On this page

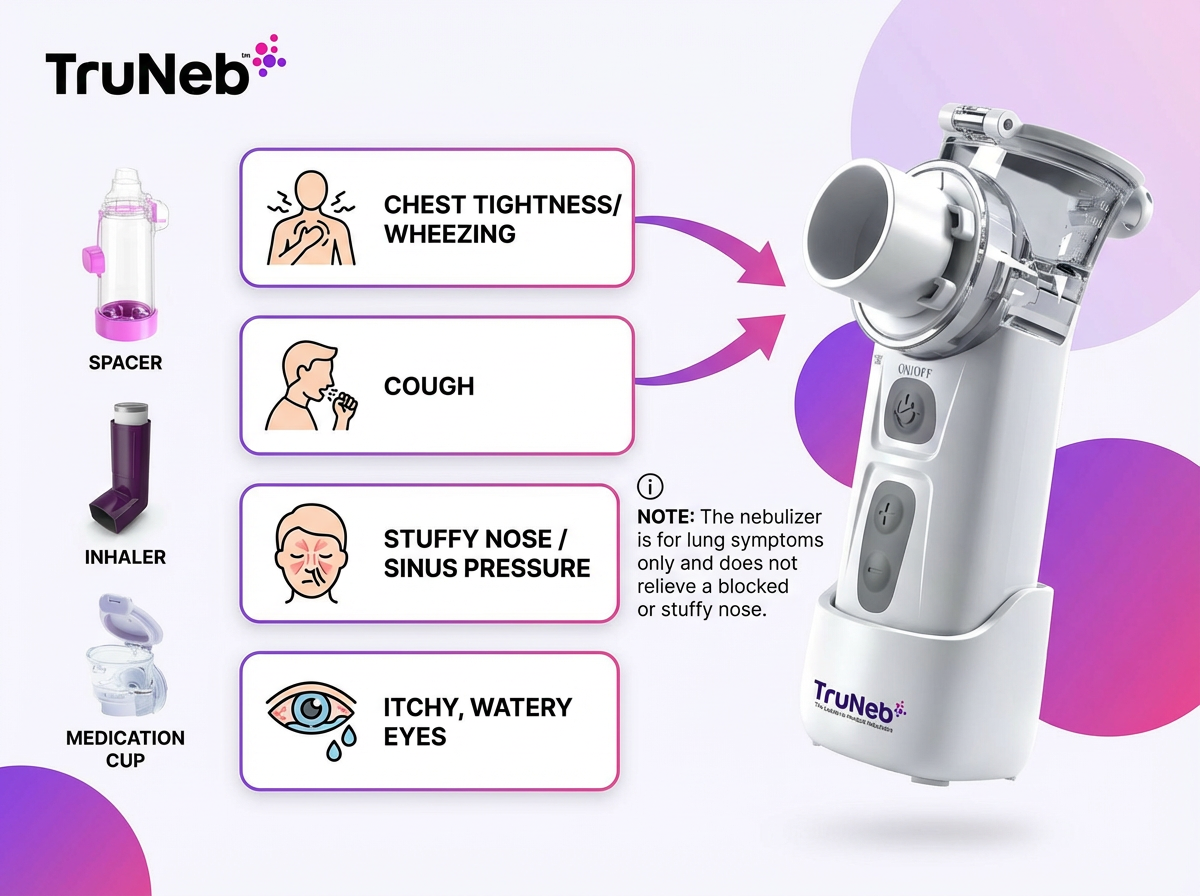
Nebulizer vs. Other Allergy Treatments – Comparing Your Options
Choose the tool that matches your symptom. Here's how a nebulizer for allergies stacks up against other allergy medication alternatives like inhalers, nasal sprays, pills, and allergy shots.
| Option | Works best for | How it delivers | Portability/use | Notes |
|---|---|---|---|---|
| Nebulizer | Chest symptoms (wheeze, tightness) from allergies or asthma | Fine mist you breathe for around 5–10 minutes | Home or portable units, minimal coordination | Helpful during flares or if inhaler technique is hard |
| Inhaler (asthma inhaler) | Quick relief or prevention for chest symptoms | Puffs in seconds with correct technique | Very portable | Technique matters, spacers can help |
| Nasal steroid spray | Nasal congestion, sneezing, runny nose | Acts directly in the nose | Pocket-size | Gold standard for allergic rhinitis |
| Oral antihistamine | Sneezing, runny nose, itchy eyes | Pill that works throughout the body | Very portable | Does not open tight airways |
| Oral decongestant | Temporary nasal congestion | Reduces nasal swelling | Portable | Not for opening airways; use as directed |
| Allergy shots/drops (immunotherapy) | Reducing allergy sensitivity over time | Gradual immune training | Clinic or at-home (depending on type) | Long-term prevention, not fast relief |
Nebulizer vs inhaler for allergies
- Both can deliver the same asthma medicines for allergy-triggered wheeze (for example, albuterol).
- Inhaler: quick puffs in seconds, very portable, needs timing and technique.
- Nebulizer: normal breathing for around 5–10 minutes, no special coordination, can be easier during bad flares or for kids and older adults, helps medicine reach the lungs.
- Tradeoffs: treatments take longer. Older nebulizers with compressors tend to be louder and less portable. Newer portable mesh units improve this.
When to use which
- Mild, occasional wheeze and good inhaler technique: an inhaler is usually enough.
- Frequent flares or trouble with technique: your doctor can add or recommend a nebulizer.
Nebulizer vs nasal spray for allergies
- Nasal steroid sprays are the gold standard for nasal allergy symptoms because they act right where the swelling is.
- A nebulizer cannot replace a nasal spray for a stuffy nose.
Nebulizer vs oral medicines
- Antihistamines help sneezing, runny nose, and itchy eyes. They don't open tight airways.
- Oral decongestants shrink nasal swelling but won't stop bronchospasm. These can complement, not replace, lung treatments.
Nebulizer vs allergy shots (immunotherapy)
- Shots or drops reduce allergy sensitivity over time. They don't give fast relief during an asthma flare.
- A nebulizer is for quick symptom control. Immunotherapy is long-term prevention.
Consumer note: You might see products labeled "steam inhaler" near nebulizers, but they're not the same device and aren't meant for prescription nebulizer medicines.
One-liner: Use nasal sprays for nose symptoms and an inhaler or nebulizer for chest symptoms.
Using Saline Nebulization for Allergies (Congestion & Post-Nasal Drip)
A saline nebulizer uses sterile salt water instead of medication. For some people with allergies, this drug-free option can help with thick mucus and post-nasal drip.
How saline helps
- The fine mist adds moisture and thins mucus so it's easier to clear, helping hydrate your airways.
- It can soothe irritated airway lining that feels dry or scratchy.
Isotonic vs hypertonic
- Isotonic 0.9% saline: gentle hydration, similar to a nasal spray effect delivered as a mist.
- Hypertonic 3% or 7% saline: extra salty, draws water out of swollen tissues and can loosen stubborn mucus. Doctors commonly use hypertonic saline when mucus is very thick and sticky.
About nasal congestion
- You inhale through your mouth, so most mist reaches the lungs and throat. It's not a sinus rinse, so it won't flush your nose like a neti pot, but moisture can reach the back of the nose and ease post-nasal drip.
Product note
- TruNeb™ offers pre-measured sterile 3% and 7% hypertonic saline ampules you can discuss with your doctor.
Safety
- Hypertonic saline can irritate some airways. Your doctor can tell you whether 3% or 7% hypertonic saline, or a milder option, fits your situation and how frequently to use it, if at all.
- You'd use saline nebulization alongside your usual allergy treatments, not instead of nasal sprays or prescribed inhalers.
One-liner: Saline nebulization can thin mucus and soothe airways without using a drug.
Proper Nebulizer Use and Precautions for Allergy Sufferers
Here are general steps most people follow when using a nebulizer; always follow the instructions from your doctor and your device's manual.
- Wash your hands before handling parts.
- Add the prescribed solution to the nebulizer cup (or sterile saline if your doctor advised it).
- Connect tubing and attach the mask or mouthpiece.
- Sit upright, turn the device on, and relax your breathing.
- Breathe slowly through your mouth for the full session, usually around 5–10 minutes, or whatever timing your doctor recommended, until the cup is empty.
- Turn off the machine. Rinse the cup and mask or mouthpiece with warm water and let air-dry. Do a full soap wash daily or as instructed.
Tips for kids
- Use a child-sized mask. Keep them calm with a book or video during the session (usually several minutes).
Safety notes
- Only use medicines prescribed for nebulizer use. Don't pour in essential oils or non-nebulizer drugs. Don't use medications prescribed for someone else, and don't change your prescribed dose without checking with your doctor.
- Bronchodilators can cause brief tremors or a faster heartbeat. If you feel chest pain, severe dizziness, or signs of an allergic reaction (hives, swelling), stop and seek medical care.
- If you use a steroid medicine in your nebulizer, rinse your mouth afterward to lower the risk of thrush.
- Keep parts clean and dry. Store in a dust-free place so you're not breathing in irritants.
- Follow the treatment schedule your doctor gave you. If you need your nebulizer more often than planned, or your symptoms aren't improving, call your doctor to review your allergy or asthma action plan.
⚠️ If you have severe trouble breathing, chest pain, blue lips or face, or can't speak in full sentences, call 911 or seek emergency medical care right away. Don't rely on a home nebulizer alone.
One-liner: Using the right solution, breathing steadily, and keeping parts clean can make nebulizer treatments work better and feel safer.
Choosing the Best Nebulizer for Allergy Relief
Not all nebulizers are the same. Picking the right one makes daily use easier during allergy season.
What to look for
- Portability: a compact portable nebulizer, usually a mesh nebulizer, you can use at home, in the car, or on the sideline.
- Quiet operation: helpful for kids and for bedtime treatments. Traditional compressor nebulizers are bulkier and louder, while portable mesh nebulizers are smaller and quieter.
- Treatment speed: faster delivery (around 5–10 minutes) helps busy routines.
- Easy cleaning: simple parts you can rinse and dry quickly.
- Power: rechargeable battery or USB charging for on-the-go use. Plug-in is fine for bedside use.
- Fit: adult and child-sized masks or a mouthpiece for a good seal.
- Kids: If you're buying for a child, look for a truly child-friendly nebulizer with a small mask, quiet motor, and simple controls.
A portable mesh nebulizer like the TruNeb™ portable mesh nebulizer is quiet, travel-friendly, and kid-ready. Those features make it easier to stick with treatments when pollen is high.
One-liner: Choose a quiet, portable mesh nebulizer you'll actually use, and build the plan with your doctor.
Next Steps – Talk to Your Doctor & Allergy Relief Resources
Allergies are common and often overlap with asthma. If chest symptoms are part of your pattern, ask your clinician where a nebulizer fits in your plan.
Bring these questions:
- Should I use a nebulizer during my allergy season or only during flares as part of my allergy action plan?
- Which solution (medicine or saline) should I use in it, and how often?
- Could hypertonic saline (3% or 7%) be right for me?
Resources:
- ACAAI: Allergy facts and basics.
- CDC: Data on allergy and asthma overlap.
- TruNeb 3% and 7% hypertonic saline and the TruNeb portable mesh nebulizer are available to discuss with your doctor or allergist.
One-liner: Work with your doctor to fit a nebulizer and other tools into an allergy action plan that helps you breathe easier.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice. Always talk to your doctor about your symptoms, treatments, and any questions you have.
Frequently Asked Questions
Tap or click a question below to see the answer:
Short answer: no. For nasal allergy symptoms like a stuffy or runny nose and sneezing from hay fever (allergic rhinitis), a nebulizer is not a primary treatment. If you're wondering about using a nebulizer for allergic rhinitis, it's not the main tool for nose symptoms. A nebulizer's mist goes into your lungs through your mouth, so it doesn't target the nose well.
What helps the nose: intranasal steroid sprays, antihistamine pills, and saline nasal rinses that act directly in the nose. There's evidence that nasal saline rinsing can ease allergic rhinitis.
A rare exception: your doctor might suggest nebulized saline to add moisture and thin mucus. That can soothe the back of the nose and throat and may help post-nasal drip. But it's a supportive add-on, not a replacement for nose-focused therapy.
Nebulizers help lung symptoms; they don't clear a stuffy nose.