On this page
Panic Attack vs Asthma Attack: Quick Differences
If you're trying to tell a Panic Attack vs Asthma Attack apart fast, start here.
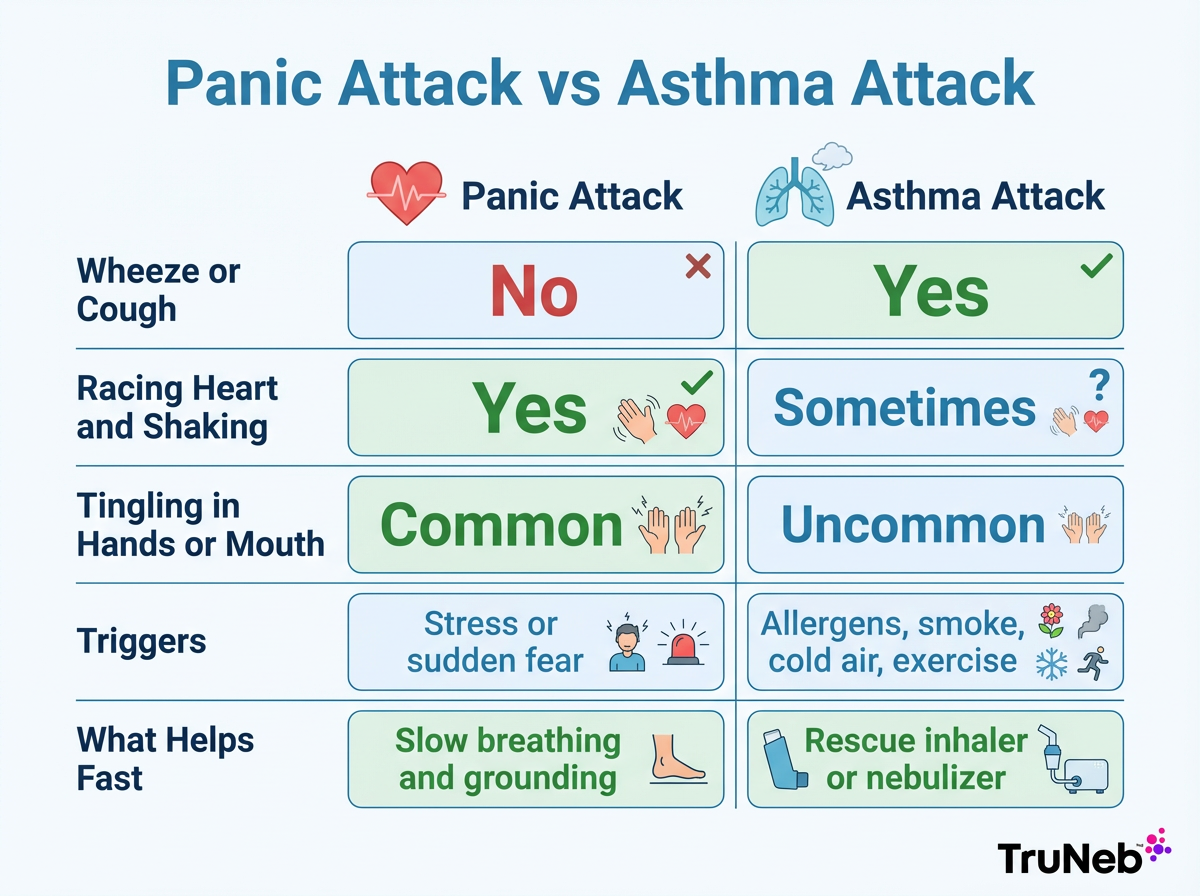
Here is the quick way to sort it out.
- Wheeze or cough points to asthma. A high-pitched whistling sound when you breathe out is common in asthma.
- Racing heart, shaking, sweating, or tingling in fingers or around the mouth points to panic.
- Triggers help. Allergens, smoke, cold air, or exercise suggest asthma. A surge of stress or a fear spike suggests panic.
- Notice what tends to bring relief. A rescue inhaler or a nebulizer can ease asthma symptoms quickly when it's an asthma flare. Slow breathing and grounding can help panic symptoms settle.
- Watch for danger signs. Blue lips or nails, severe trouble speaking, or a silent chest mean an asthma emergency — follow your emergency asthma plan and call 911.
⚠️ Emergency warning: Call 911 or seek emergency care right away if you notice blue lips or nails, a silent chest, severe trouble speaking, or if your breathing suddenly gets much worse.
Quick comparison: wheeze and relief from asthma medicine point to an asthma attack, while a racing heart and relief from calming techniques point to a panic attack.
| What you notice | Panic attack | Asthma attack | What usually helps |
|---|---|---|---|
| Breathing sounds | No wheeze | Wheeze or cough | Asthma meds for asthma; slow breathing for panic |
| Heart and body | Racing heart, shaking, sweating | Can feel tired or tight; heart rate changes aren't the main feature | Grounding and paced breathing for panic; rescue medicine for asthma |
| Tingling | Common in fingers/lips | Uncommon | Slow, longer exhales |
| Typical triggers | Stress or sudden fear | Allergens, smoke, cold air, exercise | Avoid triggers; follow your action plan |
| Response | Calming techniques ease symptoms | Rescue inhaler or nebulized medicine can improve breathing | Use the plan you made with your doctor |
| Danger signs | Fainting, chest pain—seek care | Silent chest, blue lips/nails, severe trouble speaking—call 911 | Emergency care for severe signs |
Note: Patterns guide quick decisions but don't diagnose—always follow your doctor's advice.
Example: If you feel chest tightness with wheeze and your inhaler helps, that's more consistent with an asthma attack. If your chest feels tight but you also have a pounding heart, shaking, and tingling, that's more consistent with a panic attack.
Safety note: If you're not sure, follow the asthma action plan you made with your doctor (which usually includes using your rescue medicine), then start calming breaths. Call 911 if your breathing isn't improving.
Key takeaway: Asthma narrows your airways; panic is a body alarm. Each needs a different response.
Symptom Check: Panic Attack
A panic attack is a sudden wave of intense fear. It often peaks within minutes and then eases.
These anxiety attack symptoms are common:
- Fast heartbeat
- Chest tightness or pain
- Shortness of breath or a feeling like you can't get enough air
- Sweating and trembling
- Dizziness or lightheadedness
- Tingling in hands, feet, or around the mouth
- Chills or hot flashes
- A sense of doom or loss of control
An inhaler doesn't calm panic symptoms. Slow breathing and grounding exercises can be more helpful for easing panic.
Talk with your doctor or a mental health professional if you're having frequent panic attacks, if they're getting worse, or if you're unsure what's causing your symptoms.
Key takeaway: Panic adds body-wide signs and peaks quickly.
Symptom Check: Asthma Attack
An asthma attack happens when your airways narrow and swell.
Common signs:
- Wheeze, cough, and chest tightness
- Trouble breathing and speaking in full sentences
- Feeling like you can't get air out
- Peak flow drops if you use a meter
- Nighttime or early morning symptoms
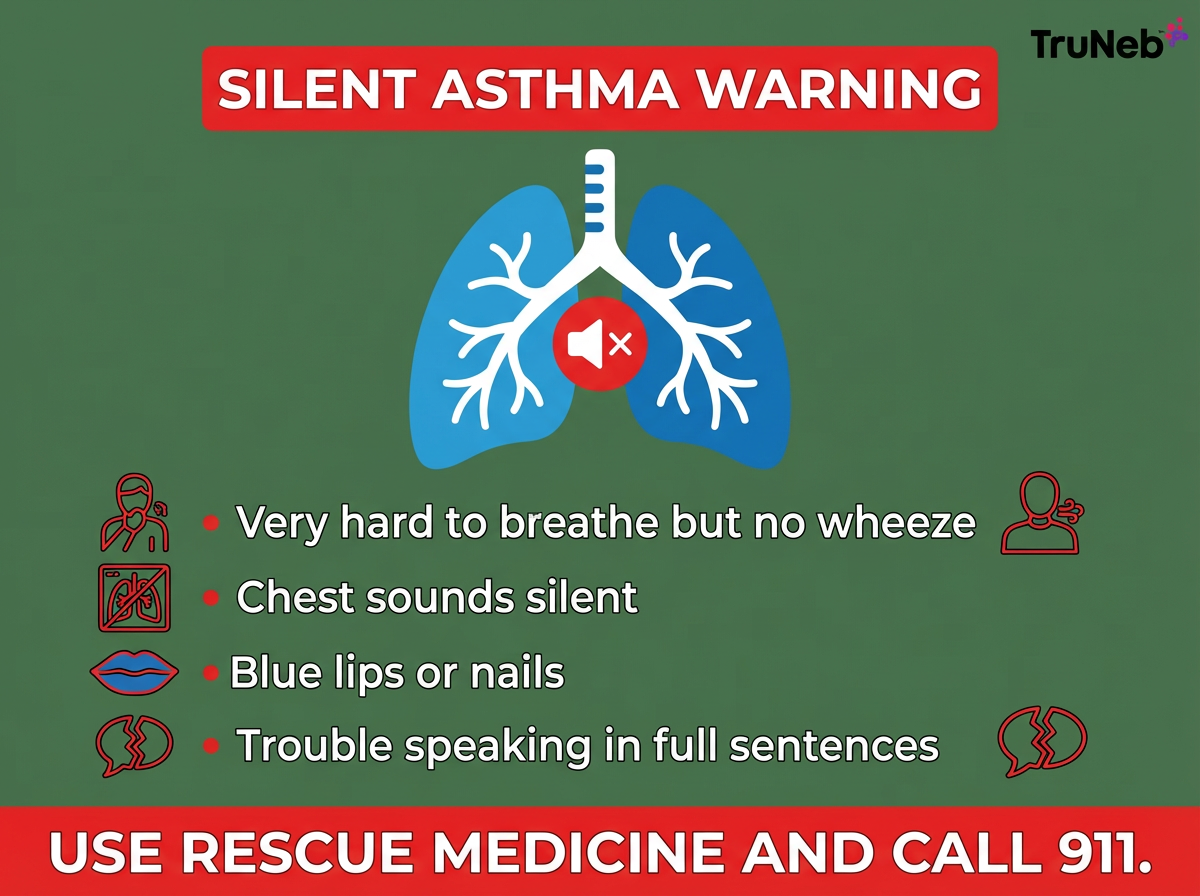
Silent asthma attack symptoms:
- Very hard to breathe but little or no wheeze
- Chest sounds silent when you try to breathe
- Blue lips or nails
A silent chest, blue lips or nails, or severe trouble speaking is an emergency. Follow your emergency asthma plan (which usually includes using your rescue medication) and call 911 right away.
Key takeaway: Wheeze and cough that improve with asthma medicine point to an asthma attack.
What To Do Now if It Feels Like Asthma
Act fast and follow your asthma action plan. Your asthma action plan from your doctor may include steps like:
- Stop and sit upright. Stay as calm as you can.
- Follow the medicine steps in your asthma action plan, such as using your prescribed rescue inhaler with a spacer or your nebulizer. If your doctor has prescribed medicine for a portable mesh nebulizer like TruNeb™ portable mesh nebulizer, use it as directed while you take slow, steady breaths.
- If you have a peak flow meter, check your number and follow your action plan zones.
- If symptoms are severe, if your chest feels silent, or if there's no quick relief after your prescribed steps, call 911.
Medical caution: Talk to your doctor before trying a new medication. Do not change doses on your own.
Key takeaway: Most asthma action plans focus on using your prescribed rescue medicine quickly and getting urgent help if symptoms don't improve.
What To Do Now if It Feels Like Panic
Calm your body so the alarm can fade.
- Breathe in for a gentle 4-second count and out for a longer 6 to 8-second count. Keep shoulders relaxed.
- Try the 5-4-3-2-1 grounding method. Name 5 things you see, 4 you feel, 3 you hear, 2 you smell, 1 you taste.
- Loosen tight clothing and get some cool air.
- Remind yourself that panic feels scary but it passes.
- If you have asthma and are unsure, follow your asthma action plan (which might include taking your rescue medicine) while you begin these calming steps. If it turns out to be panic alone, the inhaler probably won’t change your symptoms much.
If panic attacks keep happening or interfere with daily life, talk with your doctor or a mental health professional about treatment options.
Key takeaway: Panic eases with slow breathing and grounding, not asthma medicine.
When It Is Both: Break the Cycle
Asthma and panic can trigger each other. The feeling of not getting air can spark panic, and panic can tighten breathing even more. Asthma panic attack symptoms can include both wheezing and chest tightness plus a racing heart and shaking.
Break the loop:
- Follow your asthma action plan for treating your airways (usually using your prescribed rescue inhaler or nebulizer).
- At the same time, start slow breathing and grounding.
- If relief isn’t coming, call 911.
Key takeaway: Asthma panic attack treatment often means treating the lungs and calming the nervous system together.
Stay Ready: Triggers, Tools, and an Action Plan
Preparation lowers fear and keeps small problems from becoming crises.
- Know your triggers. Smoke, pollen, cold air, dust, strong smells, and illness are common asthma triggers.
- Keep your rescue inhaler and nebulizer where you can reach them fast. Check expiration dates and batteries.
- A portable nebulizer like TruNeb helps you take your prescribed medication at home, at night, or while traveling.
- If thick mucus is part of your asthma, your doctor might recommend prescription nebulized hypertonic saline (such as 3% or 7%) to help clear airways.
- ⚠️ Don't confuse a nebulizer with a steam inhaler. Steam inhalers use hot mist and aren't meant for breathing in asthma medications.
- Practice your plan. Share it with family or caregivers so they can help.
Medical caution: Talk to your doctor before trying a new medication or adding hypertonic saline. Follow your personalized asthma action plan and only use medications as prescribed by your doctor.
Key takeaway: Preparedness builds confidence because you know your triggers, your steps, and you have the right tools on hand.

Frequently Asked Questions
Key takeaway: These FAQs cover common questions about telling panic attacks from asthma attacks, what doctors look for, and when to seek help.
Tap or click a question below to see the answer:
Yes. Panic can cause fast, shallow breathing that can provoke bronchospasm (tightening of the airway muscles) in people with asthma. During a bad asthma attack, the feeling of not getting air can also trigger panic. Follow the asthma plan you and your doctor have made, which may include using your rescue inhaler or nebulizer, while you start calming techniques.
Silent asthma is severe breathing trouble with little or no wheeze. The chest can sound quiet because very little air is moving. Signs include extreme shortness of breath, trouble speaking, and blue lips or nails. It’s an emergency—follow your emergency asthma plan (usually using your rescue medicine) and call 911 right away.
Not if it’s only panic. A rescue inhaler opens narrowed airways; during a panic attack the airways aren’t the main problem. If you have asthma and aren’t sure, ask your doctor what they recommend for these situations and follow the plan you’ve made together. If it turns out to be panic alone, the inhaler probably won’t change your symptoms much.
They ask about your symptoms and triggers and can test your breathing. Spirometry or peak flow can show if airflow improves after a bronchodilator, which is more consistent with asthma. Doctors also look for panic patterns like sudden fear at rest and body signs such as shaking or tingling. Sometimes both need care at the same time.
Online quizzes can help you notice patterns, but they can’t diagnose. Use them as a prompt to talk with your doctor. If you’re unsure during symptoms, follow your asthma action plan and seek medical care.
Medical caution: Talk to your doctor before trying a new medication. Do not start, stop, or change prescription treatments on your own.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk to your doctor about your symptoms and treatment options, and seek emergency care if you think you’re having a medical emergency.