On this page
Nebulizer Relief for Pneumonia in a Nutshell
A nebulizer is a small machine that turns liquid medicine into a fine mist you breathe into your lungs. With pneumonia, it can make breathing feel easier while your body and medicines fight the infection.
Nebulizer treatment for pneumonia provides symptom relief but doesn’t cure the infection.
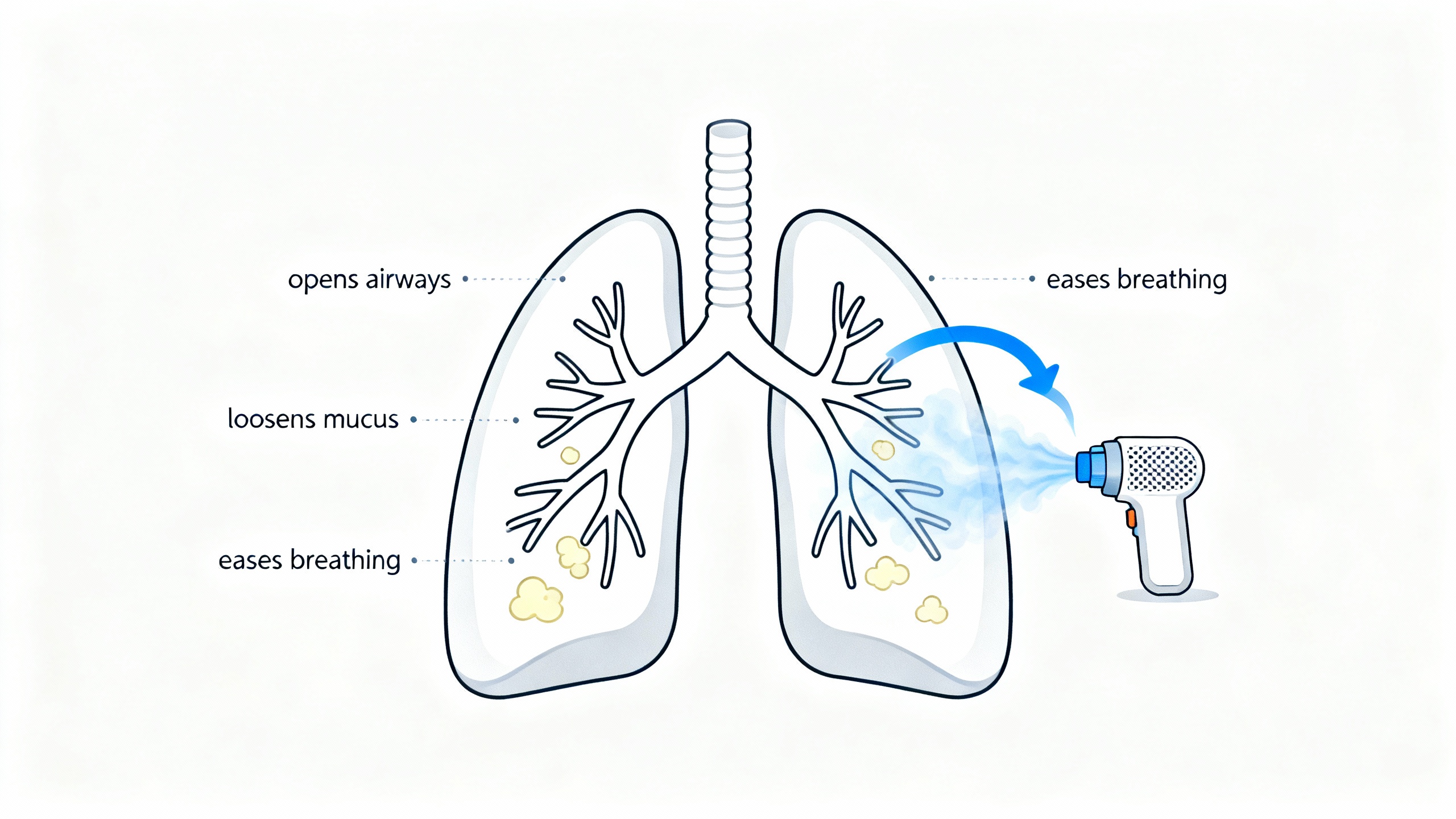
- Opens tight airways: Delivers bronchodilators that relax airway muscles, easing wheeze and chest tightness.
- Loosens mucus: Mist can thin phlegm so it’s easier to cough up.
- Improves comfort: Breathing can feel less strained for a few hours after a treatment.
A nebulizer delivers medication as a mist that can open airways and loosen mucus, easing breathing during pneumonia—though it doesn’t treat the infection itself.
Why Doctors Use Nebulizers for Pneumonia Patients
Not everyone with pneumonia needs a nebulizer. Your doctor might add breathing treatments if you have wheezing, bronchospasm, lots of mucus, or trouble using an inhaler. It’s common in young children, older adults, or people with asthma or COPD on top of pneumonia. The goal is supportive care: help you move air, clear mucus, and stay comfortable while primary treatment (like antibiotics) takes effect.
Doctors use nebulizers when wheezing, bronchospasm, or thick mucus makes it hard to move air or use an inhaler correctly.
Nebulizer vs. Inhaler: Which Helps More in Pneumonia?
| Factor | Nebulizer | Inhaler (MDI + spacer) |
|---|---|---|
| How it delivers | Continuous mist you breathe normally | Metered puffs inhaled deeply via spacer |
| Session time | ~5–10 minutes | Seconds (2–4 puffs) |
| Skill needed | Low—no timing required | Moderate—correct technique matters |
| Best for | Young children; severe shortness of breath; poor inhaler technique | People who can use correct technique; quick on‑the‑go relief |
| Power/portability | Machine; some need outlet; portable mesh units exist | Pocket‑size; no power needed |
| Cleaning | Must clean and disinfect parts | No cleaning beyond mouthpiece |
| Treats infection? | No | No |
Note: When used correctly, an MDI with a spacer can deliver bronchodilators as effectively as a nebulizer (source: American Lung Association).
Medications Delivered via Nebulizer (and How They Help)
There’s no single 'best medicine' for a nebulizer in pneumonia—doctors select the drug based on your symptoms and underlying conditions.
- Bronchodilators (e.g., albuterol): Relax the muscles around the airways to reduce wheeze and tightness. Albuterol can ease wheeze and shortness of breath during pneumonia by opening airways. Some doctors pair albuterol with ipratropium for added airway relief.
- Saline solution (normal or hypertonic): Adds moisture and thins mucus, which can make coughing up phlegm easier.
- Mucolytics (e.g., acetylcysteine): Break down thick secretions. These are used under a doctor’s direction and are sometimes paired with a bronchodilator.
- Nebulized antibiotics (special cases): In some hospital settings (for certain severe or ventilator-associated infections), antibiotics are sometimes nebulized to reach high levels in the lungs. This isn’t typical home care and is managed by doctors.
- Antivirals (rare, specific cases): Certain viral infections are sometimes treated with a nebulized antiviral in the hospital (e.g., ribavirin in specific hospital-managed RSV cases).
- Inhaled corticosteroids (select situations): Are sometimes used if there is significant airway inflammation or asthma-like reactivity (e.g., budesonide in select reactive airway situations). They don’t treat the pneumonia germ itself.
Bronchodilators open tight airways, saline hydrates and thins mucus, and other medicines are used in select cases—none of these cure the infection.
How to Use a Nebulizer Safely When You Have Pneumonia
- Follow your prescription: Use your nebulizer exactly as prescribed by your doctor. Don’t overuse; too much can cause shakiness or a fast heartbeat.
- Follow technique: Use your nebulizer as your doctor showed you and as the device instructions describe. Sitting upright and taking slow, steady breaths can help the medicine reach your lungs.
- Clean after each use: Rinse the cup and mouthpiece/mask. Disinfect per your device’s instructions, then air-dry. This helps prevent germs from growing in the equipment.
- Mind the room: If you’re contagious, do treatments in a well-ventilated space and away from others.
- Know the difference: You might see products labeled 'steam inhaler'—these are not nebulizers and don’t deliver prescription medicines.
- Make it convenient: A portable mesh nebulizer can make treatments easier when you’re tired or away from an outlet. Only use medicines your doctor prescribed for you.
Use the breathing relief window after a treatment to rest, hydrate, and recover.
Use your nebulizer as your doctor showed you, keep the parts clean, and do treatments in a ventilated space if you’re contagious.
Frequently Asked Questions
Tap or click a question below to see the answer:
No. Pneumonia is an infection. A nebulizer only delivers medicines that ease symptoms (like wheeze or cough); antibiotics or antivirals treat the cause.
Yes. Albuterol opens airways and can make coughs more productive and breathing feel easier. It does not treat the infection itself.
Use it only as prescribed. Bronchodilators are often ordered every 4–6 hours for symptoms. Don’t increase frequency on your own; overuse can cause side effects like shakiness or fast heartbeat.
Often yes. The same medicines (like albuterol) can be delivered by an inhaler with a spacer when used correctly. Your doctor will advise which device fits your situation.
Rest, stay well‑hydrated, take your prescribed medicines on schedule, and sleep with your head elevated. Ask your care team about breathing exercises or oxygen if needed.