On this page
Urgent Note: Chest Pain Needs Fast Attention
If you have new, severe, or unexplained chest pain, seek emergency care now.
Chest pain can come from the lung lining (pleurisy) or the chest wall joints (costochondritis). This guide explains the difference so you can talk clearly with your doctor.
Treat any new, severe, or unexplained chest pain as an emergency before self-diagnosing.
Talk to your doctor before trying a new medication.
⚠️ Disclaimer: This article is for informational purposes only and isn’t a substitute for professional medical advice, diagnosis, or treatment. Always talk to your doctor about your symptoms and any treatments you’re considering.
Pleurisy and Costochondritis Basics
What Is Pleurisy?
Pleurisy is inflammation of the thin lining around your lungs and inner chest wall. It causes sharp pain that gets worse when you take a deep breath, cough, or sneeze.
What Is Costochondritis?
Costochondritis is inflammation where your ribs meet your breastbone. It causes front-of-chest pain that is tender when you press the spot. Movements of your upper body can also flare it. It’s a common, usually harmless cause of chest wall pain but can feel scary because it mimics more serious problems.
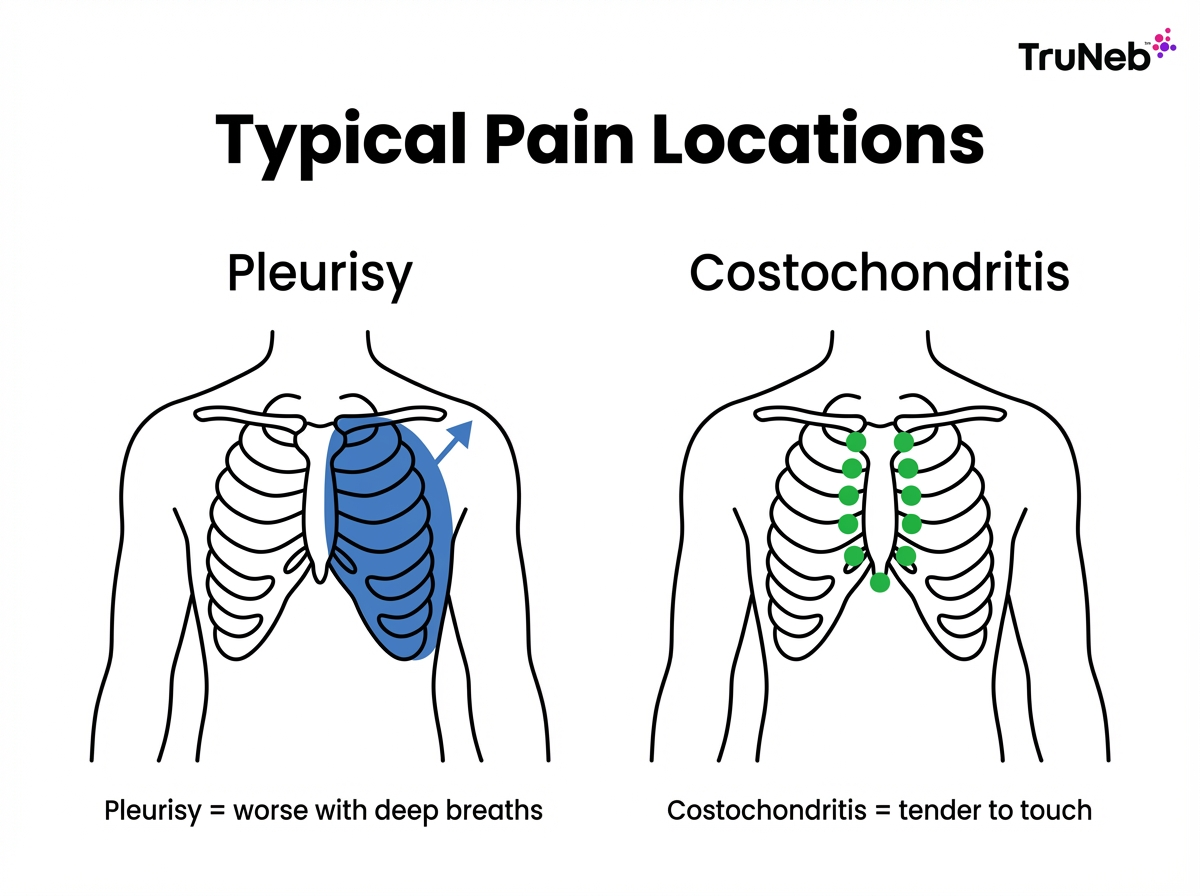
In one line: pleurisy hurts with breaths, and costochondritis hurts to the touch.
Symptoms: Pleuritic Pain vs Chest Wall Pain
Pleurisy typically causes a sharp, stabbing pain on one side of the chest or toward the back. It spikes with deep breaths, coughing, or sneezing. You might start breathing shallowly to avoid the pain.
Costochondritis usually causes sharp or aching pain near the breastbone. Pressing the sore rib joint reproduces the pain. Certain arm or trunk movements can make it worse.
Key takeaway: if deep breaths are the main trigger, think pleurisy; if pressing the spot sets it off, think costochondritis.
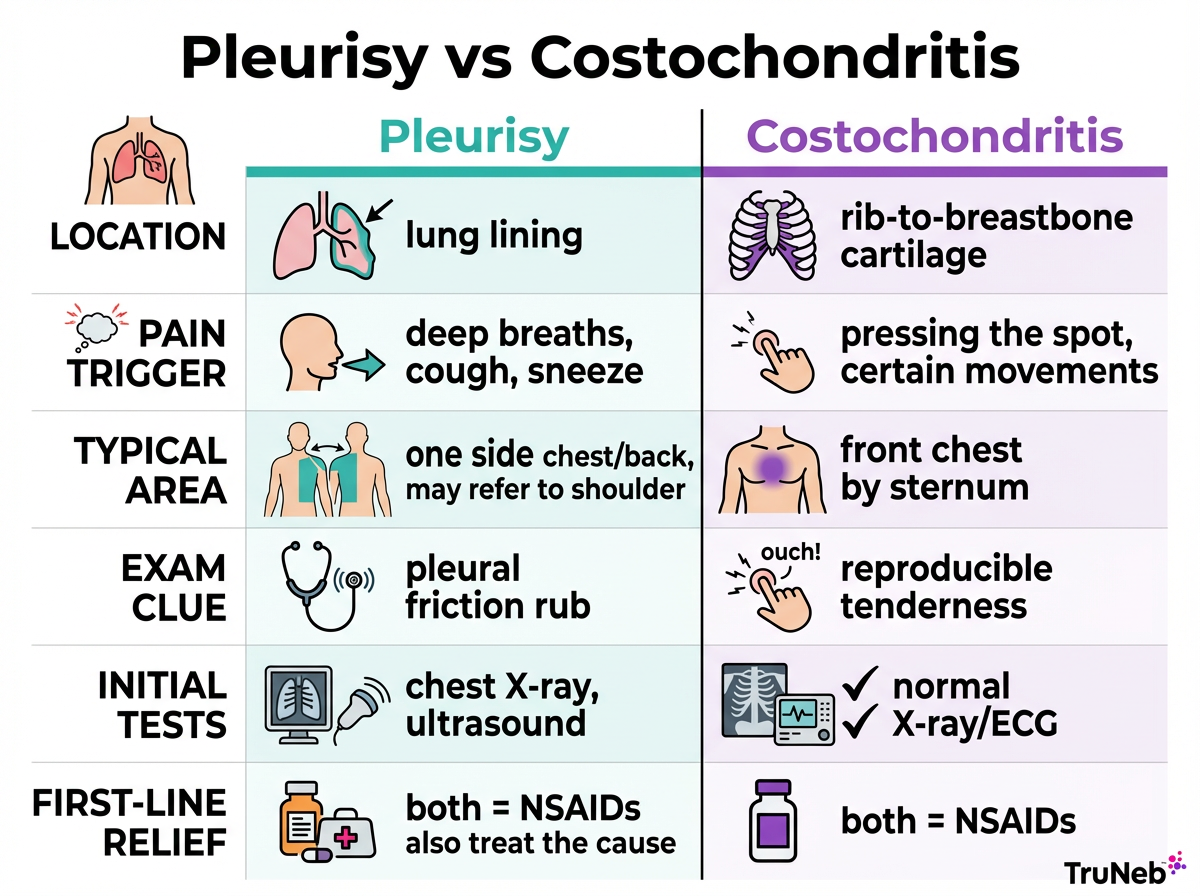
| Category | Pleurisy | Costochondritis |
|---|---|---|
| Pain location | One side chest or back, can spread to the shoulder tip. | Front of chest along the sternum. |
| Main trigger | Deep breaths, cough, sneeze. | Pressing the spot, certain movements. |
| Exam clue | Possible pleural friction rub. | Reproducible point tenderness. |
| Other signs | Cough or fever if infection. | Usually no fever, normal breathing sounds. |
| What helps | Holding a pillow against the chest when coughing, lying on the painful side. | Resting the area, posture care. |
| Common tests | Chest X-ray, sometimes ultrasound or CT. | Normal X-ray and ECG. |
Costochondritis pain can also sting with deep breaths because the chest wall moves, but the hallmark is tenderness you can reproduce by pressing the spot.
Causes and Risk Factors: Why They Happen
Pleurisy is usually a reaction to something that irritates the pleura. Common causes include viral infections, bacterial pneumonia, and less commonly tuberculosis. It can also happen with autoimmune diseases like lupus or rheumatoid arthritis. Doctors also think about lung blood clots (pulmonary embolism) or cancer if your symptoms and risk factors suggest it.
Costochondritis is usually idiopathic, meaning no single clear cause. It can follow heavy lifting, a bad cough, minor chest strain, or poor posture. It can show up with some musculoskeletal conditions and, rarely, with arthritic disorders. It isn’t caused by heart attacks or most lung infections, which is why doctors rule those out first. Very rarely, it can be infectious, especially after chest surgery or with IV drug use.
Think of it this way: pleurisy follows problems inside the chest, while costochondritis is a chest wall strain.
Diagnosis: How Doctors Tell Them Apart
Your doctor listens to when the pain happens, what worsens it, and what else you feel. Then they examine your chest.
If pressing a rib joint reproduces the pain and your heart and lung tests are normal, costochondritis is likely. If deep breaths and coughing are the main triggers, they look for pleurisy.
Common tests are a chest X-ray to look for pneumonia or fluid and an ECG to rule out a heart problem. Blood tests and, if needed, ultrasound or CT can follow based on your risk. Doctors usually diagnose costochondritis after they’ve ruled out heart and lung emergencies with tests.
Short version: normal ECG and X-ray plus point tenderness suggest costochondritis, while lung or pleural findings point to pleurisy.
Red Flags: When to Go to the ER or Doctor’s Office
Go to the ER now if chest pain comes with any of these:
- Severe or worsening shortness of breath, fainting, heavy sweating, or pain spreading to the arm, jaw, or back.
- High fever or shaking chills, or coughing up yellow-green mucus or blood.
- New chest pain after long travel or surgery, or with leg swelling (possible blood clot).
Call 911 (or your local emergency number) right away if any of these occur.
If your pain is mild, clearly tender to touch, and you feel well otherwise, a same-day or next-day clinic visit is reasonable.
⚠️ If you’re ever unsure whether chest pain is an emergency, treat it as one and get urgent care.
Key point: when you’re unsure about chest pain, it’s safer to seek urgent medical evaluation than to wait.
Costochondritis Treatment: Easing Chest Wall Pain at Home
- You can usually ease costochondritis by resting the area for a few days and avoiding moves that trigger pain. If a cough set it off, manage the cough and stay hydrated.
- People are often advised to use ice packs for short periods (around 15–20 minutes with a cloth barrier) in the first 48 hours, then switch to a warm pack to relax tight muscles—ask your doctor if this is safe for you.
- Short-term pain relievers, such as NSAIDs like ibuprofen or naproxen, are commonly used if they’re safe for you. If NSAIDs aren’t an option, acetaminophen can help.
- Mind posture and add gentle chest stretches once pain eases.
- See your doctor if pain is severe, lasts beyond a few weeks, keeps coming back, or if your symptoms change.
Bottom line: rest, ice or heat, and short-term NSAIDs usually calm costochondritis chest wall pain within days to weeks.
Talk to your doctor before starting or changing any medication or exercise routine.
Pleurisy Treatment: Medical Care and Home Relief
Treating pleurisy means treating its cause. Doctors manage infections with the right medicine, calm autoimmune flares, and drain large fluid collections when needed. For pain, NSAIDs are usually a first-line option. Doctors sometimes add other pain control if needed.
At home, protect your breathing. Many people feel better holding a pillow against the painful side when they cough. Practice gentle deep breathing as you can to keep the lungs open. Rest, hydrate, and use humidified air to ease irritation.
A nebulizer doesn’t treat pleurisy itself, but it can help thin mucus and make coughing less painful as part of your overall plan. If your pleurisy comes with thick mucus or a tough cough, a portable mesh nebulizer like the TruNeb™ portable mesh nebulizer can deliver saline mist to support comfort while your main treatment works. Use only solutions your doctor recommends in a nebulizer.
⚠️ You might see products labeled "steam inhaler" near nebulizers. These are not designed to deliver prescription breathing medicines and don’t replace a nebulizer.
Bottom line: treat the cause, control pain, and support breathing. A portable nebulizer can help cough-related discomfort in pleurisy.
Talk to your doctor before starting or changing any medication or nebulized solution.

Frequently Asked Questions
Tap or click a question below to see the answer:
Pleurisy is pain from the lining around your lungs that gets worse when you breathe in or cough. Costochondritis is pain where the ribs meet the breastbone that flares when you press on the spot or move your chest. If you’re unsure which one you have, see your doctor.
It doesn’t cause true lung shortness of breath, but deep breaths can hurt, so you might end up breathing shallowly and feel winded. If you have real trouble breathing, get checked to rule out lung or heart causes.
They match your symptoms and exam, then use tests. A chest X-ray checks for pneumonia or fluid. An ECG looks for heart problems. Point tenderness with normal tests supports costochondritis.
Follow your doctor’s plan. NSAIDs for pain, rest, pillow splinting when you cough, gentle breathing exercises, hydration, and humidified air can help. If mucus is heavy, your doctor might recommend saline with a portable nebulizer, such as TruNeb, to ease cough.
Most cases improve in days to a couple of weeks with rest and anti-inflammatory care. If it lasts longer or is severe, see your doctor.
It’s uncommon but possible, especially with underlying inflammatory conditions. Doctors will check both the chest wall and lungs if your pain has mixed features.
Heart attack pain typically feels like pressure or tightness and can spread to the arm, jaw, or back with sweating, nausea, or shortness of breath. Costochondritis is usually pinpoint, tender to touch, and worsens with certain movements. If you’re unsure whether your pain is a heart attack or costochondritis, treat it as an emergency and seek immediate care.







