On this page

How Hospitals Use Nebulizer Therapy
Hospitals use nebulizer treatments to get medicine into your lungs quickly when breathing is hard. A nebulizer turns liquid medicine into a fine mist you breathe in through a mask or mouthpiece. It works even if you're scared, coughing, or too weak to use an inhaler correctly. These nebulizer treatments in hospitals are one tool among several treatments your team uses to help ease breathing.
Where it helps most:
- Asthma attacks and sudden wheezing
- COPD flare-ups with tight, heavy breathing
- Serious lung infections like pneumonia with lots of mucus
- Swelling in the airways that needs calming fast
Why hospitals rely on it:
- No special technique needed. You just breathe.
- Multiple medicines can be given together.
- It can be connected to oxygen if your levels are low.
- A respiratory therapist or nurse can monitor you during the dose.
In short: In hospitals, nebulizers can help relieve symptoms quickly without special breathing technique, so the team can act quickly and monitor you safely.
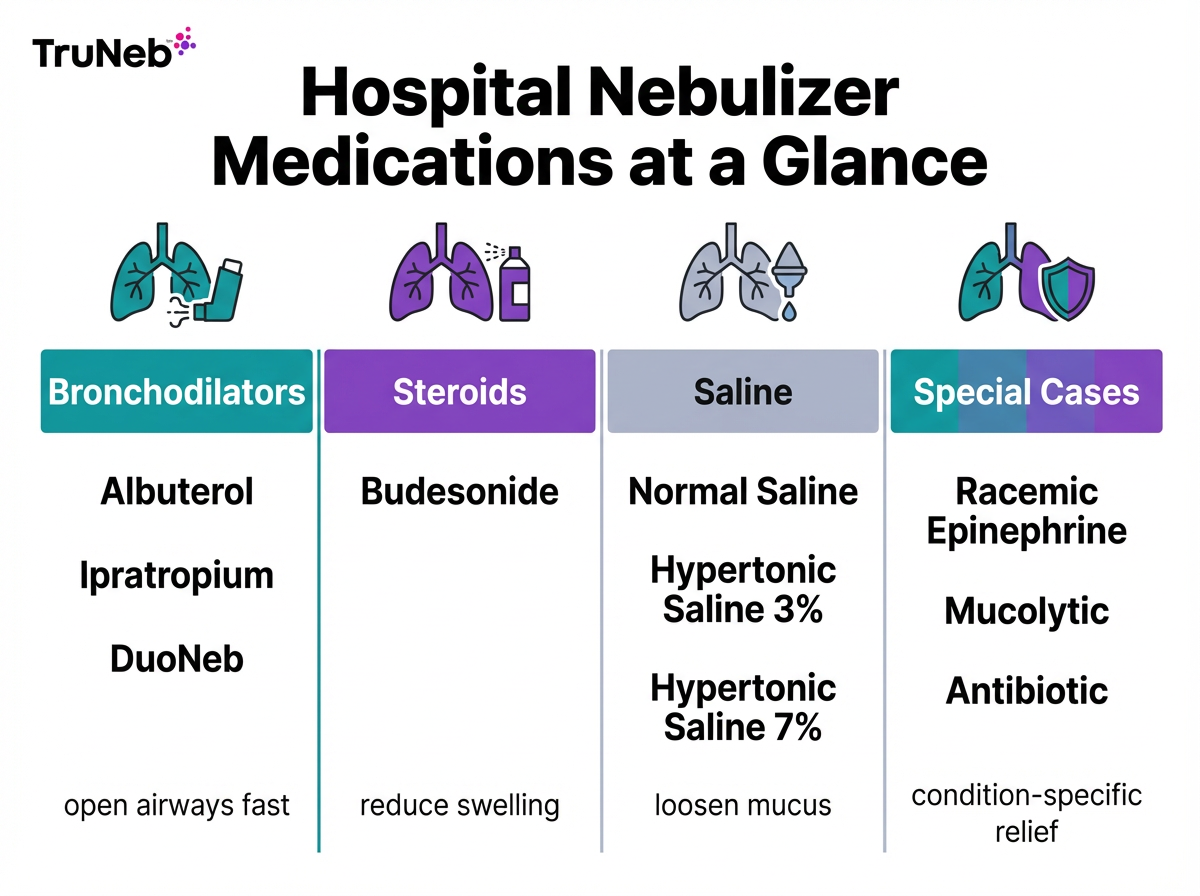
Medications and Treatments Nebulized in Hospitals
Here’s what hospitals commonly put in a nebulizer and why it helps:
Bronchodilators (fast relief)
- Albuterol: relaxes tight airway muscles to ease wheezing and shortness of breath.
- Ipratropium: adds extra bronchodilation; commonly mixed with albuterol.
- DuoNeb: albuterol + ipratropium together for stronger effect in asthma/COPD flares.
Steroids
- Budesonide: calms airway swelling and irritation; sometimes used during more severe episodes.
Saline solutions
- Normal saline: adds moisture and can help thin secretions.
- Hypertonic saline (3% or 7%): draws water into mucus to loosen it; used in hospital settings and some home-care plans for thick mucus in bronchiolitis, cystic fibrosis, or bronchiectasis under provider guidance.
Special cases
- Racemic epinephrine: reduces airway swelling in croup (barky cough with noisy breathing) in children.
- Mucolytics or antibiotics (for select conditions): help break up mucus or treat certain lung infections (e.g., acetylcysteine as a mucolytic; inhaled antibiotics like tobramycin for certain chronic infections).
These medications are chosen and dosed by your hospital team based on your specific condition and medical history.
Always check with your doctor before starting any new nebulizer medication.
In short: Common hospital nebulizer meds include albuterol, ipratropium, budesonide, and saline; each targets tight, swollen, or mucus-filled airways.
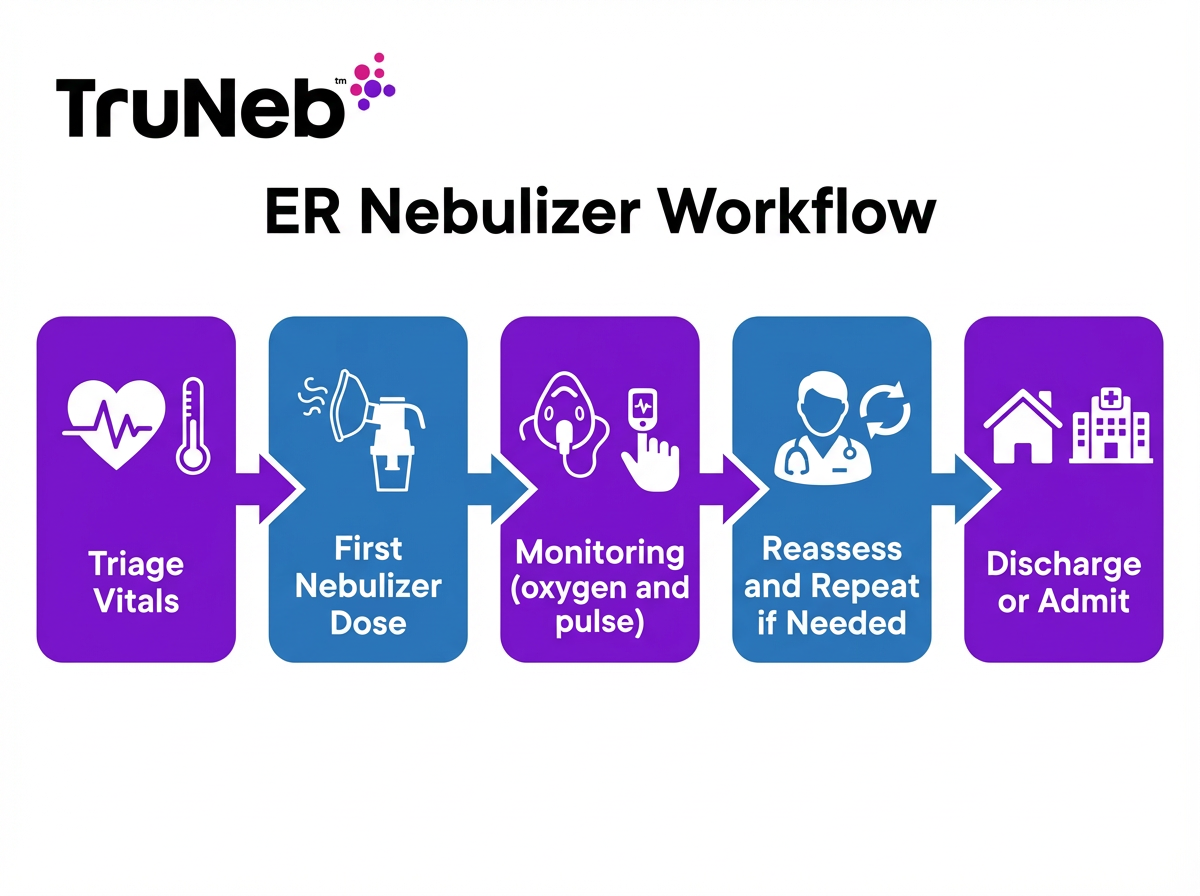
Nebulizer Treatments in the Emergency Room (ER)
In the ER, the team moves fast to help you breathe easier.
If you're short of breath and scared, it helps to know what happens next.
If you arrive with an asthma attack or COPD flare-up, here's what usually happens:
- Quick check: A nurse checks your oxygen level, pulse, and breathing.
- First dose: A nebulizer is usually set up quickly, typically with albuterol or a mix like DuoNeb.
- How to breathe: You sit upright and inhale the cool mist through a mask or mouthpiece for about 5–15 minutes.
- Monitoring: Staff watch your oxygen and heart rate and listen for less wheezing.
- Repeat if needed: If you still struggle, they can repeat the treatment or give additional medicines.
- Next steps: If you improve, you might go home with instructions. If not, you might be admitted for continued care.
Why this works: A nebulizer delivers medicine continuously over several minutes, so you don’t need to time any breaths.
In short: In the ER, a nebulizer usually starts within minutes and typically runs 5–15 minutes while staff track your oxygen and breathing.
Inpatient Nebulizer Therapy and Monitoring
If you're admitted, nebulizer treatments are scheduled and closely watched. Admissions for nebulizer care are common with severe asthma, a COPD flare, or pneumonia.
What to expect on the hospital floor:
- Set schedule: Treatments are usually ordered every 4–6 hours and as needed, based on your doctor's plan.
- Who gives it: A respiratory therapist typically brings the nebulizer to your room, checks your breathing before and after, and updates your nurse and doctor.
- Safety checks: Staff usually track your oxygen level, pulse, and how your lungs sound. They can adjust the plan based on your response.
- Oxygen hookup: If you need oxygen, your nebulizer can be run with it.
- Teaching: As you improve, the team can teach you inhaler or home nebulizer use to prepare you for discharge.
In short: On the hospital floor, respiratory therapists give scheduled treatments and monitor your breathing to guide next steps.
Nebulizer Use in ICU and Critical Care
Even in the ICU, nebulized medicine can be delivered safely.
How it’s given:
- On a ventilator: A nebulizer cup can be placed in the ventilator circuit using a T-piece, so medicine reaches the lungs through the breathing tube.
- Continuous therapy: For very severe asthma, continuous albuterol can be used under close monitoring.
- Monitoring: Heart rhythm, oxygen, and breathing pressures are tracked by the ICU team.
This approach is common in very severe asthma attacks (sometimes called status asthmaticus) or other forms of acute respiratory failure. As patients improve, treatments usually step down from continuous to intermittent, then move toward inhalers or home nebulizers before discharge.
In short: In the ICU, nebulizers can deliver medicine through ventilator circuits or continuously for severe attacks under close monitoring.
Nebulizer Treatments for Pediatric Patients
Kids usually do best with a mask and calm coaching.
Common reasons in children:
- Asthma flare: Albuterol nebulizers relieve wheeze.
- Croup: Racemic epinephrine can reduce swelling and noisy breathing.
- Bronchiolitis (usually RSV): Hypertonic saline can help loosen thick mucus in some cases.
What helps:
- Child-sized masks and simple instructions.
- A parent nearby for comfort.
- Short, frequent checks help catch jitteriness or a faster pulse, and the hospital team adjusts doses by your child's weight.
The goal is the same as for adults: steady breathing, less work, and a safe plan to go home when ready.
In short: In hospitals, kids get child-sized masks, weight-based doses, and calm support to help make nebulizer treatments as safe and comfortable as possible.
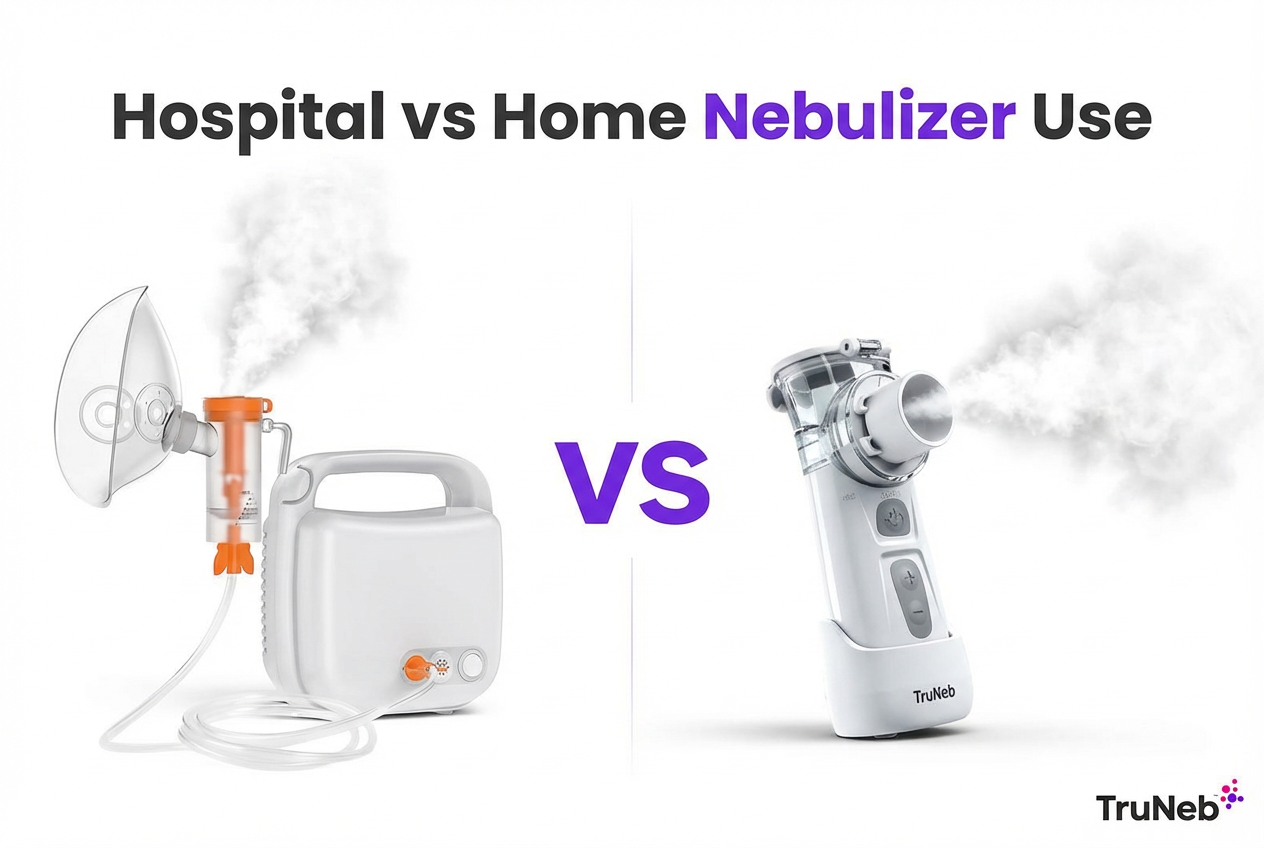
Nebulizer vs Inhaler: How Hospitals Decide
Both deliver medicine to your lungs. The best choice depends on your condition in the moment.
Key points:
- Effectiveness: When used correctly, inhalers with a spacer can work as well as nebulizers. Studies show similar effectiveness when both are used correctly.
- Why choose a nebulizer in the hospital: During distress, many people can’t time breaths or get a good seal. A nebulizer lets you breathe normally. It can also combine medicines and deliver them continuously for several minutes.
- When inhalers make sense: If you’re stable and can use proper technique, an inhaler is fast and portable. Teams usually switch to inhalers before discharge to match what you’ll do at home.
Your care team picks the method that gets medicine into your lungs quickly and safely, then adjusts as you improve.
In short: In a crisis, hospitals usually choose nebulizers for reliability; once stable, inhalers with a spacer can work just as well.
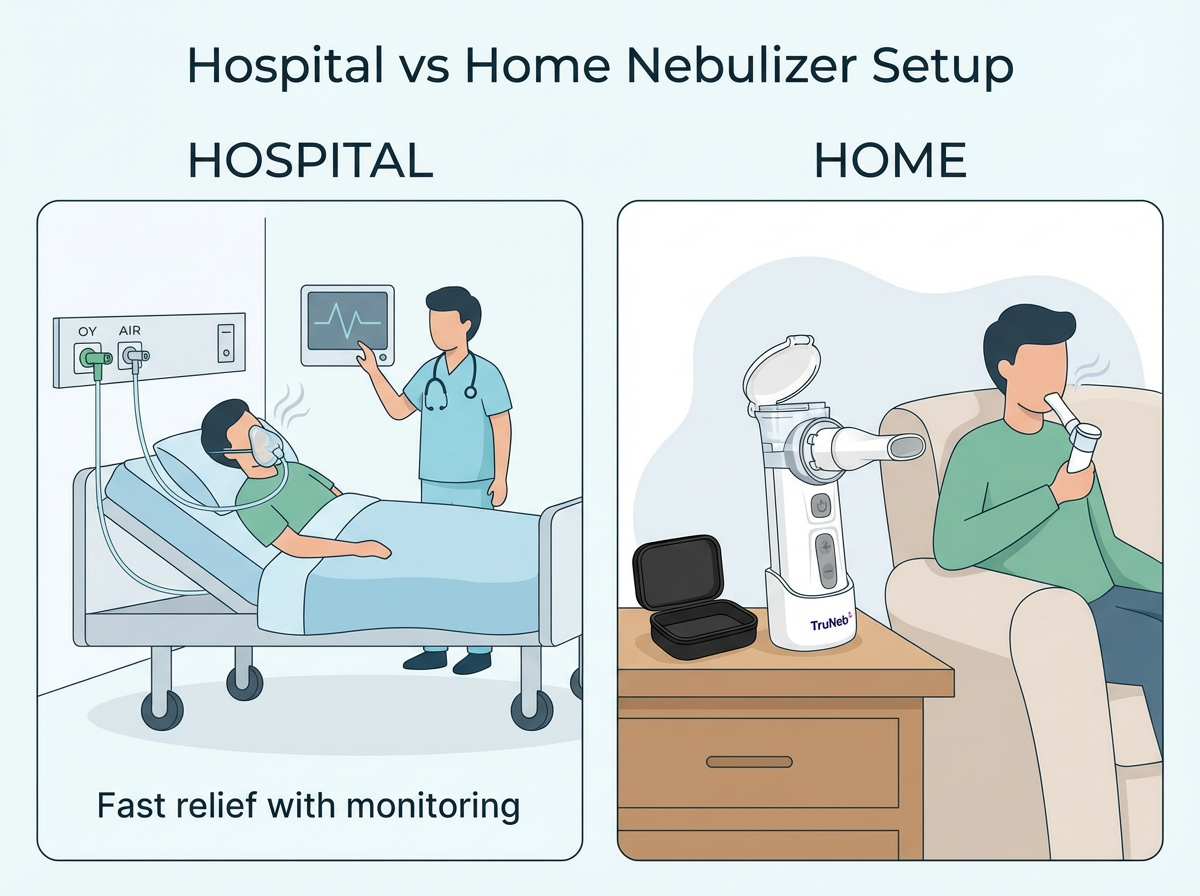
Discharge and Home Care After Hospital Nebulizer Treatments (Continuing Care at Home)
If you still need treatments at home, your team will set you up with the right plan.
Before you leave:
- Device access: You might get a prescription for a home nebulizer. Insurance usually covers it through a medical equipment provider. If you're using insurance, you'll need a prescription for the device. Basic nebulizer machines can also be bought without a prescription if you're paying out of pocket.
- Medications: You’ll receive prescriptions for the vials you need and clear dosing instructions.
- Cleaning basics: You’ll be shown how to rinse parts after each use, air dry, and disinfect on a regular schedule.
At home:
- Keep a routine: Use and clean your nebulizer as instructed. Store supplies in a clean, dry place.
- Portable options: A compact handheld mesh nebulizer can make home and travel treatments simpler and quieter while still delivering a fine mist.
- ⚠️ If you’re shopping for equipment, don’t mix up steam inhalers with nebulizers. Steam inhalers are not meant for breathing prescription medications.
- Follow-up: Check in with your doctor to review your progress. If you’re needing frequent rescue treatments, tell your care team.
Safety note: Talk to your doctor before trying a new nebulizer medication, changing your dose, or changing how often you use your treatments.
⚠️ Get emergency help right away if you have severe trouble breathing, chest pain, blue lips or face, confusion, or if your usual treatments aren’t helping. Call 911 or your local emergency number.
In short: After discharge, a prescription nebulizer, clear cleaning steps, and simple follow-up keep your breathing on track at home.
Frequently Asked Questions
Tap or click a question below to see the answer:
Nebulizers are easier to use during distress. You just breathe the mist, so medicine gets in even if you can’t time breaths or seal an inhaler. Inhalers with a spacer can work just as well when used correctly, and studies show similar effectiveness.
Albuterol is the most common. Hospitals sometimes add ipratropium (the mix is called DuoNeb) during asthma or COPD flares. Depending on your situation, you might also get budesonide (a steroid), hypertonic saline for thick mucus, or racemic epinephrine for croup in kids.
A single dose usually runs about 5–15 minutes, depending on the medicine and device. If you still have trouble after one dose, the team can repeat it or add other treatments.
If you still need treatments, your team can prescribe a home nebulizer and medications. Insurance usually covers the device through a medical equipment provider, and you’ll be shown how to use and clean it.
Hospital setups can run off wall oxygen or larger compressors, which may deliver a dose a bit faster. Modern home mesh and compressor nebulizers are designed to deliver the prescribed dose effectively when used and maintained correctly.
Disclaimer: This article is for informational purposes only and isn’t a substitute for professional medical advice, diagnosis, or treatment. Always talk with your doctor about your symptoms, treatments, and any questions you have about your care.