On this page

Babies mostly breathe through their noses, so congestion can make feeding and sleep hard. Most mild colds do not need a nebulizer; comfort care like saline nose drops and a cool mist humidifier usually helps. Sometimes, under your doctor’s guidance, a nebulizer for baby congestion can help, especially with wheezing or very thick mucus. This guide explains when a nebulizer can help baby congestion, how it works, and how to use it safely with your pediatrician’s plan.
When Is a Nebulizer Needed for Baby Congestion
Use a nebulizer only when a pediatrician says it can help with a specific problem:
- Bronchiolitis (a lower lung infection that is usually caused by RSV) with wheezing or heavy chest congestion. Some doctors use saline nebulization in moderate cases to thin mucus, generally under medical supervision in a clinic or hospital. Routine bronchodilators are not recommended for typical bronchiolitis.
- Wheezing or reactive airway episodes. A doctor can prescribe nebulized albuterol to open tight airways.
- Croup with stridor (a high-pitched noise when your baby breathes in). Nebulized epinephrine is an emergency treatment given in a clinic or ER, not at home.
Conditions like pneumonia usually require hospital care; a home nebulizer is not the primary treatment.
Not needed: a runny or mildly stuffy nose without breathing trouble. Comfort care usually works better.
A portable mesh device like the TruNeb™ portable mesh nebulizer can fit into the plan when your doctor recommends inhaled saline or medicine.
Bottom line: Use a nebulizer for wheeze or very thick mucus under doctor guidance, not for an ordinary runny nose.
How a Nebulizer Relieves a Baby’s Congestion
A nebulizer turns liquid into a fine mist your baby can breathe.
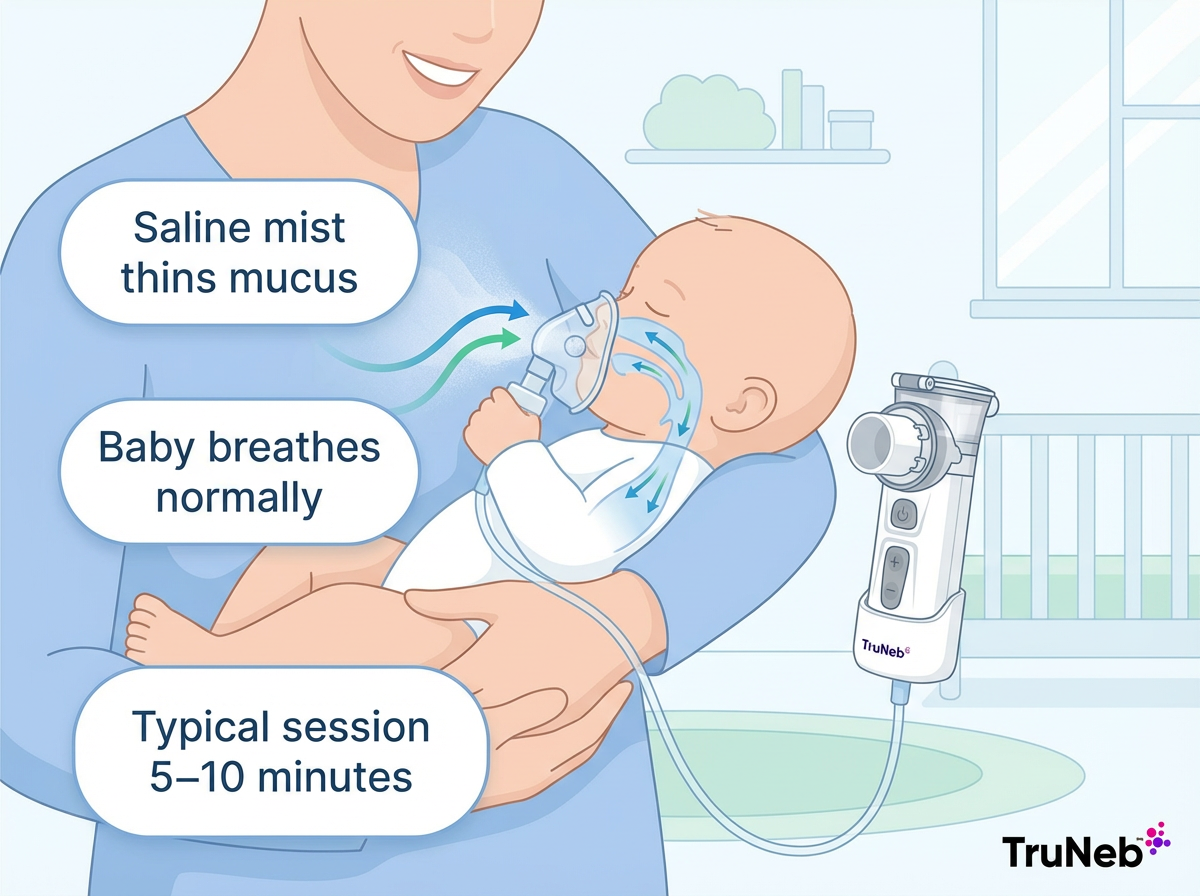
For congestion, sterile saline mist adds moisture to the airways and thins thick mucus. That makes it easier for your baby to clear mucus by coughing, sneezing, or swallowing.
Nebulized saline mainly helps loosen mucus in the nose, throat, and small airways, so both a stuffy nose and chest congestion can feel easier.
Babies do not have to time their breaths. With a mask on, they simply breathe normally while the mist does the work.
Types:
- Compressor (jet) nebulizers plug into the wall and use an air pump.
- Mesh nebulizers use a vibrating mesh to make an ultra-fine, quiet mist in a small handheld unit.
Quick note: A nebulizer sends mist directly into your baby’s airways. A humidifier adds moisture to the room air for general comfort.
Consumer warning: If you see products labeled "steam inhaler," remember they are not the same as nebulizers and are not meant for breathing medicines, especially not for babies.
Bottom line: Nebulizer mist thins mucus and reaches tiny airways while your baby breathes normally.
Is It Safe to Use a Nebulizer on a Baby?
Yes. Nebulizers are generally considered safe for babies when used the right way and under medical guidance.
Do this:
- Use only sterile saline or the exact medication and dose your pediatrician prescribed
- Use an infant-sized mask and keep your baby upright and calm during the session
- Stay with your baby for the entire treatment
Do not do this:
- Do not put essential oils, OTC cough and cold products, or homemade mixtures in a nebulizer
- Do not increase dose or frequency on your own
Over-the-counter cough and cold medicines are not recommended for children under 2, and they should never be nebulized.
Normal reactions: Saline can trigger a brief cough or sneeze as mucus loosens. Medications like albuterol can sometimes cause mild jitteriness. Call your doctor if anything seems severe. If your baby seems more short of breath, very fussy, or unusually quiet during a treatment, stop the session and call your doctor.
Safety note: Talk to your doctor before trying a new medication.
Bottom line: Nebulizers are generally safe for babies when you use the right solution, the right mask, and follow your doctor’s plan.
What Solution Should You Use in a Baby’s Nebulizer?
For baby congestion, doctors usually start with plain sterile saline in the nebulizer.
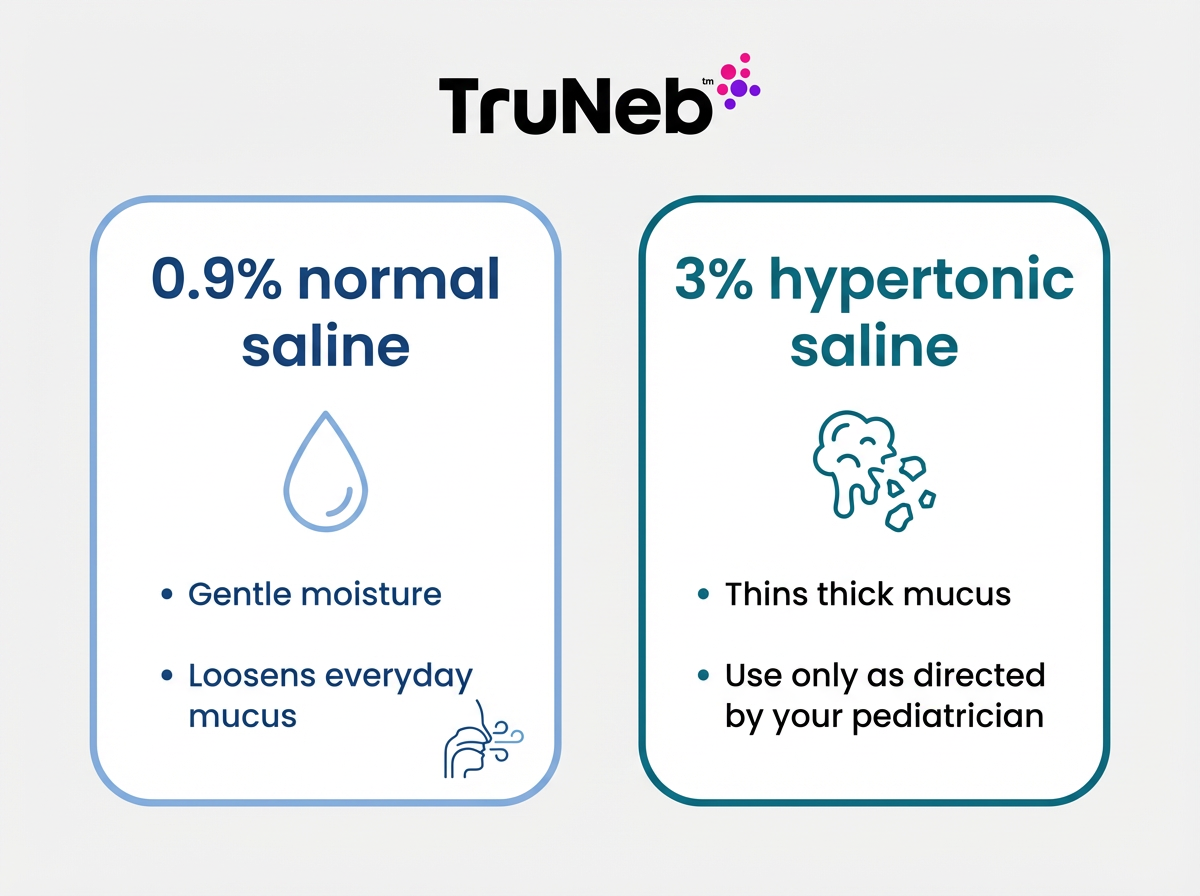
Options:
- 0.9% normal saline: Gentle moisture that helps loosen mucus.
- 3% hypertonic saline: Stronger salt solution that draws water into the airways and thins thick mucus. Pediatricians sometimes recommend this for bronchiolitis or very sticky mucus, usually for short-term use under close guidance.
- 7% hypertonic saline: A higher concentration used in older children under specialist care; it’s not routine for babies.
Medications:
- Bronchodilators like albuterol are used for wheezing or reactive airways if your doctor prescribes them.
- Epinephrine for severe croup is given in a clinic or ER, not at home.
Important:
- Use only sterile, neb-ready solutions in single-use vials.
- Do not nebulize decongestant drops, essential oils, or homemade salt water.
TruNeb™ also sells ready-to-use 3% hypertonic saline vials made for nebulizers. Use hypertonic saline only if your baby’s doctor recommends it.
Bottom line: For congestion, saline is usually enough; medicines are for specific diagnoses.
What Makes a Nebulizer Baby-Friendly?
Look for features that keep treatments short, quiet, and easy:
- Ultra-quiet operation so you can treat without startles or stress
- Fast treatments around 5–10 minutes
- Portable and rechargeable so you can move from nursery to car seat without hunting for an outlet
- Infant mask compatibility to get a good seal on tiny faces
- Simple setup and easy cleaning so you can focus on your baby, not parts
A quiet handheld nebulizer means you can treat a congested baby at night without a loud motor waking everyone.
Why TruNeb fits: TruNeb is a handheld mesh nebulizer that is quiet, compact, USB rechargeable, and designed for simple, fast treatments. It’s easy to pack and easy to use during naps or travel.
Bottom line: A quiet, quick, cordless nebulizer makes treatments easier on both babies and parents.
How to Give a Nebulizer Treatment to a Congested Baby
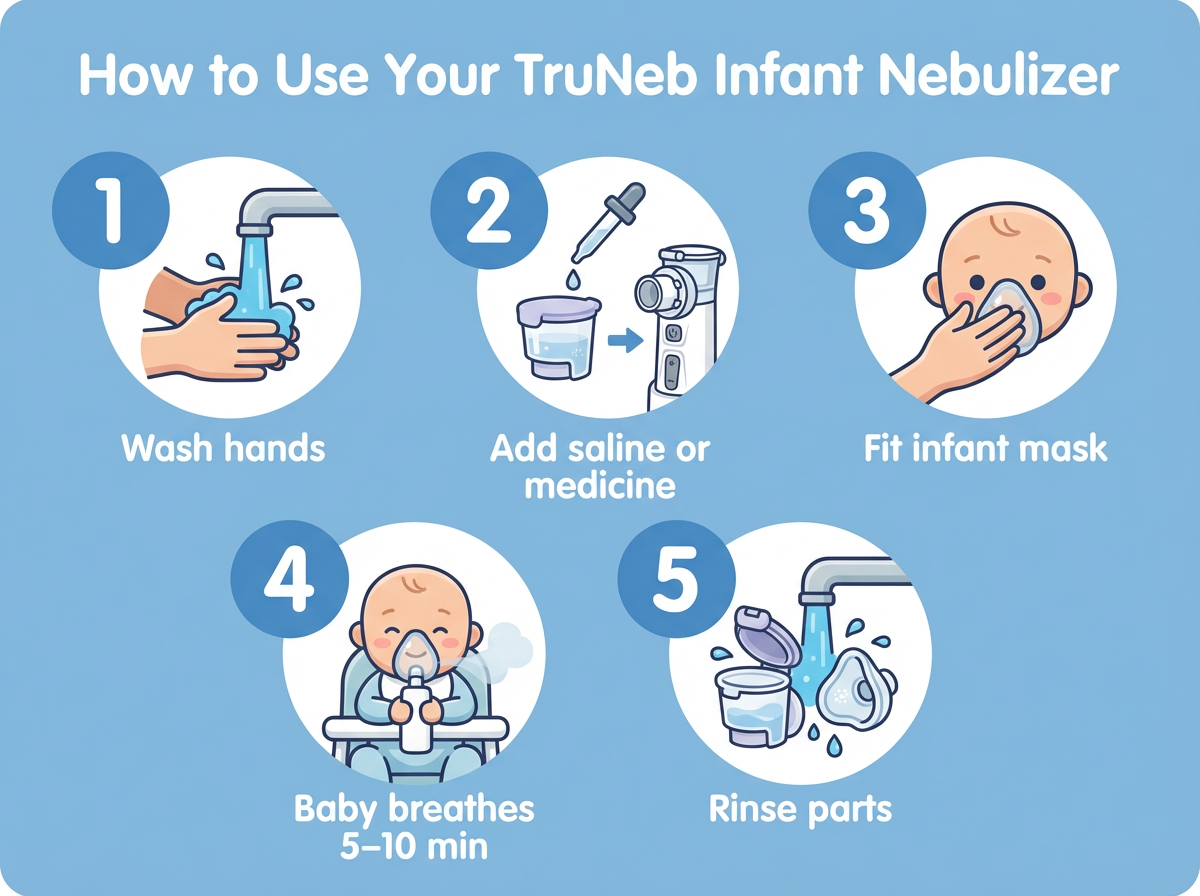
Here’s how to use a nebulizer for baby congestion. These are general steps to show what a baby session usually looks like—always follow your doctor’s instructions and your device manual.
- Wash your hands and set up. Gather the device, the medicine cup, and the infant mask. Add the exact saline or medication your doctor prescribed, as directed by your doctor or the device instructions. If you use a portable device like TruNeb, make sure it’s charged.
- Fit the infant mask. It should gently cover the nose and mouth without big gaps.
- Hold your baby upright. Keep them calm with a song, a story, or a favorite toy. Crying hard reduces how much mist reaches the lungs.
- Start the nebulizer. You should see a light mist. Hold the mask in place and let your baby breathe normally.
- Finish the dose. Continue until the mist slows or the cup is empty, usually about 5–10 minutes, or as directed by your doctor.
- Clean the parts you used. Rinse the mask and cup now so they’re ready for next time (see the cleaning section below for full hygiene steps).
Bottom line: Upright, calm, steady breathing for 5–10 minutes gets the most from each treatment.
How to Clean a Nebulizer After Use
A quick cleaning routine keeps each treatment safer for your baby’s lungs. Dirty nebulizer parts can grow germs that go straight into your baby’s airways, so cleaning really matters.
After each use:
- Detach the mask and medicine cup
- Rinse them with warm water and let them air-dry on a clean towel
Regularly:
- Wash with mild dish soap and warm water. Rinse well and air-dry completely.
- Disinfect weekly if you use it frequently. Some families use a 1:3 vinegar and hot water soak for 30 minutes, then rinse and dry. Check your device manual for the method approved for your model; some mesh nebulizers have specific instructions and do not recommend vinegar soaks.
Never submerge the electronic body of a mesh nebulizer. Store all parts dry in a clean pouch.
Bottom line: Rinse after every use and disinfect on a schedule to prevent germs.
Know the Red Flags and When to Seek Emergency Care
Call 911 or go to emergency care right away if you see:
- Blue or gray color around the lips, face, or tongue
- Skin pulling in between ribs or at the neck with each breath (retractions)
- Strong nostril flaring
- Very fast breathing or pauses in breathing
- Limpness, extreme sleepiness, or trouble waking
- Signs of dehydration, such as very few wet diapers
If you’re outside the U.S., call your local emergency number instead of 911.
Call your pediatrician soon if treatments are not helping, symptoms are getting worse, you feel you need treatments more often than prescribed, or if you’re unsure whether to keep doing treatments at home.
Bottom line: Blue lips, retractions, or very fast breathing are emergency signs.
Why TruNeb™ Is a Good Fit for Baby Congestion
A baby-friendly nebulizer should be quiet, quick, and easy to take anywhere. TruNeb was designed for busy families who want treatments to fit into everyday life.
TruNeb™ is a portable nebulizer for baby congestion that’s quiet and easy to take anywhere. It’s a portable mesh nebulizer for babies and young children that fits in a diaper bag and sets up fast, so you can stick with your doctor’s plan at home or on the go.
- Nighttime: the quiet mesh mist helps you treat without waking everyone
- On the go: handheld, USB‑rechargeable design fits in a diaper bag
- With your doctor’s plan: compatible with sterile saline and prescribed medicines
As noted above, TruNeb also offers ready-to-use 3% hypertonic saline to pair with your nebulizer. Always follow your pediatrician’s instructions on if and when to use hypertonic saline with your baby.
Learn more about how TruNeb could fit into your family’s routine.
Bottom line: Quiet, portable, and simple to use, TruNeb fits real life with a congested baby.
Frequently Asked Questions
Tap or click a question below to see the answer:
They do different jobs. A humidifier adds moisture to the room for overall comfort. A nebulizer delivers a mist of saline or medicine straight into your baby’s airways. For mild stuffiness, a humidifier and saline nose drops are often enough. If your baby has deeper congestion or wheezing, your pediatrician can add nebulizer treatments.
Yes—when used correctly under medical supervision. Use an infant-sized mask, only sterile saline or prescribed medication, and watch your baby throughout the session. Your pediatrician should guide newborn use.
Only as often as your pediatrician prescribes. Don’t increase dose or frequency on your own. If you think your baby needs treatments more often, call the doctor to review the plan.
The device itself usually doesn’t require a prescription, but medications do. Even for saline, ask your pediatrician how and when to use the nebulizer for an infant.
A saline nebulizer can moisten and loosen nasal mucus, which can make suctioning easier, but it isn’t a decongestant. For a simple stuffy nose, start with saline nose drops and a cool‑mist humidifier. Use a nebulizer only if your pediatrician recommends it as part of care.
Bottom line: Use a humidifier for mild stuffiness and a nebulizer for doctor-guided, targeted relief when your baby has deeper congestion or wheezing.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your baby’s symptoms and before starting, stopping, or changing any nebulizer treatments or medications.