On this page

Healthy Lungs vs COPD Lungs: Key Differences at a Glance
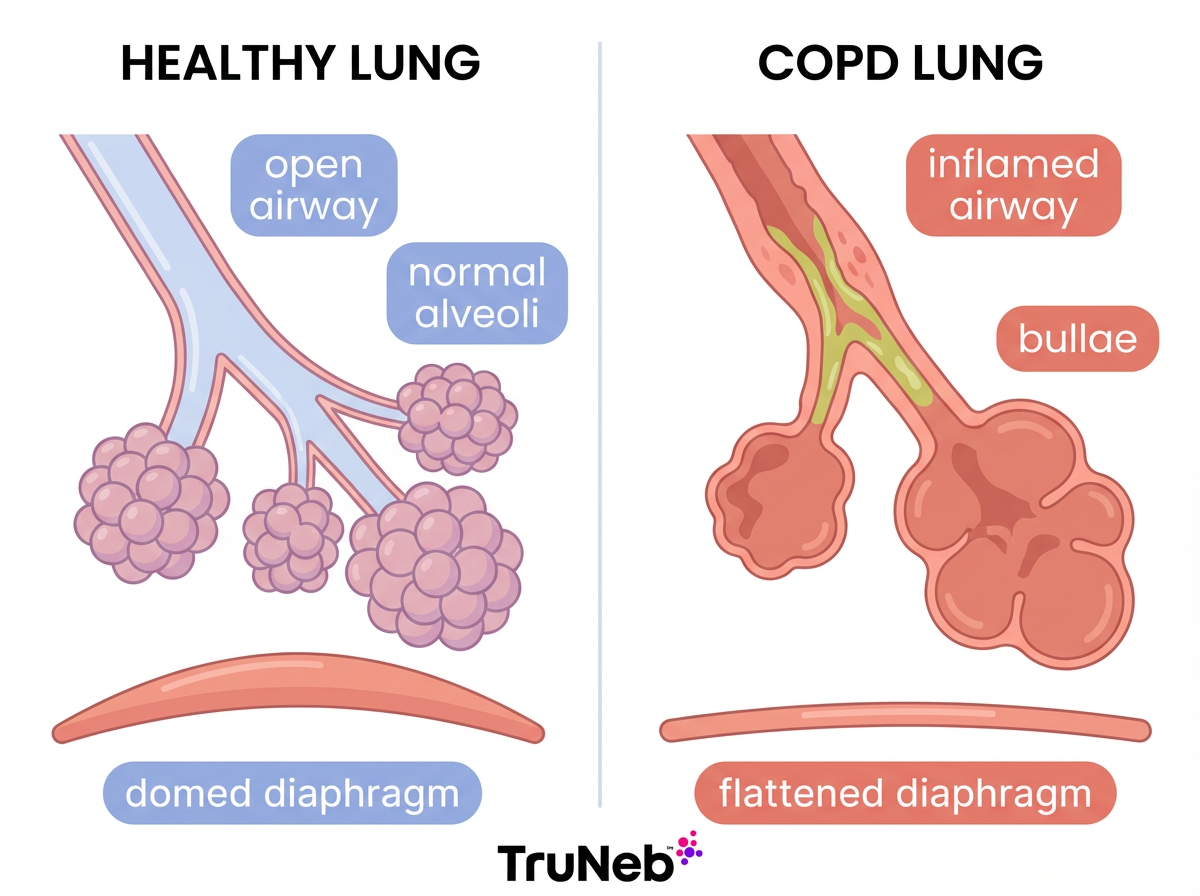
Healthy lungs are elastic and clear. Air moves in and out easily, and oxygen passes into your blood without trouble.
COPD (Chronic Obstructive Pulmonary Disease) is a long-term lung disease that includes emphysema and chronic bronchitis, and it causes chronic airflow limitation. This section explains the difference between healthy lungs and COPD lungs so you can see what changes over time.
In COPD, ongoing damage affects both the airways and the tiny air sacs. Airways get inflamed and thicker. The air sacs (alveoli) lose their spring and can break into bigger, floppy spaces. It becomes hard to breathe out, so old air gets trapped. Over years, lungs can look larger on scans and the diaphragm can look flatter. The damage doesn’t fully reverse and tends to progress without care.
In short: healthy lungs are elastic and clear; COPD lungs are inflamed, less elastic, and usually hyperinflated with trapped air.
Normal Lung Structure and Function
Your lungs branch like a tree. Air moves from the windpipe to the bronchi, then into smaller bronchioles, and finally into millions of tiny air sacs called alveoli.
In healthy lungs:
- Airways are open and smooth, with little mucus.
- Cilia (tiny hairs) sweep out dust and germs.
- Alveoli are springy, like new balloons. Their elastic recoil helps them fill and empty with each breath.
- Oxygen crosses thin alveoli walls into the blood, and carbon dioxide leaves when you exhale. This swap is called gas exchange.
- The diaphragm sits like a soft dome under your lungs. It drops down to pull air in and rises to push air out.
In short: healthy lungs have clear airways, springy alveoli, and a strong diaphragm that makes breathing easy.
How COPD Changes the Lungs: Structure and Mechanics
Here’s how COPD damages the lungs over time:
Alveoli damage and loss of elasticity
- In emphysema, the thin walls between alveoli break down. Numerous small air sacs merge into larger air spaces called bullae.
- These big spaces hold air but don’t exchange oxygen well. Less surface area for gas exchange means less oxygen gets to your blood, especially with activity.
- The lungs lose their natural spring. Air doesn’t leave easily, so it gets trapped (hyperinflation).
Airway inflammation, thickening, and mucus
- In chronic bronchitis, the airway lining stays swollen and irritated.
- The walls can thicken, and the glands make extra mucus. Mucus clogs tubes and slows airflow.
- Airway muscles can tighten (bronchospasm), making breathing even harder during flare-ups.
Air trapping and breathing muscles
- Narrowed airways can collapse early when you breathe out. Air gets stuck inside (air trapping).
- Trapped air pushes the diaphragm down over time. Instead of a dome, it looks flat on scans and works less effectively.
- The chest can look rounder from front to back (sometimes called a barrel chest in advanced disease). Breathing takes more effort and can feel like blowing through a narrow straw.
In short: COPD destroys alveoli, thickens and clogs airways, and traps air, which flattens the diaphragm and makes each breath harder.
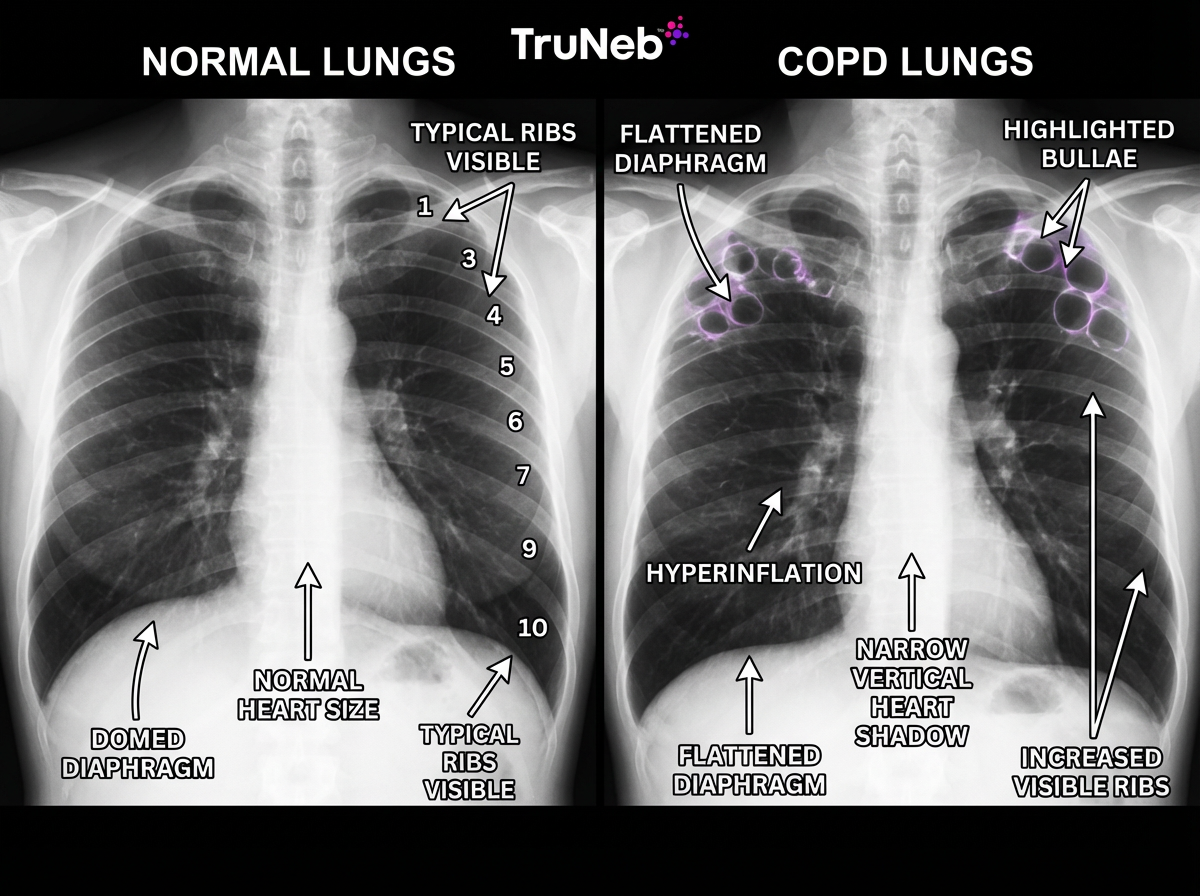
What COPD Looks Like on X-ray and CT Scan
On scans, COPD lungs usually look larger and darker with a flattened diaphragm, while normal lungs look compact with a domed diaphragm and fine vessel markings.
Chest X-ray signs:
- Hyperinflated lungs: more black space than normal because extra air is trapped. More ribs are visible above the diaphragm than normal.
- Flattened diaphragm: instead of a smooth dome, it sits lower and looks flatter.
- Bullae: round, darker areas that look like holes where lung tissue is destroyed.
- Fewer fine lung markings in damaged areas: parts can look unusually clear.
- Long, narrow heart shadow in emphysema: sometimes called a floating heart appearance from overinflated lungs.
CT scan can show:
- Small bullae and early emphysema that an X-ray can miss.
- Thickened airway walls and patterns of emphysema.
- How much lung is affected, and sometimes enlarged pulmonary arteries.
Compared with a normal CT, COPD shows bullae and airway wall thickening; a normal lung CT looks uniform without large air pockets.
Imaging is also used to rule out other conditions such as pneumonia, heart failure, or lung cancer.
Note: mild COPD can look normal on a plain X-ray; spirometry typically finds airflow problems earlier.
Bottom line: scans of COPD usually show bigger, darker lungs with a flat diaphragm and bullae, while early disease can still look normal on X-ray.
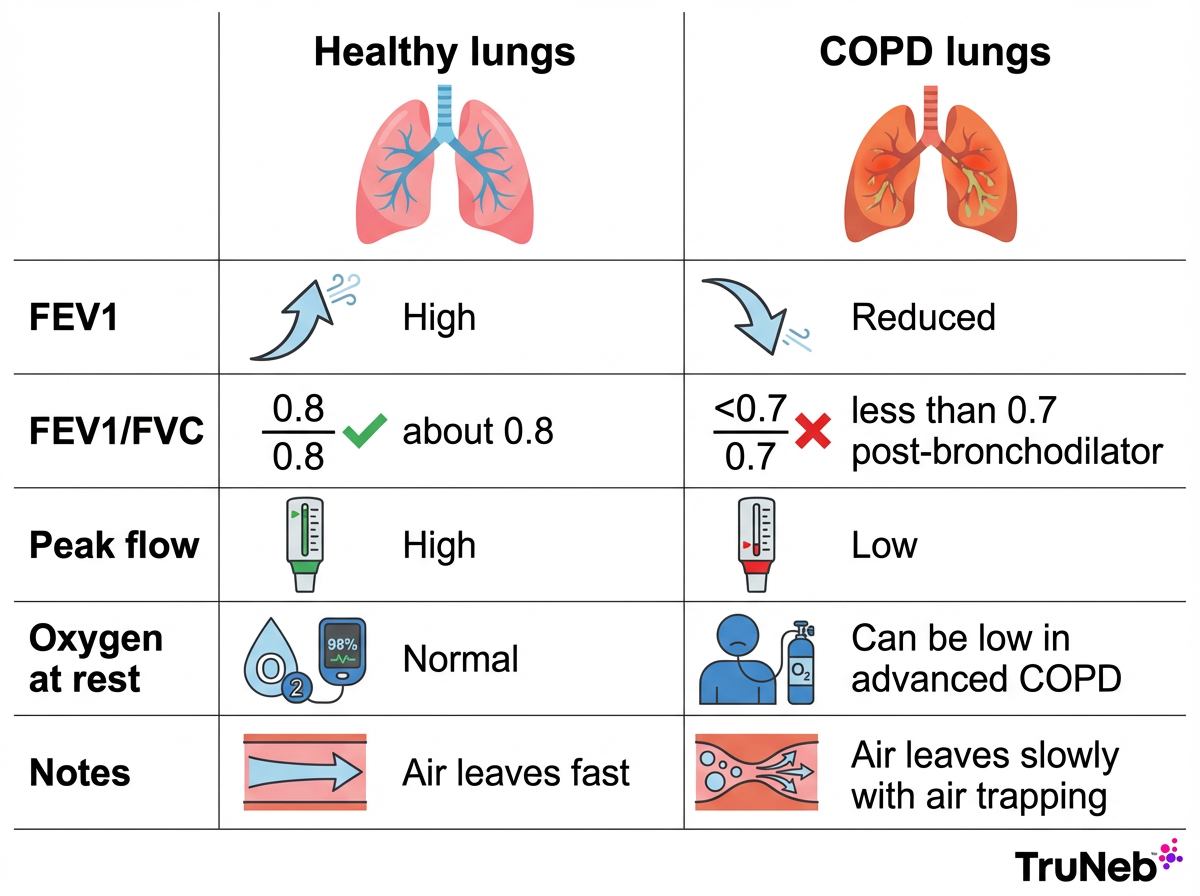
Normal vs COPD Lung Function and Breathing Tests
Spirometry shows slower, reduced airflow in COPD compared with normal lungs.
Spirometry is the main test. You take a deep breath and blow out as hard and fast as you can. If your doctor suggests spirometry, the test is quick and painless.
What’s normal:
- You blow out most of your air in the first second (FEV1).
- The FEV1/FVC ratio is usually around 0.8 (80%).
What COPD shows:
- FEV1 is reduced.
- The FEV1/FVC ratio is below 0.7 after using a bronchodilator, showing airflow obstruction.
- Peak flow is lower because air leaves more slowly.
- Lung volumes such as residual volume are increased, and total lung capacity can be higher due to trapped air.
Oxygen and exercise:
- Early COPD can have normal oxygen at rest but drops with activity.
- Advanced COPD can cause low oxygen and high carbon dioxide, sometimes checked with an arterial blood gas test. Your oxygen saturation, measured with a pulse oximeter, helps track this at home or in the clinic.
That’s why climbing stairs can feel like sprinting against a headwind.
Put simply: spirometry finds COPD by showing a low FEV1/FVC ratio and slower airflow, usually before changes appear on X-ray.
From Healthy to COPD: Causes and Progression
Most COPD develops over years.
Main causes:
- Smoking is the top cause. The longer and more you smoke, the higher the risk.
- Long-term exposure to dust, fumes, or heavy air pollution can also damage lungs.
- A rare genetic condition called alpha-1 antitrypsin deficiency can lead to early emphysema, even in non-smokers.
Progression and early changes:
- Damage builds slowly. Early COPD can be silent on X-ray and doesn’t always cause much shortness of breath at rest.
- Research has found that some smokers with normal lung tests still have COPD-like symptoms and subtle changes that standard tests can miss.
Irreversibility:
- COPD damage to alveoli and airways is permanent. You can’t regrow destroyed lung tissue.
- The good news: quitting smoking and the right care can slow decline and help you feel and function better.
In summary: COPD damage is permanent, but early care and quitting smoking can slow decline and improve daily breathing.
Managing and Supporting COPD Lungs
While COPD damage can’t be reversed, you can support your lungs and feel better.
Medicines that open airways:
- Bronchodilators relax airway muscles to improve airflow. Inhaled corticosteroids can reduce airway inflammation when prescribed.
- These can be taken by inhaler or by nebulizer. A portable mesh nebulizer like the TruNeb™ device turns liquid medicine into a fine mist that’s convenient to use at home or on the go.
⚠️ Steam inhalers are not the same as nebulizers and shouldn’t be used to deliver COPD medications.
Clearing mucus:
- If mucus is a daily problem, airway clearance helps. Controlled coughing, chest physiotherapy, and postural drainage can move mucus.
- Some people use nebulized hypertonic saline to thin and move mucus under your doctor’s guidance. Not everyone needs this; it’s for specific mucus problems.
Rehab, oxygen, and protection:
- Pulmonary rehabilitation helps you build stamina and learn breathing skills like pursed-lip breathing (breathing out slowly through pursed lips, like you’re whistling, to keep airways from collapsing).
- If oxygen runs low, your doctor can prescribe supplemental oxygen.
- Protect what you have: stop smoking, avoid lung irritants, and keep up with flu and pneumonia vaccines.
⚠️ If you have severe shortness of breath at rest, chest pain, blue lips or face, or confusion, seek emergency medical care right away. Talk to your doctor if your breathlessness suddenly worsens, your cough changes, or your usual treatments stop working as well.
Safety note: Talk to your doctor before trying a new medication or saline treatment. Never start, stop, or change prescription therapy on your own. Use only medicines prescribed for you and equipment meant for breathing treatments, not humidifiers or steam devices.
In short: treatment can open airways, clear mucus, and build stamina so COPD lungs work as well as they can.
Frequently Asked Questions
Here are quick answers to common questions about how COPD lungs compare to healthy lungs and how doctors diagnose the condition. Tap or click a question below to see the answer:
No. Mild COPD can look normal on a chest X-ray. Doctors rely on spirometry to detect early airflow blockage. CT scans can show early lung damage and airway changes that X-rays miss. X-rays also help rule out other causes of symptoms, such as pneumonia or heart failure.
No. Damage to alveoli and airway walls is permanent. Treatment and healthy habits can still slow decline and help you breathe and move better.
With spirometry. A low FEV1/FVC ratio after a bronchodilator confirms airflow obstruction. Imaging helps show the extent of damage and rule out other problems.
Yes. Long-term exposure to dust, fumes, or heavy air pollution can cause COPD. A rare condition called alpha-1 antitrypsin deficiency can also lead to emphysema.
Emphysema is one type of COPD. Chronic bronchitis is the other main type. A lot of people have features of both.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms and before making any changes to your medications or treatment plan.