
Yes. Thick mucus can drain only backward, so you notice throat clearing and coughing without a visible runny nose. Dry indoor air and silent reflux can also make it feel like mucus is stuck in your throat.
Usually, yes. Dry air thickens mucus and irritates your throat. A bedside humidifier keeps mucus looser and your throat more comfortable. Aim for moderate humidity and keep the unit clean.
Match it to the cause. Antihistamines help allergy symptoms, decongestants open a stuffy nose (but can keep you awake if taken late), and daily nasal steroid sprays reduce long-term nasal swelling. Use cough suppressants only for short-term sleep support and only as directed on the label. Talk to your doctor before trying a new medication.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk to your doctor about your symptoms and before starting or changing any treatment.