On this page
Introduction
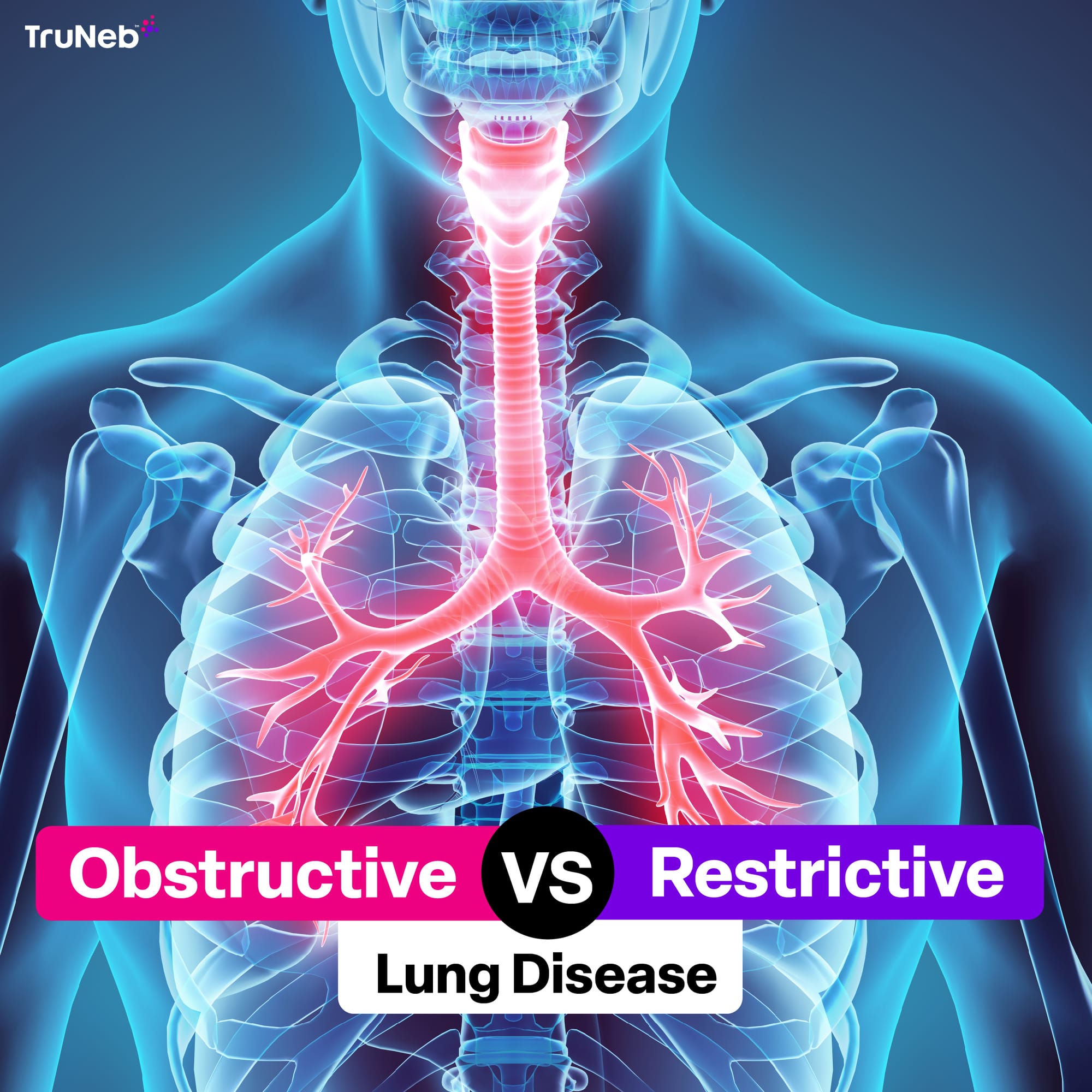
When it comes to breathing, we often take the intricate work of our lungs for granted—until something goes wrong. If you’ve ever found yourself out of breath with no clear reason, you might have wondered what’s happening inside your chest. Obstructive and restrictive lung diseases are two broad categories that explain a lot of respiratory conditions.
But what’s the difference between them, and why does it matter? This article breaks it all down for you. By the end, you’ll have a clear understanding of these conditions, their causes, and treatments.
What Are Obstructive and Restrictive Lung Diseases?
What Is Obstructive Lung Disease?
Imagine trying to exhale through a straw. That’s what living with obstructive lung disease can feel like. These conditions make it hard for your lungs to push air out, leaving too much air trapped inside.
- What’s happening? The airways in your lungs become narrow or blocked, slowing the flow of exhaled air.
- Common causes include:
- COPD: A group of diseases like emphysema and chronic bronchitis.
- Asthma: A condition where inflammation narrows your airways during an attack.
- Bronchiectasis: Permanent widening of the airways, leading to mucus buildup.
- Cystic fibrosis: A genetic condition that causes thick, sticky mucus in the lungs.
What Is Restrictive Lung Disease?
Now, picture trying to blow up a balloon with stiff, unyielding rubber. That’s restrictive lung disease—your lungs just won’t expand fully, no matter how hard you try to inhale.
- What’s happening? Something is limiting how much your lungs can expand, either because of stiffness in the lung tissue or external restrictions.
- Common causes include:
- Pulmonary fibrosis: Scarring in the lungs that makes them less flexible.
- Interstitial lung disease: A group of disorders affecting the tissue between air sacs.
- Neuromuscular conditions: Diseases like ALS that weaken the muscles used for breathing.
- Extrinsic factors: Conditions like scoliosis or obesity that compress the lungs.
How the Lungs Work: A Quick Refresher
Before diving into the differences of obstructive vs restrictive lung disease, let’s take a moment to appreciate the mechanics of good ol’ breathing! Think of your lungs as a pair of sponges sitting in your chest, connected to a series of branching airways.
- The basics of breathing:
- When you inhale, your diaphragm pulls down, creating space for air to flow into your lungs.
- Air travels through the bronchi and smaller airways into alveoli (tiny sacs where oxygen enters your blood).
- Exhaling pushes out carbon dioxide, a waste product of metabolism.
- What happens in lung disease?
- Obstruction: Your airways are like clogged pipes, slowing air outflow.
- Restriction: Your lungs lose their elasticity or get compressed, limiting how much air comes in.
Here’s how these sections could be expanded while maintaining the same approachable and engaging tone as the multifocal pneumonia article you referenced.
Key Differences: Obstructive vs Restrictive Lung Disease
Pathophysiology
Understanding what’s happening under the hood is key to knowing the differences between these two categories.
- Obstructive lung diseases:
- Airflow during exhalation is limited.
- Air gets trapped in the lungs, causing hyperinflation over time.
- Restrictive lung diseases:
- Total lung capacity (TLC) is reduced.
- Lungs can’t fully expand due to stiffness or external pressure.
Causes
The reasons behind these conditions vary widely, but the effects are equally life-altering.
Obstructive causes:
- Smoking (a major culprit for COPD).
- Environmental allergens (asthma triggers like pollen or dust).
- Chronic infections (like those leading to bronchiectasis).
Restrictive causes:
- Autoimmune conditions (e.g., sarcoidosis).
- Chronic scarring (pulmonary fibrosis).
- Physical deformities (e.g., scoliosis).
Symptoms
While both types of lung disease share some overlapping symptoms, subtle differences can clue you in.
Shared symptoms:
- Shortness of breath (especially during exertion).
- Fatigue and reduced exercise tolerance.
- Chronic coughing.
Obstructive-specific:
- Wheezing and noisy breathing.
- Increased mucus production.
Restrictive-specific:
- Difficulty taking deep breaths.
- A feeling of tightness or pressure in the chest.
Diagnostic Differences
Figuring out whether you’re dealing with obstruction or restriction isn’t always straightforward. Doctors rely on a combination of tests to get the full picture.
- Pulmonary function tests (PFTs):
- Obstructive diseases: Reduced FEV1 and FEV1/FVC ratio.
- Restrictive diseases: Reduced FVC and TLC but normal FEV1/FVC ratio.
- Imaging studies:
- X-rays and CT scans can reveal scarring (restrictive) or air trapping (obstructive).
- Bronchoscopy may help uncover structural or infectious causes.
Common Conditions Under Each Category
Obstructive Lung Diseases
Obstructive lung diseases make it feel like you’re trying to exhale through a straw. The air gets trapped, and it’s tough to get it all out. Here are some of the main culprits:
- Chronic Obstructive Pulmonary Disease (COPD): Think of COPD as the umbrella term for two major troublemakers—emphysema and chronic bronchitis. It’s often caused by smoking or exposure to pollutants and can leave you wheezing, coughing, and short of breath.
- Asthma: Asthma flares up when the airways get inflamed, making it hard to breathe. Triggers can range from allergens to exercise, and while it can come and go, managing it often involves inhalers and careful planning.
- Bronchiectasis: This one’s all about permanently widened airways. It leads to mucus buildup, recurrent infections, and a persistent cough that just won’t quit.
- Cystic Fibrosis: A genetic condition that creates thick, sticky mucus clogging up the lungs. It’s a lifelong challenge but one that can be managed with the right treatments.
Restrictive Lung Diseases
Restrictive lung diseases are the opposite—your lungs feel like they’re in a straightjacket, unable to fully expand. Here are the key players:
- Pulmonary Fibrosis: This condition causes scarring in the lungs, making them stiff and less able to do their job. Over time, this leads to progressive shortness of breath and a dry, nagging cough.
- Interstitial Lung Disease (ILD): A group of conditions that inflame and scar the tissues surrounding the air sacs. It’s like your lungs’ “support system” is working against them.
- Neuromuscular Diseases: Conditions like ALS or muscular dystrophy weaken the muscles needed for breathing, limiting how much air your lungs can take in.
- Extrinsic Causes: External factors like severe scoliosis or obesity put physical limits on your lungs, compressing them and making every breath feel like a struggle.
Diagnosing Obstructive vs. Restrictive Lung Diseases
Pulmonary Function Tests
Doctors often start with pulmonary function tests (PFTs) to figure out what’s going on in your lungs. These tests are like a fitness tracker for your respiratory system:
- FEV1 (Forced Expiratory Volume in one second): This measures how much air you can blow out in the first second. If it’s low, it might mean obstructive disease.
- FVC (Forced Vital Capacity): This is the total air you can exhale after a deep breath. It’s usually reduced in restrictive diseases.
- FEV1/FVC Ratio: The magic ratio! If it’s lower than normal, it points to obstruction. A normal or higher ratio suggests restriction.
- Total Lung Capacity (TLC): Think of this as your lungs’ storage space. It’s often higher in obstructive diseases (due to trapped air) but lower in restrictive conditions.
Imaging Studies
When PFTs raise questions, imaging steps in to give doctors a visual roadmap of your lungs:
- Chest X-rays: These can reveal signs of air trapping (obstruction) or scarring and reduced lung volume (restriction).
- CT Scans: A more detailed look to pinpoint structural changes, whether it’s emphysema, fibrosis, or something else.
- Bronchoscopy: When more answers are needed, this procedure uses a small camera to explore the airways and even collect tissue samples.
Lab Tests
Lab tests add another layer of insight into how your lungs are functioning:
- Blood Oxygen Levels: A simple pulse oximeter can measure oxygen saturation, while arterial blood gas tests dig deeper to assess oxygen and carbon dioxide levels.
- DLCO (Diffusion Capacity of the Lung for Carbon Monoxide): This test checks how well oxygen moves from your lungs into your bloodstream. It’s often reduced in both restrictive and obstructive conditions, but for different reasons.
Treatment Options for Obstructive and Restrictive Lung Diseases
Treatments for Obstructive Lung Disease
The goal here is to open up the airways, reduce inflammation, and help you breathe easier. Treatments often include:
- Bronchodilators: These are your quick-relief go-to’s. Medications like Albuterol or Salmeterol relax airway muscles, making it easier to exhale.
- Corticosteroids: Inhaled or oral steroids tackle inflammation, helping to reduce swelling and mucus production.
- Pulmonary Rehabilitation: This combines exercise, breathing techniques, and education to improve lung function and overall quality of life.
- Oxygen Therapy: For those with advanced disease, supplemental oxygen helps keep blood oxygen levels stable.
- Lung Transplant: In extreme cases, a transplant may be the best option to regain quality of life.
Treatments for Restrictive Lung Disease
For restrictive diseases, it’s all about addressing the root cause and improving lung capacity where possible:
- Antifibrotic Medications: Drugs like Esbriet and Ofev can slow the progression of pulmonary fibrosis, preserving lung function.
- Immunosuppressants: Medications such as corticosteroids or methotrexate help manage autoimmune-related lung scarring or inflammation.
- Weight Loss and Exercise: For obesity-related cases, even small weight reductions can make a big difference in breathing.
- Mechanical Ventilation: Non-invasive options like BiPAP provide breathing support for those with weakened respiratory muscles.
- Lung Transplant: For severe cases, a transplant can be life-changing, offering a fresh start for damaged lungs.
Treatment Options for Obstructive and Restrictive Lung Diseases
Treatments for Obstructive Lung Disease
The goal here is to open up the airways, reduce inflammation, and help you breathe easier. Treatments often include:
- Bronchodilators: These are your quick-relief go-to’s. Medications like Albuterol or Salmeterol relax airway muscles, making it easier to exhale.
- Corticosteroids: Inhaled or oral steroids tackle inflammation, helping to reduce swelling and mucus production.
- Pulmonary Rehabilitation: This combines exercise, breathing techniques, and education to improve lung function and overall quality of life.
- Oxygen Therapy: For those with advanced disease, supplemental oxygen helps keep blood oxygen levels stable.
- Lung Transplant: In extreme cases, a transplant may be the best option to regain quality of life.
Treatments for Restrictive Lung Disease
For restrictive diseases, it’s all about addressing the root cause and improving lung capacity where possible:
- Antifibrotic Medications: Drugs like Esbriet and Ofev can slow the progression of pulmonary fibrosis, preserving lung function.
- Immunosuppressants: Medications such as corticosteroids or methotrexate help manage autoimmune-related lung scarring or inflammation.
- Weight Loss and Exercise: For obesity-related cases, even small weight reductions can make a big difference in breathing.
- Mechanical Ventilation: Non-invasive options like BiPAP provide breathing support for those with weakened respiratory muscles.
- Lung Transplant: For severe cases, a transplant can be life-changing, offering a fresh start for damaged lungs.
Restrictive vs Obstructive Lung Diseases
| Category | Restrictive Lung Diseases | Obstructive Lung Diseases |
|---|---|---|
| Definition | Difficulty expanding lungs due to reduced lung compliance or chest wall restrictions. | Difficulty exhaling air due to narrowed or obstructed airways. |
| Common Causes |
- Pulmonary fibrosis - Interstitial lung disease (ILD) - Neuromuscular diseases (e.g., ALS, muscular dystrophy) - Obesity - Scoliosis |
- Chronic obstructive pulmonary disease (COPD) - Asthma - Bronchiectasis - Cystic fibrosis |
| Symptoms |
- Shortness of breath, especially during inhalation - Difficulty taking deep breaths - Chest tightness - Fatigue - Cyanosis in severe cases |
- Wheezing - Chronic cough with mucus - Shortness of breath, especially during exhalation - Chest tightness - Frequent respiratory infections |
| Pulmonary Function Test Results |
- Decreased total lung capacity (TLC) - Normal or increased FEV1/FVC ratio |
- Decreased FEV1/FVC ratio - Increased residual volume (RV) |
| Imaging Features |
- Fibrotic changes in lungs (seen on X-rays or CT scans) - Honeycombing or ground-glass opacities |
- Hyperinflation of lungs - Air trapping and thickened airway walls |
| Treatment Approaches |
- Antifibrotic drugs (e.g., pirfenidone, nintedanib) - Immunosuppressants (e.g., corticosteroids) - Oxygen therapy - BiPAP/CPAP for neuromuscular causes - Weight loss for obesity-related cases |
- Bronchodilators (e.g., albuterol) - Inhaled corticosteroids - Oxygen therapy - Pulmonary rehabilitation - Lifestyle changes like smoking cessation |
| Severity and Prognosis | Progressive and variable, depending on the cause; severe cases may require lung transplants. | Progressive but manageable with proper treatment; early diagnosis improves outcomes. |
Preventing Obstructive and Restrictive Lung Diseases
Prevention is always better than cure. While some causes of lung disease, like genetics, can’t be avoided, there are steps you can take to reduce your risk.
Preventing Obstructive Lung Diseases
Most obstructive lung diseases are linked to environmental factors and lifestyle choices. Here’s how to reduce your risk:
- Quit Smoking: Smoking is the number one cause of COPD and worsens asthma symptoms. Quitting not only protects your lungs but also improves your overall health.
- Avoid Pollutants: Limit exposure to air pollution, dust, and workplace irritants. Use masks or protective gear in environments with harmful particles.
- Manage Asthma Triggers: Keep your home clean, avoid allergens, and carry a rescue inhaler to manage asthma attacks.
- Stay Active: Regular exercise strengthens your respiratory muscles and improves lung capacity.
Preventing Restrictive Lung Diseases
Restrictive lung diseases are harder to prevent because they often result from chronic conditions or external factors. However, these tips can help:
- Vaccinate: Get flu and pneumonia vaccines to reduce the risk of infections that can cause scarring or damage.
- Maintain a Healthy Weight: Obesity can compress the lungs, so adopting a balanced diet and regular exercise routine is essential.
- Treat Underlying Conditions: Properly manage autoimmune diseases, scoliosis, or other health issues to prevent complications.
- Practice Good Posture: For those with scoliosis or other structural conditions, posture correction and physiotherapy can support lung function.
Living with Obstructive and Restrictive Lung Diseases
Daily Life and Management
Living with a chronic lung condition doesn’t mean you can’t lead a fulfilling life. Here are some ways to manage symptoms and stay proactive:
- Follow Your Treatment Plan: Stick to your prescribed medications and therapies, whether it’s using inhalers or taking antifibrotic drugs.
- Adopt Healthy Habits: Quit smoking, eat a balanced diet, and exercise regularly. Even light activities like walking can improve lung function.
- Monitor Symptoms: Keep an eye on changes like increased shortness of breath or persistent cough, and report them to your doctor promptly.
- Join Support Groups: Connecting with others who understand your journey can provide emotional support and practical tips.
Tools and Technologies to Help
Advances in medical technology make it easier to manage lung conditions:
- Portable Nebulizers: Devices like the TruNeb™ Portable Nebulizer deliver medication directly to your lungs, making breathing treatments more accessible and convenient.
- Home Oxygen Therapy: For those with severe conditions, oxygen tanks or concentrators can improve quality of life.
- Smart Apps and Trackers: Apps can remind you to take your medication, track symptoms, and even alert your doctor if your condition worsens.
The Importance of Early Diagnosis
Both obstructive and restrictive lung diseases can progress over time, so catching them early is crucial. Regular check-ups, especially if you have risk factors like smoking or a family history of lung disease, can make a huge difference.
- Don’t Ignore Symptoms: Shortness of breath, chronic cough, or wheezing shouldn’t be dismissed as “just getting older.” They could signal an underlying issue.
- Be Proactive: Ask your doctor for pulmonary function tests or imaging if you’re experiencing persistent respiratory problems.
Final Thoughts
Understanding the differences between obstructive vs restrictive lung disease empowers you to take control of your health. While these conditions can sound intimidating, proper diagnosis, treatment, and lifestyle adjustments can make a world of difference.
Remember, whether it’s managing symptoms with tools like nebulizers or taking steps to prevent lung disease altogether, every action counts. Your lungs work hard for you—give them the care they deserve. And if you or a loved one is dealing with a lung condition, don’t hesitate to reach out to a healthcare provider for support.
*Article reviewed by a licensed Registered Respiratory Therapist